
·Letter
to the Editor·
Successful
scleral buckling for long-standing retinal detachment with subretinal
proliferation 4-year after strabismus surgery
Hyuna Kim1, In Young Chung1,2
1Department of Ophthalmology,
Gyeongsang National University College of Medicine, Jinju 52727, Korea
2Institute of Health Science,
Gyeongsang National University, Jinju 52727, Korea
Correspondence to: In Young Chung. Department of
Ophthalmology, Gyeongsang National University Hospital, #79 Gangnam-ro, Jinju
52727, Korea. in0chung@hanmail.net
Received:
DOI:10.18240/ijo.2019.11.24
Citation: Kim
H, Chung IY. Successful scleral buckling for long-standing retinal detachment
with subretinal proliferation 4-year after strabismus surgery. Int J
Ophthalmol 2019;12(11):1812-1814
Dear Editor,
We would like to report the case of
a patient with long-standing retinal detachment (RD) with subretinal
proliferation after strabismus surgery who was successfully treated by scleral
buckling. Globe perforation is a potentially dangerous complication of
strabismus surgery that may result in vision loss or even complete blindness
and pthisis bulbi[1-2]. Because
most cases of scleral perforation occurred with handling ocular muscles are
limited in superficial in depth and short in length, and produce no
complications—its true incidence is not always apparent. Older studies have
reported an incidence rate of 8%-12.1% of cases[3],
whereas more recent studies have reported the rate as 0.13%-2.8%[4]. This decrease in the incidence has resulted from
improved surgical techniques and the introduction of spatula needles. Increased
awareness among surgeons may have also contributed to this decrease. Possible
treatment options recommended for globe perforation include observation alone,
cryopexy, diathermy, and laser retinopexy[5],
however, treatment is still under debate. An iatrogenic scleral perforation
typically causes damage to the immediate adjacent choroid, and there may or may
not be damage to the underlying retina, depending on the depth of the needle
pass[6]. Most cases with perforation are
asymptomatic, however, visual loss with RD may occur several years later. In
this study, we obtained the written informed consent from the patient, and this
case study is in accordance with the tenets of the Declaration of Helsinki.
An 8-year-old male was referred to
our hospital for decreased visual acuity 2 days ago in his right eye. Upon
examination, his visual acuity was hand motion in the right eye,
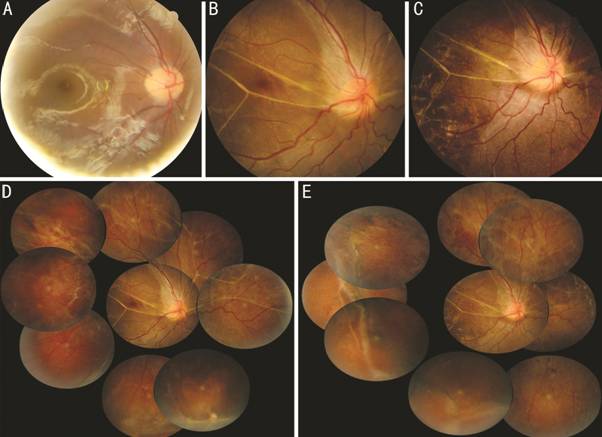
Figure 1 Fundus of the right eye Obtained at the day after previous
surgery (A), at initial visit (B, D), and at last follow-up (C, E). A: Normal fundus
and optic disc configuration; B, D: Wide shallow RD with multiple subretinal
bands; C, E: Attached retina after scleral buckling.
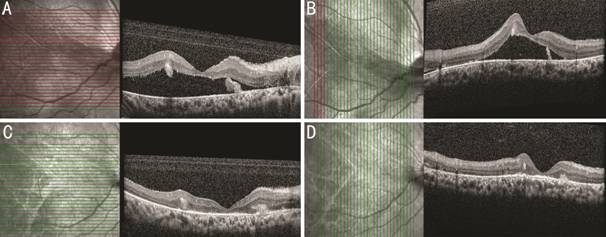
Figure 2 Optical coherence
tomography of the right eye A, B: RD including macula.
Intraretinal cystic lesion with peripapillary fibrous proliferation with band.
C, D: Attached retina after scleral buckling. Whole retinal layers were
thinned, and photoreceptor layer was disrupted. Some intraretinal cysts still
existed.
During the surgery, we identified
small atrophic linear scar underneath the recessed lateral rectus muscle, which
suspected the estimated perforation site during prior strabismus surgery. We
performed scleral buckling and encircling with subretinal fluid drainage.
Following conjunctival incision and four rectus muscle guiding sutures for
isolation, sclerotomy was performed at the inferotemporal area to drain the
subretinal fluid. Segmental buckling procedure using
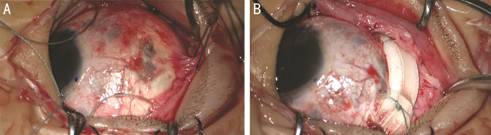
Figure 3 Intraoperative findings A: The estimated perforation site was
exposed after conjunctival incision and guiding sutures, located adjacent to
the new insertion of the recessed lateral rectus muscle. B: Segmental buckling
procedure using
Not all retinal breaks progress to
true detachment. Vitreous changes, such as the detachment of the vitreous and
vitreoretinal adhesions at the location of the break, contribute to the
production of RD. The fibrous tissue emanating from the perforation site is one
of the common findings in cases with retinal breaks progressed to RD. Although
there is no consensus regarding prophylactic treatment, laser treatment or
cryopexy is likely warranted for some cases with risks. Patients who have
disturbed vitreous, including aphakia, high myopia, systemic collagen disorders
such as Marfan syndrome, older age, extensive retinal damage, or fluid cuffs
around the retinal perforation, or those unavailable for follow-up are
considered to have predisposing factors for RD. However, our patient was an
8-year-old male who had a firm vitreous base and was unaware of the perforation
during surgery. In the one of previous report, in nearly every case, the
surgeon was aware of all subsequently identified perforations during surgery[7]. By the retrospective review with routine funduscopic
examination after strabismus surgery, they detected 10 scleral perforations in
513 patients (1121 procedures). They reported that most perforations were not
detected at the time of the surgery and were incidental findings at the time of
screening[8]. Some authors have recommended
routine funduscopy after surgery. In our case, a patient without any risk
factor who was unaware of the perforation during surgery presented with true RD
with severe visual loss after 4 years. During surgery, good exposure, maintaining
a dry operative field, using adequate magnification and illumination,
manipulation of the needle tangential to sclera, use of blunt-tipped scissor,
and providing special attention to fibrotic muscles are important. Long-term
follow-up is also essential. In our case, a progression of chronic RD was not
detected despite of regular visual acuity check-up in local eye clinic. The
patient was only 8-year-old, the peripheral visual field occlusion and minor
floater was not recognized by him or disregarded by doctor. Also, the central
visual acuity may be remained well until the macular-off detachment
development.
Retinal thinning resulting in
atrophy is a characteristic finding in long-standing RD[9].
Secondary intraretinal cysts may develop if RD has been present for
approximately 1y, and these disappear after retinal reattachment. In this case,
scleral buckling surgery was performed to treat long-standing RD with
subretinal proliferations. Scleral buckling is highly successful in eyes with
rhegmatogenous RD associated with subretinal proliferations and no or minimal
epiretinal proliferations[10]. An additional
360-degree encircling was performed in order not to miss all retinal holes and
tears in long-standing RD. Because of the location of the perforation site, the
buckling sponge was applied upon the new insertion of the recessed lateral
rectus muscle, but there was no adverse effect to muscle action.
In this case, a patient without any
predisposing factor who was unaware of perforation during surgery progressed to
true RD with severe visual loss after 4y. After surgery, a regular examination,
including dilated funduscopy, should be followed. Scleral buckling surgery on
recessed muscle is a good treatment option.
ACKNOWLEDGEMENTS
Conflicts of Interest: Kim H, None; Chung IY, None.
REFERENCES