·Clinical Research·
Trocar
opening: silicone oil removal with phacoemulsification and intraocular lens
implantation
Xu
Zhang, Ya-Jie Pan, Zheng-Yu Song
Department of Ophthalmology,
Correspondence to: Zheng-Yu Song. Department of Ophthalmology, Shanghai
Shuguang Hospital, Shanghai University of Traditional Chinese Medicine, No.185
Avenue of Pu’an, Huangpu District, Shanghai 200021, China. rockersong@126.com
Received:
Abstract
AIM: To evaluate the efficacy and safety of a
modified technique [trocar opening (TO)] for silicone oil removal (SOR) in
combination with phacoemulsification and intraocular lens (IOL) implantation.
METHODS: A total of 60 eyes of 60 patients with cataract
and silicone oil-filled eyes were enrolled in this study. The patients were
divided into two groups: the patients in the control group underwent 23-gauge
pars plana active SOR surgery with phacoemulsification
and IOL implantation, while the patients in the TO group underwent TO methods
during surgery. Best corrected visual acuity (BCVA), surgery time, intraocular
pressure, and operative complications were observed 6mo after surgery.
RESULTS: There was no significant difference between the
two groups in terms of age, gender, preoperative, intraocular pressure, or time
of silicone oil stay. Prior to surgery, the mean BCVA for the control and TO
groups was 1.34±0.44 and 1.36±0.42. At 6mo following surgery, the mean BCVA
improved to 0.74±0.36 and 0.77±0.32, respectively (P<0.001). There
was no significant difference between the two groups. The mean SOR time was
6.9±2.3min and 4.8±1.2min in the control and TO groups (P=0.008). The
total operation time was 28.2±8.5min and 24.6±6.4min, respectively (P=0.035).
Posterior capsule rupture occurred in four eyes of control and none of TO group
(P<0.01). Late recurrent retinal detachment occurred in one eye in
the control group (2mo after surgery) and in one eye in the TO group (4mo after
surgery).
CONCLUSION: TO is a simple, effective, time-saving, and
safe method for SOR combined with phacoemulsification and IOL implantation.
KEYWORDS: intraocular
lens implantation; phacoemulsification; posterior capsule rupture; silicone oil
removal
DOI:10.18240/ijo.2019.11.09
Citation: Zhang X, Pan YJ, Song ZY. Trocar opening: silicone oil removal with
phacoemulsification and intraocular lens implantation. Int J Ophthalmol 2019;12(11):1720-1724
INTRODUCTION
Silicone oil filling in the vitreous cavity is a
common method used to withstand the retina and maintain the intraocular
pressure (IOP) in posterior eye surgery (proliferative vitreoretinopathy,
proliferative diabetic retinopathy, giant retinal tears, and ocular trauma)[1]. However, there are several complications caused by
silicone oil tamponade, such as silicone oil emulsification, secondary
glaucoma, cataract, and corneal degeneration[2].
Therefore, it is suggested that the silicone oil should be removed as soon as
its tamponade effect is no longer needed. In addition, it is recommended that a
combined operation with cataract extraction and silicone oil removal (SOR) is
necessary following the occurrence of secondary cataract[3].
Phacoemulsification in a vitrectomized eye is
associated with a higher rate of posterior capsule rupture because of the hard
nucleus[4]. Furthermore, the buoyancy
of the silicone oil may lead to posterior capsule elevation and additional
anterior chamber instability, which increase the risk of posterior capsule
rupture[5]. The incidence of posterior capsule
rupture during phacoemulsification in vitrectomized eyes or combined surgery
has been reported between 1.5% and 10.1%, which is higher than that observed
for normal phacoemulsification[4-6].
Therefore, in SOR combined with phacoemulsification, new approaches are
warranted to reduce the incidence of posterior capsule rupture. Herein, we
report a new method, termed trocar opening (TO), of SOR in combination with
phacoemulsification and intraocular lens (IOL) implantation.
SUBJECTS AND METHODS
Ethical Approval
The study protocol has
been approved by the Institute’s Ethics Committee on human research. This
research adhered to the tenets set forth in the Declaration of Helsinki, and
written informed consent was provided by all patients.
This consecutive case study was conducted from July
2017 to December 2017. A total of 60 patients (60 eyes) were included and
underwent SOR in combination with phacoemulsification and IOL implantation. All
previous 23-gauge (
All patients underwent measurements of keratometry,
anterior chamber depth, and axial length using the IOL Master (IOL Master V1.1;
Carl Zeiss Meditec,
All patients, in which the density of the removed oil
was 5700 cSt, were randomly divided into two groups: control and TO. In the
control group (30 eyes), standard
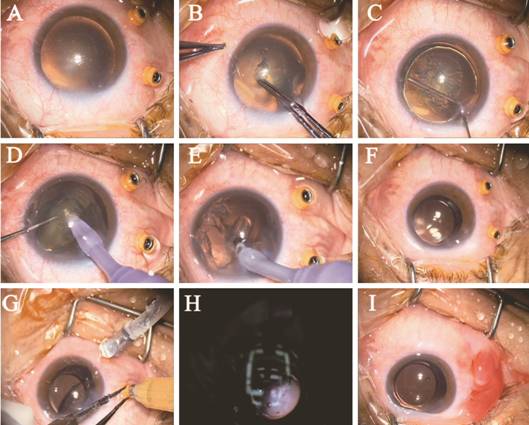
Figure 1 SOR with phacoemulsification and IOL
implantation using the trocar opening method A: Unplugged
microcannula placement in the inferotemporal and superotemporal quadrants
Statistical Analysis In this study, the SPSS software (version 13.0 for
Windows; SPSS Inc.,
RESULTS
A total of 60 patients (60 eyes) were included in our
study. The baseline demographics and characteristics of the patients are
summarized in Table 1. There was no significant difference between the two
groups in terms of age, sex, pre-operative IOP, or time of silicone oil stay.
Table 1 Baseline demographic data and characteristics
of the patients mean±SD
|
Parameters |
Control group |
TO group |
P |
|
Age (y) |
52.2±9.2 |
54.7±8.4 |
0.687 |
|
Sex (male, %) |
46.7 |
53.3 |
0.154 |
|
Right eye (%) |
43.3 |
46.7 |
0.165 |
|
Pre-operative IOP (mm Hg) |
16.7±3.4 |
17.5±3.7 |
0.435 |
|
Time of SO stay (mo) |
5.4±2.4 |
5.8±1.8 |
0.562 |
|
BCVA (logMAR) |
1.34±0.44 |
1.36±0.42 |
0.672 |
TO: Trocar opening; IOP: Intraocular pressure; SO:
Silicone oil; BCVA: Best corrected visual acuity.
Surgery was successfully performed in all patients.
The silicone oil was completely removed from all eyes. In the last follow-up
after surgery, there was no significant residual oil in the anterior chamber or
in the vitreous cavity. There were no serious intraoperative complications,
except the occurrence of posterior capsule rupture in four eyes in the control
group and IOLs were planted in the sulcus, and none in the TO group (P<0.01).
Late recurrent retinal detachment occurred in one eye in the control group (2mo
after surgery) and in one eye in the TO group (4mo after surgery). This was
attributed to proliferative vitreoretinopathy and these patients were
re-operated with pars plana vitrectomy and silicone oil tamponade. There was no
recurrence of retinal detachment observed at the 6-month follow-up. In
addition, there were no other postoperative complications (e.g.,
vitreous hemorrhage, dislocated IOL, or endophthalmitis) observed.
The mean surgical time is summarized in Table 2.
There was significant difference between the two groups. Cataract time was
defined as the interval between making and sealing the cornel incision. SOR
time was defined as the interval between the connection of the infusion tube
and the sealing of the sclera incisions. Total time was defined as the interval
between the patient on and off the operating table.
Table 2 Comparison of mean cataract time, SOR time,
and operation time in the two groups mean±SD, min
|
Parameters |
Control group |
TO group |
P |
|
Cataract time |
8.4±3.2 |
7.2±2.6 |
0.013 |
|
SOR time |
6.9±2.3 |
4.8±1.2 |
0.008 |
|
Operation time |
28.2±8.5 |
24.6±6.4 |
0.035 |
TO: Trocar opening; SOR: Silicone oil removal.
The mean IOP is summarized in Table 3. There was no
significant difference between the two groups, and hypotony did not occur.
Except retinal redetachment, the remaining eyes showed improvement in BCVA at
the last follow-up visit. Prior to surgery, the mean BCVA in the control and TO
group was 1.34±0.44 and 1.36±0.42, respectively. At 6mo after surgery, the mean
BCVA improved to 0.74±0.36 and 0.77±0.32, respectively (P<0.001).
There was no significant difference between the two groups.
Table 3 Comparison of IOP in the two groups
mean±SD, mm Hg
|
Post operation |
Control group |
TO group |
P |
|
1d |
12.6±4.5 |
13.5±4.2 |
0.423 |
|
1wk |
15.4±3.8 |
15.5±4.4 |
0.261 |
|
1mo |
15.1±2.6 |
14.8±3.3 |
0.345 |
|
3mo |
15.5±3.6 |
14.9±4.1 |
0.472 |
|
6mo |
16.2±3.7 |
15.7±3.2 |
0.413 |
TO: Trocar opening.
DISCUSSION
In this study, we reported a novel management
strategy for SOR with phacoemulsification and IOL implantation. The results
demonstrated that the TO method is simple, effective, time-saving, and safe. It
involves only one step i.e., maintaining the microcannulas unplugged
during phacoemulsification and IOL implantation.
There are many methods used for SOR: transpupillary
or pars plana, active or passive,
We introduced a new method of maintaining the TO
during phacoemulsification and IOL plantation to overcome the
buoyancy of the silicone oil. This approach offers two advantages. Firstly, one
could let the silicone oil flow out of the opening trocar instead of directly
elevating the posterior capsule, increasing anterior chamber stability and
decreasing the possibility of posterior capsule rupture. In this study, posterior
capsule rupture did not occur in the TO group, while it occurred in four of 30
eyes (13.3%) in the control group. This incidence was similar to those reported
in other studies[4-6]. Secondly,
this method could decrease the volume of the remaining silicone oil when
initiating SOR, since the silicone oil is flowing out during the entire
phacoemulsification. Thus, it can reduce the time needed for SOR. According to
our results, the cataract time, SOR time, and operation time were shorter in
the TO group versus the control group.
Yildirim et al[12]
reported that the mean removal time through a corneal tunnel incision was
approximately 7.6-9min for passive SOR. The mean time for passive removal of
1000 cSt silicone oil using
The potential disadvantage of sutureless vitrectomy
is postoperative wound leakage. Zafar et al[19]
reported transient hypotony in 7.3% of the examined eyes. Moreover, Song et
al[16] reported that nine of 48 eyes (18.75%)
required additional sutures intraoperatively, while three eyes (6.25%)
developed postoperative hypotony. We sutured all the sclerotomy
sites to prevent postoperative hypotony, and obtained a safe result (no
occurrence of hypotony). The incidence of retinal redetachment after SOR was
reported to be 0.02%-20%[6-7,19-20]. In this study, this incidence
was 4.8% in each group, indicating that this new method did not increase the
incidence of retinal re-detachment. Furthermore, there were no other
postoperative complications (e.g., vitreous hemorrhage, dislocated IOL,
or endophthalmitis) observed. According to these findings, the TO is a safe
method.
The present study was characterized by some
limitations, namely a relatively small sample size and short follow-up time.
Future investigations with larger controlled cases and longer follow-up time
are warranted to validate the efficacy and safety of this technique.
In conclusion, our findings indicated that the TO
method is a simple, effective, time-saving, and safe method for SOR with
phacoemulsification and IOL implantation.
ACKNOWLEDGEMENTS
Foundation: Supported by
Conflicts of Interest: Zhang X, None; Pan YJ, None; Song ZY,
None.
REFERENCES