·Basic Research·
Increased
interleukin-26 expression in proliferative diabetic retinopathy
Peng Wang, Wen-Yan Wang, Xue-Dong Zhang
Department of Ophthalmology, the
First Affiliated Hospital of Chongqing Medical University, Chongqing Key
Laboratory of Ophthalmology, Chongqing Eye Institute, Chongqing 400016, China
Correspondence to: Xue-Dong Zhang. Department of
Ophthalmology, the First Affiliated Hospital of Chongqing Medical University,
No.1 Youyi Road, Yuzhong District, Chongqing 400016, China. zxued@sina.com
Received: 2018-08-20
Accepted: 2019-07-25
Abstract
AIM: To detect the possible role of interleukin (IL)-26 in
diabetic retinopathy (DR) patients.
METHODS: Subjects were divided into diabetes without
retinopathy (DWR) group (n=20), non-proliferative diabetic retinopathy
(NPDR) group (n=20), proliferative diabetic retinopathy (PDR) group (n=20)
and normal control group (n=20). The protein expression of IL-26 in the serum and vitreous fluid were
measured by enzyme-linked immunosorbent assay (ELISA). The mRNA change of IL-26 in peripheral blood mononuclear cells
(PBMCs) was assessed by real-time polymerase chain reaction.
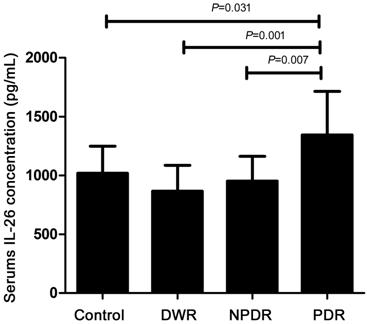
RESULTS: The serum expression of IL-26 in PDR group was significantly elevated
compared with the normal control group, DWR group and NPDR group. The vitreous
fluid concentration of IL-26 in
PDR patients (without anti-VEGF therapy) was also higher compared to normal
controls. However, no obvious significance was found concerning the expression
of IL-26 in
vitreous fluid between PDR after anti-VEGF therapy and normal controls. In PDR
group, the mRNA level of IL-26 significantly increased compared with the normal
controls and DWR patients in the
PBMCs.
CONCLUSION: Protein and mRNA expression of IL-26 are increased
in serum, vitreous fluid and PBMCs in PDR patients, suggesting that IL-26 may
be associated with the pathogenesis of PDR.
KEYWORDS: interleukin-26; serum; vitreous
fluid; peripheral blood mononuclear cells; proliferative diabetic retinopathy
DOI:10.18240/ijo.2019.11.04
Citation: Wang
P, Wang WY, Zhang XD. Increased interleukin-26 expression in proliferative
diabetic retinopathy. Int J Ophthalmol 2019;12(11):1688-1692
INTRODUCTION
Diabetic retinopathy (DR), related
to inadequate glycemic control among diabetes patients, has become a usual
sight-threatening disease[1]. It has been reported
that increased polyol pathway, oxidative stress, advanced glycation
end-products (AGEs), the renin-angiotensin-aldosterone system (RAAS) and
inflammation contributed to the occurrence and development of DR[2-6]. Recently, there is plenty of
evidence suggesting that low-grade inflammation and immune responses play
critical roles in DR[6].
Th17 cells, differentiated from CD4+
T-helper cells[7], are pivotal in the pathogenesis
of autoimmune diseases and produce inflammatory cytokines in coordination with
special cells into the target organ to induce tissue inflammation. Recent
studies have focused on the role of Th17 cells and related inflammatory
cytokines [interleukin (IL)-17A,
IL-17F, IL-21, IL-22] in DR. It
has been reported that disturbances in Th17 cells and IL-17, IL-22 in serum and peripheral blood mononuclear
cells (PBMCs) are possibly associated with DR[8-9]. Takeuchi et al[10]
demonstrated that IL-17A, IL-17F, IL-21, IL-22 were overexpressed in
vitreous fluid of proliferative diabetic retinopathy (PDR) patients.
IL-26, another cytokine produced by
Th17 cells, is a part of the IL-10 cytokine family, which includes IL-19,
IL-20, IL-22, IL-24 and type III interferons (IFN-λ), namely IL-28A, IL-28B and IL-29[11-13]. After it has been secreted, IL-26 binds to special
receptor complex, constituted by IL-20R1/IL-10R2, and induces the secretion of inflammatory
cytokines, including IL-1β, IL-8, tumor necrosis factor (TNF)-α and
granulocyte-macrophage colony-stimulating factor, through activating STAT3 and
STAT1 signaling[14]. Besides, IL-26 can bind to
extracellular DNA and generate the secretion of IL-6 and IL-1β by human
monocytes in a stimulator of IFN genes- and inflammasome-dependent manner[15]. It has been reported that IL-26 participate in the
onset and development of multiple chronic inflammatory and autoimmune-related
diseases, such as rheumatoid arthritis, chronic graft-versus-host disease,
inflammatory bowel disease and chronic hepatitis C virus (HCV), and increased
concentration of IL-26 could be detected[7,16-18]. However, there is no study about the effect of IL-26 in DR. Therefore, we explored whether
IL-26 was associated with the development of DR.
SUBJECTS AND METHODS
Ethical Approval This study got the approvement by
the Clinical Ethical Research Committee of the First Affiliated Hospital of
Chongqing Medical University. All procedures referred to the tenets of Helsinki
declaration and informed consents were signed from patients.
Subjects Sixty type 2 diabetes mellitus (T2DM)
patients (31 men and 29 women, average age =59y) were recruited in this study.
Patients were divided into three groups: group 1, T2DM patients without DR
(DWR, n=20); group 2, T2DM patients with non-proliferative diabetic
retinopathy (NPDR, n=20); group 3, T2DM patients with PDR (n=20).
The above division was based on the international classification standard of DR
according to fundus photography and fluorescein angiography. Normal controls (n=20,
including 11 men and 9 women, mean age =60y) were recruited. The patients who
had a chronic systemic disease (such as hematological or autoimmune disease),
dialysis, cancer, ocular disorders or previous intraocular surgery were
excluded. Serum was gained from blood samples after centrifugation and stored
at -80°C. The PBMCs were
segregated from heparinized blood by Ficoll-Hypaque density-gradient
centrifugation. Vitreous body was extracted by 1 mL needle inserted into
vitreous cavity via manual suction from PDR patients (n=20)
before anti-vascular endothelial growth factor (VEGF) treatment or a pars plana
vitrectomy after anti-VEGF treatment. As getting vitreous via manual
suction was difficult, most samples were obtained by a pars plana vitrectomy
after anti-VEGF therapy (n=14). Twenty patients who were diagnosed with
idiopathic macular epiretinal membrane (IMEM, n=8), idiopathic macula
hole (MH, n=12) and had undergone vitrectomy were recruited as the
control group. Subjects with diabetes, hypertension, hematological disease, or
renal insufficiency with dialysis were excluded. Vitrectomy samples were
reserved at -80°C after
centrifugation. The control group was matched for age and gender with the
diabetes mellitus patients.
Enzyme-Linked Immunosorbent Assay The concentration of IL-26 in the serum and vitreous from DWR, NPDR,
PDR patients and normal controls were measured by human ELISA kits (Yuanye,
China) followed the manufacturer’s instructions. A microplate reader (Molecular
Devices, Sunnyvale, CA, USA) was applied to read the absorbance at 450 nm. The
minimum detectable concentrations by this assay was 10 pg/mL.
Real-time Quantitative RT-PCR RNA was abstracted from the PBMCs
with Trizol Reagent (Takara, Japan) complied with the manufacturer’s instruction.
cDNA was synthesized using Superscript III Reverse Transcriptase (Takara,
Japan) and then the synthesized first-strand of cDNA was measured by real-time
quantitative PCR analysis with SYBR Green labeling method. Quantitative PCR was
conducted by an Applied Biosystems 7500 Fast Real-Time PCR System (Foster City,
CA). To investigate IL-26 expression, we used the following primer sequences:
β-actin, forward 5’-AGG GAA
ATC GTG CGT GAC-3’, reverse 5’-CGC TCA TTG CCG ATA GTG-3’; human IL-26, forward 5’-CAATTGCAAGGCTGCAAGAA-3’, reverse 5’-TCTCTAGCTGATGAAGCACAGGAA-3’.
The real-time PCR reaction was followed by the guidelines of the SYBRH Premix
Ex TaqTM kit (Takara, Japan). The relative gene expression of IL-26 were
performed by the 2-ΔΔCT method for analyses.
Statistical Analysis Statistical analysis was carried out
using SPSS 19.0. Graphs were made by Prism version 5 (GraphPad Software Inc.,
La Jolla, CA, USA). All data were presented as mean±standard deviation (SD).
Statistical comparisons among the normal control group, DWR group, NPDR group
and PDR group about serum and mRNA concertration were performed using one-way
analysis of variance (ANOVA) followed by the Student-Newman-Keuls (SNK) test.
Data for the vitreous fluid level of IL-26 was analyzed using independent
samples t-test after performing the Kolmogorov-Smirnov test. P<0.05
was thought to be reached the statistical significance.
RESULTS
Clinical Characteristic of all
Participants As Table 1 showed, there were no
significant difference was found referring to age, gender and blood pressure
between all participants. Fasting plasma glucose (FPG) and HbA1c of diabetes patients were higher compared
with normal controls.
Table 1 Clinical and laboratory
features of the PDR patient and the control groups n=20
|
Parameters
|
Controls
|
DWR
|
NPDR
|
PDR
|
P
|
|
Gender (M/F)
|
11/9
|
13/7
|
8/12
|
10/10
|
|
|
Age (y)
|
60±10
|
65±11
|
57±10
|
56±9
|
0.056
|
|
Systolic BP (mm Hg)
|
125±14
|
135±12
|
132±25
|
134±15
|
0.388
|
|
Diastolic BP (mm Hg)
|
75±7
|
81±9
|
78±9
|
80±9
|
0.266
|
|
HbA1c (%)
|
5.4±0.27
|
7.0±1.4
|
7.9±1.2
|
8.6±1.5
|
<0.001
|
|
FPG (mmol/L)
|
5.17±0.17
|
8.32±0.37
|
9.12±0.91
|
10.01±1.29
|
<0.001
|
|
No. of patients receiving
anti-VEGF (after/before vitreous sampling)
|
|
|
|
14/6
|
|
BP: Blood pressure; FPG: Fasting
plasmaglucose; DWR: Diabetic without retinopathy; NPDR: Non-proliferative
diabetic retinopathy; PDR: Proliferative diabetic retinopathy.
Increased Protein Expression of IL-26 in Serum and Vitreous Fluid of PDR
Patients As Table 2 showed, serum
concentration of IL-26 in PDR
patients was 1343.75±370.41 pg/mL, which was significantly increased compared
with the normal controls (P=0.031), DWR (P=0.01) and NPDR
patients (P=0.007, Figure 1). However, there wasn’t any difference found
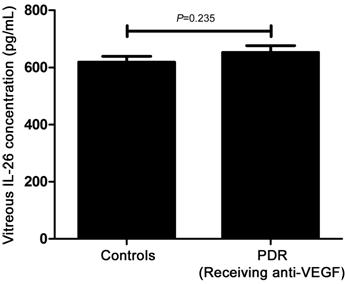
among healthy controls, DWR and NPDR patients in this study. Furthermore, we
also explored the protein concentration of IL-26
in vitreous fluid. Just as shown in Table 3, as many patients
had been received anti-VEGF treatment, to exclude the influence of anti-VEGF
drugs on the expression of IL-26, we respectively compared the patients who had
received anti-VEGF treatment (n=14) and did not have anti-VEGF treatment
(n=6) with the controls. We found that the concentration of IL-26 in vitreous body from PDR patients
without receiving anti-VEGF therapy was remarkably elevated as compared to
healthy controls (P=0.04, Figure 2). However, the statistical difference
could not be found between the patients who had received anti-VEGF treatment
and the controls (P=0.235, Figure 3).
Table 2 Serum concentrations of
IL-26
n=20
|
Serum concentration
|
Controls
|
DWR
|
NPDR
|
PDR
|
|
IL-26 (pg/mL)
|
1017.86
|
865.95
|
951.31
|
1343.75
|
|
Range
|
762.50-1498.5a
|
553.00-1288.50c
|
567.50-1251.00b
|
908.00-2411.50
|
Dunnett test, LSD test, SNK t-test
were performed to analyze differences between groups. aP<0.05,
bP<0.01, cP<0.001.
Table 3 Vitreous concentrations of
IL-26
|
Vitreous concentration
|
Controls,
n=20
|
PDR
|
|
Without anti-VEGF, n=6
|
Receiving anti-VEGF, n=14
|
|
IL-26 (pg/mL)
|
618.69
|
686.00a
|
666.85
|
|
Range
|
563.0-645.5
|
618.50-822.50a
|
625.50-681.50
|
Independent samples t-test
were performed to analyze differences between groups. aP<0.05
vs controls.
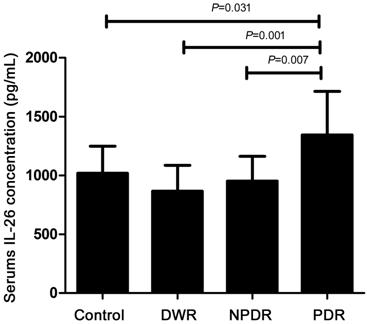
Figure 1 IL-26 protein concentration
in serum in normal controls (n=20), DWR (n=20), NPDR (n=20)
and PDR patients (n=20).

Figure 2 IL-26 protein concentration
in vitreous fluid in normal controls (n=20) and PDR patients (n=6,
without anti-VEGF therapy).
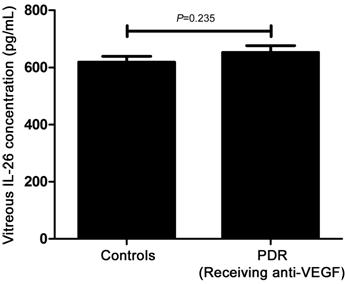
Figure 3 IL-26 protein concentration
in vitreous fluid in normal controls (n=20) and PDR patients (n=14,
receiving anti-VEGF therapy).
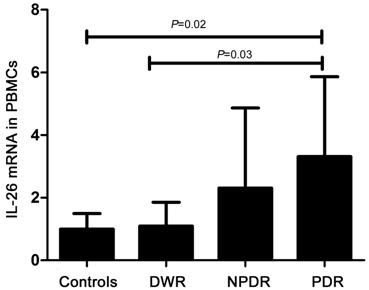
Increased Gene Expression of IL-26 in PBMCs of PDR Patients We further assayed the concertration
of IL-26 mRNA in PBMCs (Figure 4). The IL-26 mRNA expression in PDR patients
was remarkablely increased than that in healthy controls and DWR patients (P<0.05).
However, no obivious difference was observed among the normal controls, DWR and
NPDR patients, or between the NPDR patients and PDR patients.
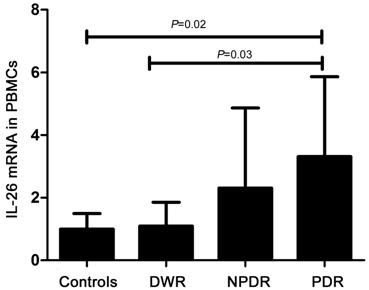
Figure 4 IL-26 mRNA expression in
PBMCs from healthy controls (n=20), DWR (n=20), NPDR (n=20)
and PDR patients (n=20).
DISCUSSION
Our study showed that PDR patients
had an increased expression of IL-26 in
serum and PBMCs. In the meantime, we also found that IL-26 protein expression in
vitreous fluid from PDR patients without receiving intravitreal anti-VEGF
therapy significantly elevated. These data mentioned above indicate that the
increased expression of IL-26 may contribute to the pathogenesis of PDR.
Our study displayed an increased
protein level of IL-26 in the
serum of PDR patients as compared to normal controls, DWR and NPDR patients.
Our results are in consistent with the previous studies reported in other
autoimmune and chronic inflammatory diseases. Miot et al[17] found that the serum expression of IL-26 in HCV was higher than that in controls,
and chronic HCV infection relates to inflammation. Lopalco et al[19] reported the serum expression of IL-26 in Behçet’s disease (BD) patients with
mucocutaneous manifestations plus ocular involvement was significantly higher
than that in the subgroup with only mucocutaneous involvement. Collectively,
these results certify that IL-26 is involved in the pathogenesis of various
autoimmune and chronic inflammatory disorders.
Inflammatory cytokines aggregate in
special tissue and form a proinflammatory microenvironment. Furthermore, we
detected the protein concentration of IL-26
in vitreous fluid and found that the concertration of IL-26 was
higher in vitreous fluid of PDR patients without anti-VEGF therapy than that in
normal controls. Our findings agreed with the findings reported by Kaabach et
al[20] and Corvaisier et al[7], which showed IL-26 was highly expressed in the
cerebrospinal fluid of neuro-BD patients and in the synovial fluids in
rheumatoid arthritis patients. Moreover, we found that the concentration of IL-26 in the vitreous fluid was downregulated
after intravitreal injection of anti-VEGF therapy, which indicates that
anti-VEGF therapy may directly inhibit the expression of IL-26. However, it
needs further study to verify the effect of anti-VEGF on the concentration of
IL-26 in vitro
experiments.
Next, we designed an experiment to
measure the gene expression of IL-26 in
PBMCs. We found that there was an elevated expression of IL-26 mRNA in PDR
patients compared with normal controls and DWR patients. This result is in
accordance with the protein expression of IL-26
in serum. However, the exact mechanism about how to regulate
the expression of IL-26 in PBMCs
in DR deserves further investigation.
ACKNOWLEDGEMENTS
Foundation: Supported by the National Natural
Science Foundation of China (No.81870643).
Conflicts of Interest: Wang P, None; Wang WY, None; Zhang
XD, None.
REFERENCES
|
1 Cheung N, Mitchell P, Wong TY. Diabetic retinopathy.
Lancet 2010; 376(9735):124-136.
https://doi.org/10.1016/S0140-6736(09)62124-3
|
|
|
|
2 Lorenzi M. The polyol pathway as a mechanism for
diabetic retinopathy: attractive, elusive, and resilient. Exp Diabetes Res
2007;2007:61038.
https://doi.org/10.1155/2007/61038
PMid:18224243 PMCid:PMC1950230
|
|
|
|
|
3 Ran RJ, Du LP, Zhang XD, Chen XL, Fang YH, Li YY,
Tian HY. Elevated hydrogen sulfide levels in vitreous body and plasma in patients
with proliferative diabetic retinopathy. Retina 2014;34(10):2003-2009.
https://doi.org/10.1097/IAE.0000000000000184
PMid:24743641
|
|
|
|
|
4 Stitt AW, Jenkins AJ, Cooper ME. Advanced glycation
end products and diabetic complications. Expert Opin Investig Drugs
2002;11(9):1205-1223.
https://doi.org/10.1517/13543784.11.9.1205
PMid:12225243
|
|
|
|
|
5 Wilkinson-Berka JL. Angiotensin and diabetic
retinopathy. Int J Biochem Cell Biol 2006;38(5-6):752-765.
https://doi.org/10.1016/j.biocel.2005.08.002
PMid:16165393
|
|
|
|
|
6 Tomić M, Ljubić S, Kastelan S. The role of inflammation and
endothelial dysfunction in the pathogenesis of diabetic retinopathy. Coll
Antropol 2013;37(Suppl 1):51-57.
https://doi.org/10.1155/2013/213130
PMid:24288441 PMCid:PMC3830881
|
|
|
|
|
7 Corvaisier M, Delneste Y, Jeanvoine H, Preisser L,
Blanchard S, Garo E, Hoppe E, Barré B, Audran M, Bouvard B, Saint-André JP,
Jeannin P. IL-26 is overexpressed in rheumatoid arthritis and induces
proinflammatory cytokine production and Th17 cell generation. PLoS Biol
2012;10(9):e1001395.
https://doi.org/10.1371/journal.pbio.1001395
PMid:23055831 PMCid:PMC3463509
|
|
|
|
|
8 Chen H, Ren XR, Liao NY, Wen F. Th17 cell frequency
and IL-17A concentrations in peripheral blood mononuclear cells and vitreous
fluid from patients with diabetic retinopathy. J Int Med Res
2016;44(6):1403-1413.
https://doi.org/10.1177/0300060516672369
PMid:27885039 PMCid:PMC5536736
|
|
|
|
|
9 Chen H, Wen F, Zhang XZ, Su SB. Expression of
T-helper-associated cytokines in patients with type 2 diabetes mellitus with
retinopathy. Mol Vis 2012;18:219-226.
|
|
|
|
|
10 Takeuchi M, Sato T, Tanaka A, Muraoka T, Taguchi M,
Sakurai Y, Karasawa Y, Ito M. Elevated levels of cytokines associated with
Th2 and Th17 cells in vitreous fluid of proliferative diabetic retinopathy
patients. PLoS One 2015;10(9):e0137358.
https://doi.org/10.1371/journal.pone.0137358
PMid:26352837 PMCid:PMC4564282
|
|
|
|
|
11 Fickenscher H, Hör S, Küpers H, Knappe A, Wittmann
S, Sticht H. The interleukin-10 family of cytokines. Trends Immunol
2002;23(2):89-96.
https://doi.org/10.1016/S1471-4906(01)02149-4
|
|
|
|
|
12 Ouyang W, Rutz S, Crellin NK, Valdez PA, Hymowitz
SG. Regulation and functions of the IL-10 family of cytokines in inflammation
and disease. Annu Rev Immunol 2011;29:71-109.
https://doi.org/10.1146/annurev-immunol-031210-101312
PMid:21166540
|
|
|
|
|
13 Sabat R. IL-10 family of cytokines. Cytokine Growth
Factor Rev 2010;21(5):315-324.
https://doi.org/10.1016/j.cytogfr.2010.11.001
PMid:21112807
|
|
|
|
|
14 You W, Tang QY, Zhang CY, Wu JD, Gu CR, Wu ZS, Li
XC. IL-26 promotes the proliferation and survival of human gastric cancer
cells by regulating the balance of STAT1 and STAT3 activation. PLoS One
2013;8(5):e63588.
https://doi.org/10.1371/journal.pone.0063588
PMid:23704922 PMCid:PMC3660585
|
|
|
|
|
15 Poli C, Augusto JF, Dauvé J, Adam C, Preisser L, Larochette
V, Pignon P, Savina A, Blanchard S, Subra JF, Chevailler A, Procaccio V,
Croué A, Créminon C, Morel A, Delneste Y, Fickenscher H, Jeannin P. IL-26
confers proinflammatory properties to extracellular DNA. J Immunol
2017;198(9):3650-3661.
https://doi.org/10.4049/jimmunol.1600594
PMid:28356384
|
|
|
|
|
16 Dambacher J, Beigel F, Zitzmann K, De Toni EN, Göke
B, Diepolder HM, Auernhammer CJ, Brand S. The role of the novel Th17 cytokine
IL-26 in intestinal inflammation. Gut 2009;58(9):1207-1217.
https://doi.org/10.1136/gut.2007.130112
PMid:18483078
|
|
|
|
|
17 Miot C, Beaumont E, Duluc D, et al. IL-26 is overexpressed
in chronically HCV-infected patients and enhances TRAIL-mediated cytotoxicity
and interferon production by human NK cells. Gut 2015; 64(9):1466-1475.
https://doi.org/10.1136/gutjnl-2013-306604
PMid:25183206
|
|
|
|
|
18 Ohnuma K, Hatano R, Aune TM, Otsuka H, Iwata S, Dang
NH, Yamada T, Morimoto C. Regulation of pulmonary graft-versus-host disease
by IL-26+CD26+CD4 T lymphocytes. J Immunol 2015;194(8):3697-3712.
https://doi.org/10.4049/jimmunol.1402785
PMid:25786689 PMCid:PMC4568737
|
|
|
|
|
19 Lopalco G, Lucherini OM, Lopalco A, Venerito V, Fabiani
C, Frediani B, Galeazzi M, Lapadula G, Cantarini L, Iannone F. Cytokine
signatures in mucocutaneous and ocular behçet's disease. Front Immunol
2017;8:200.
https://doi.org/10.3389/fimmu.2017.00200
PMid:28289419 PMCid:PMC5327443
|
|
|
|
|
20 Kaabachi W, Bouali E, Berraïes A, Dhifallh IB, Hamdi
B, Hamzaoui K, Hamzaoui A. Interleukin-26 is overexpressed in Behçet's
disease and enhances Th17 related -cytokines. Immunol Lett 2017;190:177-184.
https://doi.org/10.1016/j.imlet.2017.08.008
PMid:28811236
|
|