
·Clinical Research·
Clinical
features and treatment outcomes of primary ocular adnexal mucosa-associated
lymphoid tissue lymphoma: a single center retrospective analysis of 64 patients
in China
Hui Yu1, Yu-Xin Du1, Zhen-Chang Sun1,
Xiao-Rui Fu1, Nan Tan2, Wei-Feng Gong2,
Ming-Zhi Zhang1
1Department of Oncology, Zhengzhou
University First Affiliated Hospital; Lymphoma Diagnosis and Treatment Center
of Henan Province, Zhengzhou 450052, Henan Province, China
2Department of Ophthalmology,
Zhengzhou University First Affiliated Hospital, Zhengzhou 450052, Henan
Province, China
Co-first authors: Hui Yu and Yu-Xin Du
Correspondence to: Wei-Feng Gong. Department of
Ophthalmology, Zhengzhou University First Affiliated Hospital, Νo. 1 Jianshe
East Road, Zhengzhou 450052, Henan Province, China. weifenggongky@163.com;
Ming-Zhi Zhang. Department of Oncology, Zhengzhou University First Affiliated
Hospital; Lymphoma Diagnosis and Treatment Center of Henan Province, Νo. 1
Jianshe East Road, Zhengzhou 450052, Henan Province, China.
mingzhi_zhang1@126.com
Received:
Abstract
AIM: To investigate the clinical features, treatment and prognosis of primary
ocular adnexal mucosa-associated lymphoid tissue lymphoma (POAML).
METHODS: A retrospective analysis was performed on 64
patients with POAML who were admitted to the First Affiliated Hospital of
Zhengzhou University from January 2006 to December 2018.
RESULTS: With a median follow-up of 61mo (range, 2-156mo),
estimated overall survival (OS) rate and progression-free survival (PFS) rate
at 10y reached 94.5% and 61.5%, respectively. Median OS time and PFS time were
not reached. During this period, only 3 patients died, but none of them died
directly due to disease progression. One patient (1.6%) developed
transformation to diffuse large B-cell lymphoma (DLBCL). Of the 56 patients
achieved complete remission after first-line treatment, 5 (8.9%) developed local
and/or systemic relapse eventually. Patients ≥60y had significantly shorter PFS
than younger patients (P=0.01). For patients with early stages (Ann
Arbor stage I and stage II), univariate analysis confirmed that radiotherapy
dose lower than 32 Gy were independently associated with shorter PFS (P=0.04).
Other factors including gender, bone marrow involvement, the initial location
of the disease, and the laterality were not associated with PFS.
CONCLUSION: The data from our center indicate that POAML has a
slow clinical progression and has an excellent clinical outcome. Patients with
POAML harbor a continual risk of relaps and transformation to aggressive
subtype of lymphoma.
KEYWORDS: primary ocular adnexal MALT
lymphoma; mucosa-associated lymphoid tissue; involved site radiation therapy;
immunochemotherapy
DOI:10.18240/ijo.2019.11.11
Citation: Yu
H, Du YX, Sun ZC, Fu XR, Tan N, Gong WF, Zhang MZ. Clinical features and
treatment outcomes of primary ocular adnexal mucosa-associated lymphoid tissue
lymphoma: a single center retrospective analysis of 64 patients in China. Int
J Ophthalmol 2019;12(11):1731-1736
INTRODUCTION
Primary ocular adnexal lymphoma
(POAL) is extranodal lymphoma that often occurs in the orbit, lacrimal gland,
conjunctiva, and eyelids, accounting for up to 55% of all ocular adnexal tumors[1-2]. In the 1970s, the annual incidence
of POAL was about 0.28 per 100 000, which showed a gradual increase in the past
40y[3-4]. Most of the POAL
belong to non-Hodgkin’s lymphoma (NHL), and the most common pathological
subtype is extranodal marginal zone lymphoma of mucosa-associated lymphoid
tissue (MALT) which accounts for 35% to 88% of POAL cases[5-7].
Despite significant advances in
studies of etiology, clinical manifestations and treatment of primary ocular
adnexal mucosa-associated lymphoid tissue lymphoma (POAML) in decades, there
are still many important etiological and prognostic issues that remain
unresolved[8-10]. Although some
studies have reported the close relationship between Chlamydia psittaci and
POAML in certain geographic areas, this connection is not universal and there
may be other inducing conditions[11]. In terms of
treatment, 85%-100% of patients with limited stages can get lasting clinical
remission by receiving radiotherapy treatment (RT), but the optimal dose of RT
remains controversial[12]. In addition, although
radiotherapy can perform good local control, it has been reported that 5%-32%
of patients will have systemic recurrence[8,13-14]. Regarding the use of immunochemotherapy
alone or combined with other treatment modalities, overall data is limited due
to the insufficient number of patients and lack of large prospective
multicenter studies, there is no consensus on the initial treatment guidelines
for patients with POAML. The clinical features of the initial disease site,
patient age, stage or initial performance are still controversial for the
prognosis of patients with POAML.
Currently, there are very few large cohort
studies reported on POAML in China. Consequently, we conducted a
single-institute retrospective analysis of 64 patients with POAML received
treatment at our institution between 2006 and 2018. The purpose of this
analysis was to analyze the impact of initial clinical presentation, staging
and different treatment modalities on prognosis, and will provide useful
guidelines for POAML treatment.
SUBJECTS AND METHODS
Ethical Approval This study was approved by the
Ethical Review Committee of the First Affiliated Hospital of Zhengzhou
University, Zhengzhou, China. All procedures adhered to the tenets of the
Declaration of Helsinki for research involving human subjects. Written informed
consents were obtained from all participants enrolled in this study.
Subjects and Enrollment
Criteria This study included 64 patients with
POAML who were admitted to the First Affiliated Hospital of Zhengzhou
University from January 2006 to December 2018. Patients enrolled in this study
were required to have biopsy material that diagnosed MALT lymphoma, according
to 2016 World Health Organization (WHO) classification criteria for lymphoid
hematopoietic tumors.
Information about the patients’
gender, age, Eastern Cooperative Oncology Group (ECOG) physical status (PS)
score, the symptoms and signs present at the initial diagnosis, imaging data,
treatment plan and prognosis were collected and recorded in detail. All
patients received comprehensive laboratory examinations, including blood
routine test, liver and kidney function, lactate dehydrogenase (LDH), β2‑microglobulin,
serum Immunofixation electrophoresis, coagulation function and hepatitis B
virus-DNA quantification. Bone marrow smears and biopsies were also performed.
Staging was based on the Ann Arbor
standard. Prognosis stratification was performed according to MALT lymphoma
international prognostic index (MALT⁃IPI). Age ≥70y, Ann Arbor stage III
or IV and serum LDH level above normal are prognostic disadvantages. One point
was calculated for each unfavorable factor. Patients with a total score of 0
were identified as low-risk, with score of 1 were classified as intermediate risk,
≥2 were divided into high-risk patients.
Treatment Patients’ treatment plans were
determined mainly based on the stage of the disease and judgments of physician.
Treatment methods are diversity including local therapy (surgery alone,
radiotherapy alone, surgery combined with radiotherapy) and systemic therapy
(immunochemotherapy, surgery combined with radiotherapy and immunotherapy,
radiotherapy and immunochemotherapy). Patients with limited stages were most
commonly treated with local therapy, mainly radiotherapy.
Statistical Analysis Overall survival (OS) is the length
time from the initial disease diagnosis to death from any cause or the last follow-up.
Progression-free survival (PFS) was defined as the time from diagnosis to
disease recurrence, pathological transformation, relapse, or death. Efficacy
assessment referred to the Lugano mitigation criteria for NHL, which includes
complete response (CR), partial response (PR), stable disease (SD) and
progressive disease (PD). The sum of the CR rate and the PR rate is the
objective response rate (ORR). No patients were excluded from efficacy and
survival analysis because of missing efficacy information. Statistical analysis
was performed using SPSS 17.0 software (SPSS, Chicago, IL, USA), survival curve
was drawn by Kaplan⁃Meier method, and single factor
survival analysis was performed by Log⁃rank test. P≤0.05 was
considered statistically significant.
RESULTS
Clinical Characteristics Between 2006 and 2018, 64 patients
with POAML received treatment at our institutions. Median age at diagnosis was
58y (range, 41-82y), including 36 males (56.3%) and 28 females (43.7%). The
remaining clinical features are detailed in Table 1.
Table 1 Clinical features of the 64
patients with primary ocular adnexal MALT lymphoma
|
Characteristic |
n (%) |
|
Gender |
|
|
Male |
36 (56.3) |
|
Female |
28 (43.7) |
|
Anatomical location |
|
|
Orbit |
39 (60.9) |
|
Conjunctiva |
15 (23.4) |
|
Lacrimal gland |
11 (17.2) |
|
Eyelids |
12 (18.8) |
|
Bilateral disease |
5 (7.8) |
|
Ann Arbor stage |
|
|
I |
52 (81.3) |
|
Ⅱ |
3 (4.7) |
|
Ⅲ |
4 (6.3) |
|
Ⅳ |
5 (7.8) |
|
MALT⁃IPI score |
|
|
0 |
48 (75.0) |
|
1 |
10 (15.6) |
|
≥2 |
6 (9.4) |
|
ECOG PS score |
|
|
0 |
61 (95.3) |
|
≥1 |
3 (4.7) |
|
LDH above normal |
6 (9.4) |
|
Bone marrow involvement |
4 (6.3) |
MALT⁃IPI:
Mucosa-associated lymphoid tissue international prognostic index; LDH: Lactate dehydrogenase;
ECOG PS score: Eastern Cooperative Oncology Group physical status score.
Relevant previous medical history
was Sjögren’s Syndrome (SS) and eye disorders in 2 patients (3.1%) and 7
patients (10.9%), respectively. Chronic hepatitis B infections were detected in
2 (3.1%) patients. Only 51 patients underwent the monoclonal gammopathy test
through blood examination, of which 5 patients were immunoglobulin M (IgM)
type, 1 patient IgG type, and 1 patient IgA type.
Orbit were the most common primary
site involved (39 patients, 60.9%), followed by conjunctiva (15 patients,
23.4%), lacrimal glands (11 patients, 17.2%) and eyelids (12 patients, 18.8%).
Among them, 5 cases were bilateral lesions (7.8%). The clinical characteristics
of POAML are diverse according to the location of tumors. Common symptoms of
patients in this study included eyelid swelling, proptosis, conjunctival
injection, painless palpable mass, ptosis, foreign body sensation, blurred
vision, and blurred vision.
All the patients underwent
whole-body imaging or bone marrow examination. At the time of presentation, 52
(81.3%) patients and 3 (4.7%) patients were with limited stage, Ann Arbor stage
I, II, respectively. 4 (6.3%) patients and 5 (7.8%) patients were with stage
III and stage IV, respectively. The majority of patients had good physical
condition with an ECOG PS score of 0 (95.3%, 61/64). Risk stratification showed
that most patients were at low and medium risk (58 patients, 90.6%), only 6 patients
(9.4%) were evaluated as high risk with MALT-IPI score ≥2. Among them, 6
patients (9.4%) were detected with increased LDH at the time of initial
diagnosis.
Treatment, Response, and
Follow-up A total of 64 patients had available
data of first-line therapy, response and outcome. Details of response rates and
relapses rates of varied treatment modalities are summarized in Table 2.
Table 2 Outcomes according to
treatment modalities and disease stage at presentation
|
Ann Arbor stage |
n |
CR |
Relapse |
|
I, II |
|
|
|
|
Local treatment |
|
|
|
|
ISRT |
30 |
27 |
5 |
|
Surgery only |
4 |
4 |
2 |
|
Surgery+ISRT |
15 |
13 |
2 |
|
Systemic treatment |
|
|
|
|
Rituximab+ISRT |
4 |
4 |
1 |
|
Surgery+rituximab+ISRT |
2 |
2 |
0 |
|
III, IV |
|
|
|
|
R-CVP |
5 |
3 |
2 |
|
R-CHOP |
3 |
2 |
1 |
|
R-CVP+ISRT |
1 |
1 |
0 |
ISRT: Involved site radiation
therapy; R-CVP: Rituximab, cyclophosphamide, vincristine/vindesine, prednisone;
R-CHOP: Rituximab, cyclophosphamide, epirubicin, vincristine/vindesine,
prednisone; CR: Complete response.
Among the patients with limited
stage (Ann Arbor stage I and stage II), there were 30 patients received
involved site radiation therapy (ISRT) alone, and 4 patients only received
surgery treatment. Fifteen patients and 4 patients underwent the ISRT combined
with surgery and ISRT combined with rituximab, respectively. Only 3 (5.5%) of
these patients with limited stages did not achieve CR. With a median follow up
of 58.5mo (range, 2-156), the incidence of relapse in the local treatment
groups (ISRT and/or surgery) was not significantly different than the patients
received systemic treatment (P-value is 0.92).
Among the patients with advanced
stage (Ann Arbor stage III and stage IV), five patients of them were treated
with rituximab, cyclophosphamide, vincristine/vindesine, prednisone (R-CVP)
regimen, and 3 patients were received rituximab, cyclophosphamide, epirubicin,
vincristine/vindesine, prednisone (R-CHOP). Only 1 patient was treated with
R-CVP combined with ISRT, since after the systemic therapy, the eyelid involved
did not reach CR, and local ISRT was followed as the adjuvant treatment.
Although 3 (33.3%) of these patients with advanced stages did not reach CR
after the initial treatment, the incidence of relapse of the patients with
advanced stage was no significant difference with the patients with the limited
stages groups (P-value is 0.29). Overall, the dose of radiotherapy
varied though our study period, ranging from 26 to 45 Gy (median dose, 32 Gy). First-line
treatment resulted in CR in 56 patients (87.5%) and PR in 4 patients (6.3%; 1
patient with stage I, 1 patient with stage IV), SD in 2 patients with stage II,
and PD in 3 patients (1 patient with stage I, 1 patient with stage II, and 1
patient with stage III).
Survival, Outcome and Prognostic
Factors Follow-up data were available for
all patients with a median follow-up of 61mo, with ranging from 2 to 156mo.
During this period of time, only 3 patients died, but none of them died
directly of disease progression. The OS rate is 94.5% at 10y (Figure
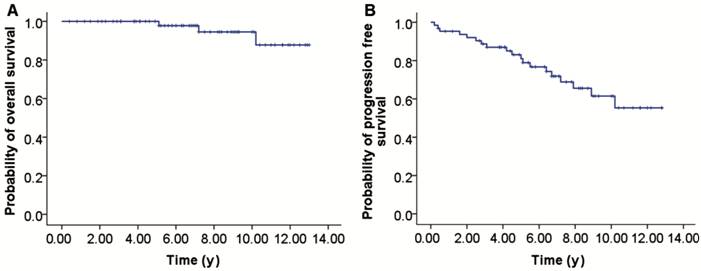
Figure 1 Survival of patients with
POAML A: OS; B: PFS.
Associations between age, gender,
stage, LDH levels, bone marrow involvement, treatment, and outcome were
examined. Since there is no disease progression-related death, we focused on
analyzing the factors related with PFS. Among these factors, gender, bone
marrow involvement, the initial location of the disease, and the laterality
were not associated with PFS. The identified prognostic factors including age and
radiotherapy dose are shown in Figure 2. Patients ≥60y had significantly
shorter PFS than younger patients (P=0.01; Figure
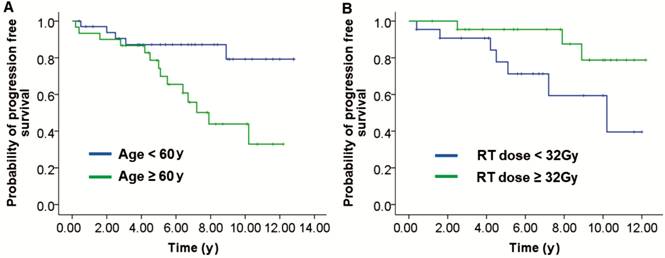
Figure 2 Univariate analysis of
factors associated with PFS A: According to the age of all
patients: aged <60y versus ≥60y; B: According to the radiotherapy dose in
patients with stage I and II: RT dose <32 Gy versus ≥32 Gy.
DISCUSSION
Lymphoma is the most common type of
adult primary ocular adnexal tumors, and POAL mainly involves the orbit,
conjunctiva, eyelids, lacrimal glands, and lacrimal sac. Among the pathological
types, the incidence of MALT lymphoma was the highest, accounting for 62%, and
its prognosis was significantly better than other pathological types.
Follicular lymphoma (17%) is the second most common subtype followed by DLBCL
(10%)[15]. The present study summarized 64 cases
of POAML in our single institute, which, to our best knowledge, is a largest retrospective
study on POAML in China. Our findings are not only consistent with some results
of the previously reported observations, but also provided new information on
prognostic factors, treatment and outcomes specifically for Chinese patients.
Multiple retrospective studies from western countries have reported clinical
features of POAML, including female preponderance, median age about 65y, and
frequent occurrence in the orbit[8]. However,
studies from other Asian counties described a significantly younger median age
about 45y and a male prevalence[5,9,16]. Median age at diagnosis of our cohort is 58 years
old, and the ratio of male to female is 1.3:1, which is similar to that
reported in Asian countries such as Japan and South Korea. These results
suggest that there is a significant difference between Asian countries and
western countries in the age and gender composition of POAML.
The literature reports that ocular
adnexal lymphoma most often affects orbital, bilateral involvement of about 7%
to 24%, bone marrow involvement of about 2% to 8.6%[8,17-19], our data is consistent with
previous reports with orbit involvement (60.9%), bilateral disease (7.8%), and
bone marrow involvement (6.3%). Although researchers from Miller School of
Medicine demonstrated that bilateral involvement was independently associated
with inferior outcome with statistically shorter OS and PFS than in patients
with unilateral disease[8]. Data from our center
was exhibited no statistical connection between bilateral disease and the
outcome.
Majority of the patients were with
limited stages at the time of initial diagnosis. The patients with stage I
accounted for 52 cases (81.3%), with low and intermediate risk. Only 1 patient
had B symptoms (unexplained fever >
The commonly recognized pathogenesis
of POAML include chronic inflammation (for example, C psittaci) or autoimmune
disorders that produce sustained antigenic stimulation, resulting in localized
lymphoid tissue hyperplasia. Sustained chronic antigen stimulation can cause
genetic instability, leading to the proliferation of normal lymphoid cell
malignant clones, which eventually transform into MALT lymphoma. The C psittaci
tests were negative in all patients in our study. However, reports from other
geographic showed that C psittaci infection was found to be closely related to
the occurrence of the disease[11,14].
Compared with normal population controls, patients with autoimmune disorders,
such as rheumatoid arthritis, SS and systemic lupus erythematosus, are more
likely to develop MALT lymphoma, which again suggests an important role for
autoimmune disorders in the pathogenesis of POAML[20].
Two patients in our study had a history SS and received treatment. Engels et
al[21] reported that patients with SS had a
1000-fold increased risk of developing MALT-type lymphoma.
Treatment of POAML is effective by
surgical resection, radiotherapy and chemotherapy. ISRT performed an excellent
local control (86% to 100%) of POAML patients at Ann Arbor stage I in all
previous studies. Consistent with previous reports, ISRT also performed local
control in 87% of our patients at stage I. Although the excellent initial
remission to ISRT in stage I patients, a continuous risk of local or distant
relapse or progression of 6.7% at 1y, 10% at 5y, and 16.7% at 10y were
observed. Desai et al[8] showed that local
and systemic relapses or progression of 5.1% at 1y, 17.5% at 5y, and 31% at 10y
for the patients with Ann Arbor stage I after radiotherapy as initial
treatment. Decaudin et al[22] summarized
that systemic relapses (6% to 50%) and local relapses (up to 15%) were observed
in patients treated with radiotherapy in a POAML review. Transformation to
aggressive lymphoma and central nervous system involvement has also been
reported. The cause of recurrence may be explained by microscopic disease
remaining outside the surgical or radiotherapy treatment area. Therefore,
although the patient can achieve good local control, some patients will still
have distant recurrence in a short time or years. Kim et al[23] reported that patients with POAML have high risk
factors, surgery combined with immunochemotherapy may reduce the recurrence
rate. Six patients with stage I-II POAML in our center underwent immunotherapy
or immunochemotherapy after local treatment, and all of them reached CR after
initial treatment. Only one patient developed disease progression as of the end
of follow-up. Although we found that patients with high MALT-IPI scores,
immunotherapy or immunochemotherapy combined with local radiotherapy, have the
tendency to improve PFS compared with ISRT alone. However, the reason may be
the limited number of cases, and there is no statistical difference in PFS
between these two modalities.
The optimal dose of radiotherapy has
not yet reached a consensus, high dose of radiotherapy can reduce the
recurrence rate, but the incidence of adverse reactions related to radiotherapy
is correspondingly increased. Desai et al[8],
who analyzed 98 patients with stage I, demonstrated that whether the dose of RT
(<30.6 Gy vs ≥30.6 Gy, P=0.0001) or doses of (<36 Gy vs
≥36 Gy, P=0.0007) were related with PFS, but not OS. Fung et al[24] reported a similar observation that 5-year local
control rate was 81% in patients treated with RT at doses of <30 Gy, but in those
received RT dose ≥30 Gy5-year local control rate reached 100% (P<0.01).
The optimal radiation dose 30.6-32.4 Gy in 1.8 Gy fractions was suggested for POAML
patients. The dose of radiotherapy varied though our study period, ranging from
26 to 45 Gy (median dose, 32 Gy). We demonstrated that RT at dose lower than 32
Gy led to higher incidence of local and systemic recurrence and shorter PFS
compared with patients received RT dose ≥32 Gy. Therefore, the range of RT
effective doses reported in the literature is very broad. Overall, the analysis
showed that higher RT doses led to better PFS, but also increased the risk of
local acute and chronic complications. To demonstrate whether lower dose of
radiotherapy combined with immunotherapy has superior PFS than the radiotherapy
alone, long-term follow-up and large cohort study are required.
In summary, our study confirms that
POAML is relatively indolent disease, characterized by long survival, the
persistent risk of recurrence and transformation to aggressive lymphoma.
Through partial results reported in this article is not completely consistent
with previous reports, and there is controversy. We demonstrated that age and
radiotherapy dose affected the outcome of POAML patients. There findings will
be helpful in stratification of POAML patients in future treatment studies.
Prospective clinical studies, multi-center collaboration, and large sample
statistics may help us understand the disease more deeply.
ACKNOWLEDGEMENTS
Foundation: Supported by the National Natural
Science Foundation of China (Henan Joint Fund, No.U1404308)
Conflicts of Interest: Yu H, None; Du YX, None; Sun ZC,
None; Fu XR, None; Tan N, None; Gong WF, None; Zhang
MZ, None.
REFERENCES