·Letter
to the Editor·
Full-thickness
scleral incisions technique for the treatment of a cyclodialysis cleft
following ab interno trabeculotomy
Daniela
Alvarez-Ascencio, Jesus Jimenez-Roman, Rafael Castañeda-Diez, Gabriel
Lazcano-Gomez
Glaucoma Department, Asociación Para Evitar la
Ceguera en México, IAP. Vicente García Torres 46, Coyoacán, Barrio San Lucas,
Correspondence to: Daniela Alvarez-Ascencio. Alfredo de Musset 310-208,
Polanco, Miguel Hidalgo,
Received:
DOI:10.18240/ijo.2019.10.23
Citation: Alvarez-Ascencio D, Jimenez-Roman J, Castañeda-Diez R, Lazcano-Gomez G.
Full-thickness scleral incisions technique for the treatment of a cyclodialysis
cleft following ab interno trabeculotomy. Int J Ophthalmol
2019;12(10):1662-1665
Dear Editor,
I am Dr. Daniela Alvarez-Ascencio from the Glaucoma
Department at Asociacion Para Evitar la Ceguera (APEC) in
MIGS has contributed to the current revolution in
glaucoma surgery and the new therapeutic algorithms to treat glaucoma patients.
Before MIGS, surgical treatment for glaucoma was indicated when conservative
management with topical medications, or laser failed to control intraocular
pressure (IOP). Today, MIGS include a wide group of surgical procedures that
have filled the gap between conservative treatment and traditional surgery for
patients with mild to moderate glaucoma to achieve a target pressure that may
decrease the rate of progression of the disease[1].
MIGS can be performed with an ab externo or ab
interno approach, and as a standalone or combined procedure with cataract
surgery. Although these procedures are considered to have a better safety
profile than traditional glaucoma surgical procedures[2],
several complications including hyphema, migration of device, and cyclodialysis
cleft (CC); leading to hypotony and pthisis bulbi have been described[3-4].
A CC is defined as the separation of the longitudinal
ciliary muscle fibers from the scleral spur (SS), usually as a result of ocular
trauma or anterior segment surgery[5]. The
presence of this cleft creates an abnormal pathway for aqueous humor (AH) to
drain into the suprachoroidal space. Many complications, leading to diminished
visual acuity (VA) and/or risk of phthisis bulbi, have been related
with CC including: hypotony, choroidal effusion, maculopathy, retinal and
choroidal folds, optic nerve swelling, and cataract formation[6-7].
The diagnosis of CC can be achieved by directly
visualizing the presence of an abnormal separation between the SS and the
ciliary muscle by gonioscopy[8]. Ultrasound
biomicroscopy (UBM), anterior segment optical coherence tomography (AS-OCT),
and magnetic resonance imaging (MRI) have been described as complimentary
technologies to establish the extent and location of the CC with a more
objective and accurate method. Evaluation and follow-up after laser or surgical
treatment can also be achieved with these technologies.
The final goal of CC treatment is to restore normal
IOP and to avoid complications. Different therapeutic pathways have been
reported to successfully treat CC based on the extent and length of time of the
anatomical defect. A conservative management, with topical cycloplegics and
steroids, has been recommended by many authors for CC of less than 90° or less
than 6wk[9]; however, some authors disagree about
the usefulness of topical steroids arguing that a decrease of intraocular
inflammation may affect the adhesion of the ciliary body (CB) to the sclera[10].
For clefts larger than 100°-120° with more than 3mo
with no response to conservative management, different therapeutic options
including laser procedures (Argon, Nd:YAG, and diode), cryotheraphy, and gas tamponade
have been reported to be successful when treating this type of patients with
very variable success rates[10-12].
Direct and indirect surgical cyclopexy has been reported to have good
visual prognosis and IOP control, although they can be complex procedures for
unexperienced surgeons[13]. We report
a full-thickness scleral incisions surgical technique for the treatment of a CC
secondary to cataract extraction, combined with an ab interno trabeculotomy
with Trabectome® (NeoMedix, Inc., CA,
CASE PRESENTATION
A 59-year-old woman with diagnosis of high myopia
(sph -7.00 D) and pseudoexfoliation glaucoma (PXG) underwent
phacoemulsification surgery with intraocular lens implantation and ab interno
trabeculotomy with Trabectome (NeoMedix, Inc.) in the left eye (OS). The ab
interno trabeculotomy was performed in the inferior trabecular meshwork through
the supero-nasal phaco incision. On the early postoperatory period, the patient
was managed with acetate prednisolone 1% q.i.d. tapered over a month,
and gatifloxacin q.i.d. for 10d. Visual acuity (VA) of 20/40 and
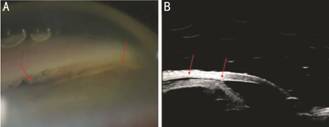
Figure 1 CC and choroidal detachment in OS A: Gonioscipic view of CC; B: UBM of CC and choroidal
detachment.
The CC was managed conservatively, with atropine 1% t.i.d.,
and acetate prednisolone 1% b.i.d., tapered to q.d. over two
months. After lack of response to medical treatment, with no improvement in IOP
or VA, argon laser cleft photocoagulation was attempted without success. Four
months after surgery, the best corrected visual acuity (BCVA) continued
decreasing to 20/400, IOP fluctuated between 2
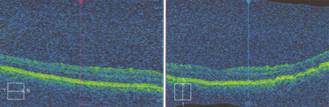
Figure 2 Macular OCT demonstrating macular folds.
SURGICAL TECHNIQUE
Surgery was performed using retrobulbar anesthesia
with lidocaine 1% and bupivacaine 0.5%. A superior 7-0 vicryl corneal traction
suture was placed, and a 100° temporal peritomy was performed (Figure 3). An anterior
chamber (AC) paracenthesis with a 15° stab knife was performed in order to
produce direct contact between the ciliary body (CB) and sclera by decreasing
the amount of aqueous humor bypassing from AC to the supraciliary space. At

Figure 3 7-0 vicryl corneal traction suture and 100º
peritomy that comprises the extent of the CC.
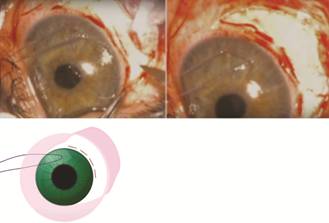
Figure 4 Full thickness scleral incisions at
A 10-0 nylon suture with spatulated needle was used
to achieve a 100° interrupted full thickness (sclera-CB-sclera) running suture
through all the incisions (Figure 5). Conjunctiva was closed using the same
10-0 nylon suture. After surgery, atropine 1% t.i.d. and acetate
prednisolone 1% t.i.d. were prescribed for 2wk.
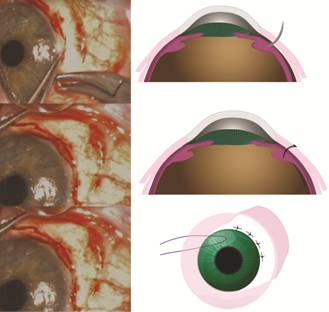
Figure
RESULTS
IOP at day 1 and week 1 were
Follow-up at month-12, VA remained stable (20/40),
IOP

Figure 6 UBM showing no communication between AC and
supraciliary space.
DISCUSSION
Numerous surgical techniques have been described for
the treatment of traumatic CC with successful results[13];
although, these surgeries are always challenging and carry additional
complexity due to the manipulation
of a hypotonous eye and the increased
risk of hemorrhage due to blind maneuvers that are required with some
techniques[13-14].
Techniques based on partial or full thickness scleral
flaps, have a greater risk of transoperative hypotony, especially in large
clefts, leading to a more difficult surgery with a high risk of bleeding and
procedure failure. On the other side, transscleral and translimbal
techniques are reported to be technically easier than those based on full
thickness scleral flaps. Blind maneuvers have a high risk of hemorrhage and
damage to intraocular structures, especially in phakic eyes[14].
Different alternative surgical approaches such as
anterior scleral buckling with or without cryotherapy[15-16], ciliary sulcus sutured and/or ab externo
fixed capsular tension ring (CTR)[17], and
placement of a 3-piece IOL in the sulcus[18-19] have been described in previous reports; although,
these techniques require experience with CB surgery.
Direct cyclopexy with full-thickness scleral
incisions we describe in this case, represents an easy and effective surgical
therapy. In our opinion, the perilimbic full-thickness scleral incisions allow
a simple approach with a lower risk of transoperative hypotony, while allowing
direct visualization of the CB. The interrupted full thickness running suture
enables a simpler approach to the detached CB, directly attaching the sclera to
the CB. The characteristics of this technique allows the treatment of all
extensions clefts in phakic or pseudophakic eyes. Long-term follow up outcomes
in this case, demonstrates the efficacy of the surgical technique.
CONCLUSION
Cyclodialysis cleft is a relative infrequent
complication with different clinical presentations; thereby, the preference for
either conservative or surgical treatment remains controversial and lacks
consensus. Hypotony and its subsequent complications, such vision loss and
pthisis bulbi are the most feared complications of CC; thereby, the accurate
diagnosis and successful treatment of these patients is essential for prompt
rehabilitation[20].
Although several treatment options have been
described to be successful, most surgical approaches are complex and carry many
intraoperative and postoperative risks, even for experienced surgeons. We
describe a technique that we the authors consider straightforward, and easier
than previous cyclopexy methods, and can be used in small or large clefts in
phakic or pseudophakic eyes with a decreased risk of complications. Long-term
follow up in this patient has showed that this simplified technique has good
prognosis results in the long run; follow-up of more cases using this technique
is necessary to confirm the effectiveness, safety and repeatability of our
approach.
ACKNOWLEDGEMENTS
Conflicts of Interest: Alvarez-Ascencio D, None; Jimenez-Roman J,
None; Castañeda-Diez R, None; Lazcano-Gomez G, None.
REFERENCES