
·Clinical Research·
Comparison
of contrast sensitivity based on the surgical results for intermittent
exotropia
Hae Rang Kim, Soo Jung Lee
Department of Ophthalmology,
Haeundae Paik Hospital, Inje University College of Medicine, Busan 612-030, South
Korea
Correspondence to: Soo Jung Lee. Department of
Ophthalmology, Haeundae Paik Hospital, Inje University College of Medicine,
Haeundae-ro 875, Haeundae-gu, Busan 612-030, South Korea. kris9352@hanmail.net
Received:
Abstract
AIM: To compare contrast sensitivity (CS) based on the surgical results for
intermittent exotropia (IXT) and to examine the relationship between CS and
photophobia.
METHODS: Medical records of the patients who underwent
bilateral lateral rectus muscle recession for IXT between 4 and 12 years old
were reviewed retrospectively. They were categorized based on the surgical
results; successful correction group (n=36) and overcorrection group
(esotropia ≥10 PD at 3mo postoperatively, n=18). Using CGT-2000 test for
CS was performed binocularly, and subjective reports of photophobia was
investigated preoperatively and at 3mo postoperatively. Objective photophobia
was defined as a significant decrease in CS in the presence of glare.
RESULTS: Preoperatively, there was no difference in CS
between the groups. Postoperatively, under mesopic conditions, significant
improvement of CS was observed at 6.3°, 4°, and 2.5° in the successful
correction group and at 6.3° and 4° in the overcorrection group, regardless of
glare. Under photopic conditions, at all visual angles except 0.64°,
improvement in CS was noted in both groups while CS worsened significantly at
0.64° in the overcorrection group postoperatively. At all visual angles under
photopic conditions postoperatively, regardless of glare, CS in the
overcorrected group was significantly worse than that in the successful
correction group, and CS was significantly decreased by addition of glare in
both groups. All patients except one (96.4%) in the successful correction group
and 8 patients (61.5%) in overcorrection group showed improvement of
photophobia postoperatively, which correlated with CS under photopic conditions
(P=0.001, 0.03).
CONCLUSION: After surgery for IXT, CS under photopic conditions
improve at all visual angles except 0.64°, while CS is significantly worse in
the overcorrection group postoperatively at 0.64°. Subjective photophobia have
significant correlation with CS under photopic conditions, and may be used as
an objective indicator of photophobia.
KEYWORDS: contrast sensitivity; intermittent
exotropia; overcorrection; photophobia; success
DOI:10.18240/ijo.2019.11.10
Citation: Kim HR, Lee SJ. Comparison of contrast sensitivity based on the
surgical results for intermittent exotropia. Int J Ophthalmol
2019;12(11):1725-1730
INTRODUCTION
It is
thought that photophobia appears to prevent pain caused by constriction of the
pupil by trigeminal nerve stimulation, acting as a protective mechanism against
harmful short wavelengths[1-4].
In patients with strabismus, it is believed that bright light stimulates the
retina and interferes with fusion, resulting in manifest strabismus, and photophobia
that closes the eyes appears to avoid diplopia and visual confusion. However,
no clear mechanism has been elucidated. The contrast sensitivity (CS) test is a
method for displaying the spatial resolution of the visual system, the results
of which could be abnormal in various diseases including amblyopia, optic
neuritis, cataract, glaucoma, strabismus, brain lesion, etc[5-6].
Previous
studies have examined photophobia patterns based on the subjective symptoms of
patients with intermittent exotropia (IXT)[7].
Chung et al[7] reported changes in
photophobia using CS test before and after surgery in patients with IXT, and
normal controls. Their studies are based on previous reports suggesting that
change in CS before and after cataract or refractive surgery is directly
affected by presence and absence of glare. Meanwhile, no study examined the
change of CS and its relationship with photophobia according to results of
strabismus surgery. This study was undertaken to compare the change of CS and
evaluate the relation of CS and photophobia in patients with successful
correction and overcorrection after surgery for IXT.
SUBJECTS AND METHODS
Ethical
Approval This study was approved by the
Institutional Review Board (IRB) of Inje University Haundae Paik Hospital,
Busan, South Korea (Approval number:
Medical
records of patients who underwent bilateral lateral rectus muscle recession
(BLR) for basic type IXT by one surgeon (Lee SJ) between August 2017 and March
2018 were reviewed retrospectively. Patients between 4y (deemed able to
cooperate in the CS test) and 12y (who had the potential to develop binocular
visual function) were included.
In order to
remove bias derived from type of IXT, only the basic type [difference in angle
of deviation ≤10 prism diopters (PD) between distance and near] IXT was
evaluated. To compare the CS according to the alignment of IXT, the patients
were divided into two groups according to the alignment after BLR at 3mo
postoperatively: 1) successful correction group (with exophoria ≤8 PD or
esophoria ≤4 PD at both distance and near, n=36); 2) overcorrection
group (with esotropia ≥10 PD at distance and near, n=18).
Patients
with history of paralytic strabismus, restrictive strabismus, amblyopia, ocular
abnormality, hyperopia or myopia ≥6 diopters (D), astigmatism ≥2 D, previous
ocular surgery (including strabismus surgery), nystagmus, congenital deformity,
neurologic abnormality, chromosomal disorder, or systemic diseases were
excluded from the study.
Age, sex,
best corrected visual acuity (BCVA; logMAR), spherical equivalent, preoperative
stereopsis (Titmus test), and binocular status (Worth 4 dot, W4D) were
recorded. Preoperative and postoperative angle of deviation were measured at a
distance of
The CS test using CGT-2000
(Takagi Seiko Co., Ltd., Tokyo, Japan) was performed preoperatively and 3mo
postoperatively. The CS was measured binocularly at 6 spatial frequencies
(6.3°, 4°, 2.5°, 1.6°, 1°, and 0.64°) under mesopic [average luminance of 5
candelas/square meter (cd/m2)] and photopic conditions (average
luminance of 100 cd/m2) with refractive correction. To provide glare
stimulus, 12 circularly aligned white lights (light-emitting diodes, LED) with a
brightness of 40 000 lx under mesopic conditions and 100 000 lx under photopic
conditions were added.
The test was carried out in the order as follows: mesopic without glare,
mesopic with glare, photopic without glare, and photopic with glare. In CS
test, photophobia was defined as a statistically significant decrease in test results
with glare.
Statistical
Analysis Statistical
analysis was performed using SPSS software version 12.10 (SPSS Inc., Chicago,
IL, USA). Independent t-test and Chi-square test were used to compare
the CS with presence or absence of glare at each spatial frequency and to
compare the CS difference between groups. The CS before and after BLR were
compared using the paired t-test. The concordance of preoperative
subjective photophobia symptoms and CS results obtained at the visual angle
with the highest reduction due to glare was evaluated by Run test. Considering
the lower prevalence of postoperative photophobia, resolution of subjective
photophobia symptoms and CS result obtained at the visual angle having no
difference due to glare was evaluated by Run test. A P-value less than
0.05 was considered as statistically significant.
RESULTS
Baseline
Characteristics of Study Subjects A total of
54 patients were included in the study. The mean age was 7.3±1.8 (4-12)y and 41
(75.9%) patients were female. All patients had a BCVA (logMAR) of 0 and the
average spherical equivalent was -0.5±2.1 (-5.8 to +5.7) D. Preoperative
stereopsis was 112.9±95.0 seconds of arc (40 to 800 seconds of arc), and 18
patients (33.3%) showed suppression. There were 36 patients in the successful
correction group, and
Table 1 Comparison of preoperative
baseline characteristics between groups according to the result of bilateral
rectus muscles recession in intermittent exotropia
mean±SD
(range)
|
Variables |
Successful correction group |
Overcorrection group |
P |
|
Totally (n) |
36 |
18 |
|
|
Age (y) |
7.4±2.0 (4 to 12) |
7.0±1.6 (5 to 10) |
|
|
Sex (F/M) |
26/10 |
15/3 |
0.65b |
|
BCVA (logMAR) |
0 |
0 |
|
|
Spherical equivalent (diopter) |
-0.4±2.3 (-5.75 to +5.63) |
-0.7±1.6 (-5.63 to +0.88) |
|
|
Stereopsis (seconds of arc) |
110.3±136.2 (40 to 800) |
96.7±39.3 (40 to 200) |
|
|
Suppression (n) |
11 |
7 |
0.54b |
|
Preoperative angle of deviation
(PD) |
+32.7±7.5 (+18 to +50) |
+31.7±4.5 (+25 to +40) |
|
|
Subjective report of photophobia
(patients) |
28 (77.8%) |
13 (72.2%) |
0.67b |
BCVA: Best corrected visual acuity;
“+” means exodeviation; aThe comparison was performed by using
Fisher’s exact test. bThe comparison was performed by using
Mann-Whitney U test.
The angle of
deviation was marked as “+” for exodeviation and “-” for esodeviation. In the
successful correction group, the angle of deviation changed from +32.7±7.5 (+18
to +50) PD preoperatively to +0.3±3.1 (-4 to +8) PD at 3mo postoperatively. In
the overcorrection group, the preoperative angle of deviation was +31.7±4.5
(+25 to +40) PD which changed to -15.0±3.4 (-18 to -10) PD postoperatively.
There was no significant difference in preoperative angle of deviation between
the two groups; the angle of deviation at 3mo postoperatively showed
statistically significant differences (P<0.001). In the
overcorrection group, 16 patients (88.9%) were treated with alternating
patching treatment while 2 patients (11.1%) were prescribed prism glasses. Six
patients who did not respond to patching were prescribed prism glasses in
addition to alternating patching treatment.
Preoperative
Comparison of CS Between Groups and Between Presence and Absence of Glare There was no
significant difference in CS between the successful correction group and overcorrection
group under both mesopic and photopic conditions, regardless of glare (mesopic
without glare, mesopic with glare, photopic without glare, photopic with glare:
P=0.880, 0.996, 0.978, and 0.948, respectively). Under mesopic
conditions, there was no significant difference in CS by glare stimuli (P=0.697
and 0.840 for the successful correction and overcorrection groups,
respectively). CS under photopic conditions tended to decrease at all visual
angles with addition of glare although with no statistical significance (P=0.459
and 0.533 for the successful correction and overcorrection groups,
respectively; Figures

Figure 1 CS test under mesopic conditions A:
Preoperative CS without glare; B: Preoperative CS with glare; C: Postoperative
CS without glare; D: Postoperative CS with glare.
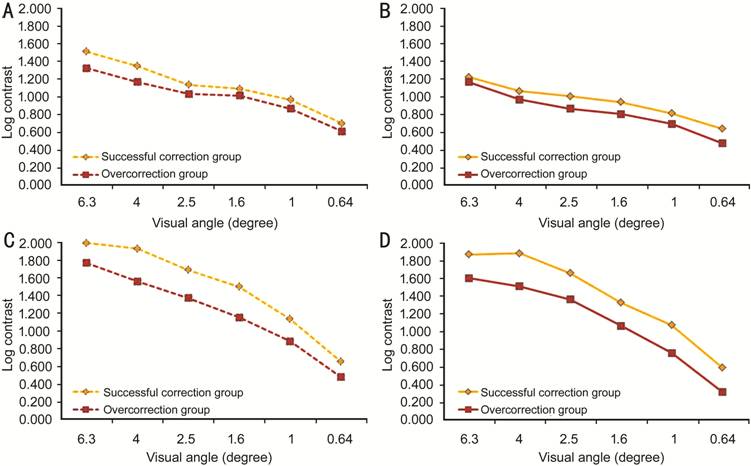
Figure 2 CS test under photopic
conditions A: Preoperative CS without glare; B:
Preoperative CS with glare; C: Postoperative CS without glare; D: Postoperative
CS with glare.
Comparison
of CS before and after BLR In the
successful correction group, CS significantly improved postoperatively at 6.3°,
4°, and 2.5° under mesopic conditions, regardless of glare, while there was no
significant difference at 1.6°, 1°, and 0.64°. In the overcorrection group,
under mesopic conditions regardless of glare, CS significantly improved
postoperatively at 6.3°, 4°, improved with no significant difference at 2.5°,
and decreased with no significant difference at 1.6°, 1°, and 0.64° (Figure 1,
Table 2).
Table 2 P-value
of change in contrast sensitivity before and after bilateral rectus muscle
recession
|
Visual angle (°) |
Mesopic without glare |
Mesopic with glare |
Photopic without glare |
Photopic with glare |
|
Successful correction group |
|
|
|
|
|
6.3 |
0.009 |
0.046 |
0.003 |
0.017 |
|
4 |
0.012 |
0.001 |
0.001 |
0.026 |
|
2.5 |
0.022 |
0.049 |
0.001 |
0.004 |
|
1.6 |
0.064 |
0.897 |
0.002 |
0.002 |
|
1 |
0.554 |
0.124 |
0.018 |
0.041 |
|
0.64 |
0.864 |
0.658 |
0.057 |
0.578 |
|
Overcorrection group |
|
|
|
|
|
6.3 |
0.042 |
0.034 |
0.001 |
0.039 |
|
4 |
0.017 |
0.027 |
0.001 |
0.029 |
|
2.5 |
0.066 |
0.054 |
0.001 |
0.043 |
|
1.6 |
0.485 |
0.545 |
0.003 |
0.044 |
|
1 |
0.658 |
0.721 |
0.012 |
0.675 |
|
0.64 |
0.590 |
0.445 |
0.003 |
0.002 |
Paired t-test.
Under
photopic conditions without glare, both groups showed significant improvement
in CS at all visual angles except 0.64° postoperatively. At 0.64°, there was
significant worsening of postoperative CS in the overcorrection group while no
difference was noted in the successful correction group. Under photopic
conditions with glare, postoperative CS significantly improved at all visual
angles except 0.64° in the successful correction group and at 6.3°, 4°, 2.5°,
and 1.6° in the overcorrection group. The latter showed no significant
difference in CS at 1°, and a significant decrease at 0.64° (Figure 2, Table
2).
Postoperative
Comparison of CS Between Groups and Between Presence and Absence of Glare Postoperatively
under mesopic conditions without glare, significant difference in CS between
groups was found at 6.3°, 4°, 2.5°, and 1.6° (all P<0.01). With
addition of glare stimuli, the absolute value of CS decreased in both groups at
6.3°, 4°, 2.5°, and 1.6°, with a non-significant difference between the groups
(Figure
All patients
except one (96.4%) in the successful correction group and 8 patients (61.5%) in
the overcorrection group showed improvement in photophobia postoperatively,
which correlated with CS under photopic conditions (P=0.001 and 0.03 for
the successful correction and overcorrection groups, respectively). No
significant correlation was found between subjective symptom and CS under
mesopic conditions (P=0.66 and 0.09 for the successful correction and
overcorrection groups, respectively).
DISCUSSION
IXT is the
most common form of exotropia, and patients often complain of blurred vision,
ocular fatigue, headache, diplopia, and photophobia. The reported prevalence of
photophobia in IXT varies from 54% to 65.5%[8-10]. However, the mechanism has not been clarified and
only a few hypotheses were suggested. Some claim that diplopia and binocular
photophobia are caused by an inability to suppress under bright light[10]. Others have claimed that, outdoors, there is insufficient stimulus to trigger
convergence so fusion is blocked by light stimulus, leading to manifest
strabismus, and this loss of control on alignment could be related to
photophobia[11-12]. Likewise,
children with exotropia often complain of photophobia under bright light[13], which is consistent with the findings of this study
where the CS changed depending on the absence or presence of glare under
photopic conditions. Further, improvement of CS after BLR at all visual angles
except 0.64° under photopic conditions in both groups
corresponds with previous studies as well.
The study results are distinct from
those of Chung et al[7], which showed
statistical agreement of CS under mesopic conditions with subjective
photophobia in the children with IXT. These differences can be explained by the
difference in setting value on CS test. Previous studies usually performed CS
test using Optec 6500 vision testing system, under the setting of a background
luminance of 3 cd/m2 for mesopic conditions
and 85 cd/m2 for photopic conditions, and glare
stimuli of 1 lx and 10 lx, respectively. Consequently, the difference in
intensity of glare light on the background luminance was greater under mesopic
conditions, and contraction of ciliary muscle by glare stimuli improved CS more
prominently under photopic conditions, leading to lesser difference in CS by
addition of glare under photopic conditions[2].
Our study was performed using CGT-2000 under a background luminance of 5 cd/m2 and
glare stimuli of 40 000 lx for mesopic conditions and a luminance of 100 cd/m2 and glare stimuli of 100 000 lx for
photopic conditions, a more intense glare, resulting in prominent difference
under photopic conditions. Also, previous studies were based on spatial
frequencies of 1.5, 3, 6, 12, 18 cycles per degree (cpd) while this study was conducted
under visual angles of 6.3, 4, 2.5, 1.6, 1, and 0.64 degrees, deviating the
test results to lower spatial frequency, equal to a larger visual angle. This
might lower the difference between CS under mesopic conditions with and without
glare.
Under mesopic
conditions without glare, postoperative CS at larger and intermediate visual
angles was significantly worse in the overcorrection group than in the
successful correction group. The absolute value of CS decreased in both groups
with addition of glare, and the difference between groups decreased to
non-significant levels. It is a plausible speculation that CS at small visual angles reflect
central visual acuity and high visual function. However, additional studies are needed to
clarify the difference with the current study.
Meanwhile, Chung et al[7] reported that CS was significantly lower at
intermediate and larger visual angles under both mesopic and photopic
conditions in the patients with IXT than in normal subjects, and improved
significantly at intermediate visual angles under mesopic conditions with glare
after strabismus surgery. Our study also showed postoperative improvement in CS
at larger visual angles and no significant difference at smaller visual
angles under
mesopic conditions in both groups. Improvement of CS at intermediate visual
angle (2.5°) in the successful correction group was also noted.
Under photopic conditions, CS
significantly improved postoperatively at all visual angles except 0.64° in
both groups. At 0.64°, postoperative CS was significantly decreased in the
overcorrection group and was similar in the successful correction group.
Previous studies have reported that CS worsened after intraocular surgeries[14-15], and theorized that it might be
due to decreased postoperative central visual acuity. However, postoperative CS
worsened even in the patients with good postoperative visual acuity, indicating
causative factors such as surgical stress or high visual functions other than
visual acuity[16]. Lew et al[12] analysed
the factors associated with binocular photophobia in IXT and found that it was
more common when the angle of exodeviation was greater than 25 PD and stereoacuity
worse than 60 seconds of arc. On this basis, they claimed that the distance
angle of strabismus reflects the strabismus condition better than the near
angle, and photophobia involves high-level visual functions like stereoacuity
rather than diplopia or exotropia itself[12]. Sjöstrand[17]
reported a decrease in CS at all spatial frequencies in anisometropic amblyopia
and decrease in CS only at high spatial frequencies in amblyopia with
esotropia, with no correlation between visual acuity and CS[15].
In addition, Jones et al[18] performed animal studies which showed damaged function of spatial CS of X-cells
of the lateral geniculate neuron only at high spatial frequencies in esotropia
comparing to normal controls. Therefore, postoperative CS decrease at a high
spatial frequency of 0.64° under photopic conditions in the overcorrection
group could be partially explained by decreased CS at high spatial frequencies,
and impaired stereopsis and high visual function in esotropia patients
comparing to normal controls[19-22]. Further studies are needed to elucidate the effect on
CS, especially, at high spatial frequency in esotropic patients without
amblyopia and to investigate the prevalence and clinical presentation of
photophobia in esotropia.
Under photopic conditions regardless
of visual angle and glare, the successful correction and overcorrection groups
showed significant difference in postoperative CS, which correlated with
subjective photophobia. Lew et al[12] reported
that photophobia also improved in cases of under-correction after exotropia
correction surgery if angle of deviation decreased to 15 PD or less. Chung et al[7] also reported improvement in glare disability even in
unsatisfactorily under-corrected IXT after strabismus surgery. These results
imply that decrease in angle of deviation improves suppression or fusion,
leading to alleviation of photophobia, which is more related to the extent of
exodeviation rather than the presence of exotropia. However, a larger angle of
exodeviation does not always coincide with more severe photophobia. Patients
have variable levels of photophobia threshold, and the symptom can be prominent
in exodeviation exceeding a certain degree or vanish below a certain degree.
Prominently worse postoperative CS in the overcorrection group both under
mesopic and photopic condition is thought to be related to decreased stereopsis
and high visual function due to esodeviation. Further studies on the
correlation between CS and decreased binocularity in overcorrection are needed.
The first limitation of this study
was a small study sample size. Secondly, some of the pediatric patients could
not clearly describe their subjective symptoms. Consequently, the difference in
preoperative and postoperative photophobia symptoms was not clearly identified
in some cases. Symptoms such as frequent blinking, eye frowning, and face turn
were checked based on parental observation; some studies have stated that
expression of these symptoms do not necessarily correspond to photophobia[23].
Nevertheless,
there was noticeable improvement in photophobia following reduction in angle of
exodeviation after surgery for IXT, and the postoperative photophobia was
significantly correlated with CS under photopic conditions. In conclusion, it
is expected that the CS test under photopic conditions in this study setting
can be used as an objective indicator of photophobia.
ACKNOWLEDGEMENTS
Conflicts of Interest: Kim HR, None; Lee SJ, None.
REFERENCES