
·Clinical Research·
Impact
of corneal parameters on intraocular pressure measurements in different
tonometry methods
Aleksandra Zakrzewska, Marta P. Wiącek, Anna Machalińska
First Department of Ophthalmology,
Pomeranian Medical University, Szczecin 70-111, Poland
Correspondence to: Anna Machalińska. Department of
Ophthalmology, Pomeranian Medical University, Al. Powstańców Wielkopolskich 72,
Szczecin 70-111, Poland. annam@pum.edu.pl
Received:
Abstract
AIM: To evaluate the impact of central corneal thickness (CCT) and corneal
curvature on intraocular pressure (IOP) measurements performed by three
different tonometers.
METHODS: IOP in 132 healthy eyes of 66 participants was
measured using three different tonometry techniques: Goldmann applanation
tonometer (GAT), Pascal dynamic contour tonometer (DCT), and ICare rebound
tonometer (RT). CCT and corneal curvature were assessed.
RESULTS: In healthy eyes, DCT presents significantly higher
values of IOP than GAT (17.34±3.69 and 15.27±
CONCLUSION: The same method should always be chosen for routine
IOP control, and measurements obtained by different methods cannot be compared.
All analysed tonometry methods are dependent on CCT; thus, CCT should be taken
into consideration for both diagnostics and monitoring.
KEYWORDS: intraocular
pressure; Goldmann applanation tonometer; Pascal dynamic contour tonometer;
ICare rebound tonometer; central corneal thickness; corneal curvature; healthy
individuals
DOI:10.18240/ijo.2019.12.06
Citation:
Zakrzewska A, Wiącek MP, Machalińska
A. Impact of corneal parameters on intraocular
pressure measurements in different tonometry methods. Int J Ophthalmol 2019;12(12):1853-1858
INTRODUCTION
Intraocular
pressure (IOP) is one of the most fundamental ophthalmological examinations. In
many cases, the result is used to determine an accurate therapeutic
approach.The IOP distribution in the general population ranges from 11 up to
According to
the available data, the usage of any tonometry techniques is restricted by many
conditions related to corneal morphology and biomechanical properties. Various
studies have shown that corneal parameters, such as central thickness,
elasticity, rigidity and curvature, can act as a measurement bias[1,5-6].
In
connection with the above findings, the question arises regarding which method
should be chosen for routine ophthalmologic examination. The aim of the study
was to compare intraocular values obtained with three different tonometers.
Additionally, the impact of central corneal thickness (CCT) and corneal
curvature on IOP measurements was assessed.
SUBJECTS AND METHODS
Ethical
Approval The study
was in compliance with the tenets of the Declaration of Helsinki. Written
informed consent was obtained from all subjects before examination.
In total,
132 healthy eyes of 66 patients examined in the First Department of
Ophthalmology at Pomeranian Medical University in Szczecin were included in the
study. Exclusion criteria were acute inflammation, history of glaucoma or any
eye surgery in the examined eye, and age under 50 and more than 85y. In all participants slit lamp
examination and fundus evaluation were performed. First, the
examination of corneal curvature and CCT were performed sequentially. Then, the
IOP examination was performed with three different tonometry techniques in
following order: RT, DCT and GAT. All measurements were performed by the one
examiner.
Measurements
Using the Goldmann Applanation Tonometer Method All GAT
(Haag Streit International, Koeniz, Switzerland) measurements were performed
after using topical anaesthetic (Alcaine®; Alcon Laboratories Inc.,
Fort Worth, TX, USA) and placing single, dry fluorescein strip over the
inferior tear meniscus. Examination was performed under a cobalt blue-filtered
light, and disposable prisms were used. After staining the cornea, the tip of
the prism was moved so that it was in contact with the central surface of the
cornea. Next, the dial of the tonometer was turned clockwise until two half
circles appeared and formed a horizontal letter S. The inner edges of both half
circles touched gently. The final result was the average of three consecutive
measurements.
Measurements
Using ICare Rebound Tonometer The
principle of RT tonometer (Tiolat
Oy, Helsinki, Finland) is based on the inductive method for measuring the
probe’s reflection force. This method allows quick and accurate measurement of IOP without the
use of anaesthetics. Before the examination, each patient was asked to look
straight ahead. The device was settled near the patient’s eye so that the
disposable probe is positioned horizontally, forming a right angle with the
central surface of the cornea. The distance between the surface of the cornea
and the tip of the probe was 4
Measurements
Using Dynamic Contour Tonometer The DCT (SMT
Swiss Microtechnology AG, Port, Switzerland) measures pulsing IOP in a direct
and continuous (dynamic) manner. The device is attached to the slit lamp and
consists of a pressure-sensing tip. During the examination, the sensor tip
touches the central corneal surface, and integrated baroreceptors measure IOP
without corneal applanation. Before the examination, topical anaesthetic was
instilled on the eye (Alcaine®; Alcon Laboratories Inc., Fort Worth,
TX, USA). The patient was asked to look straight ahead with eyes wide open and
not move for a few seconds. A disposable sensor cap was applied on the sensor
tip and moved forward until it touched the surface of the central cornea. The
signal sound informed about the detected IOP, and the result was presented on
digital display after 5s. Additionally, with every measurement, ocular pulse
amplitude (OPA) and a quality score (Q) were presented. The quality score
ranges from Q1 to Q5, and Q1 and Q2 correspond to the most reliable results.
Hence, only Q1 or Q2 results were included in statistical analysis.
Corneal
Curvature Corneal
curvature measurement was performed using KR-800 Auto Kerato-Refractometer
(Topcon, Tokyo, Japan). For each eye, the values of flat (R1) and steep (R2)
meridians of corneal curvature were assessed and presented in dioptres (D) and
mm. Averaged R1 and R2 values was considered for further statistical analysis[7].
Central
Corneal Thickness CCT was
measured with the Reichert ultrasonic pachymeter (Reichert iPac, Reichert, Inc.
Depew, NY, USA). Before the examination, the pachymeter tip was sterilized, and
topical anaesthetic was instilled on the eye. The patient was instructed to
look straight ahead with eyes wide open. The pachymeter tip was settled
perpendicularly to the central cornea with a minimal contact with its surface.
The final result was displayed after a series of beeps. The mean of three
consecutive readings was recorded.
Statistical
Analysis Descriptive
statistics are presented as the mean±standard deviation (SD). The
normality of the continuous variables was evaluated with the Shapiro-Wilk test.
The differences in IOP values between DCT or RT and GAT were analysed using the
t-test. Bland-Altman plots
were used to evaluate the agreement between the methods with 95% limits of
agreement (LoA) calculated as the mean difference± (1.96×SD). Simple and
multivariate linear regression analyses were used to study the relationship
between variables, such as corneal thickness and curvature, with IOP
measurements. For all tests and measurements, the statistical significance was
set at 0.05.
RESULTS
One hundred
thirty two nonglaucomatous eyes of 37 women and 29 men were enrolled. The mean
age of the participants was 70.95±7.76y. The CCT varied from 501 to 830 µm with
a mean value of 586.07±55.75 µm. The average keratometry for the whole group
was 43.93±1.46 D (7.69±
Table 1 The results of IOP
measurements mm Hg, mean±SD
|
Methods |
All |
<600 µm |
≥600 µm |
|
DCT |
17.34± |
17.41± |
17.18± |
|
GAT |
15.27±4.06 |
14.90±4.07 |
16.19±3.95 |
|
RT |
13.56± |
13.29± |
14.24± |
DCT: Dynamic contour tonometer; GAT:
Goldmann applanation tonometer; RT: Rebound tonometer. aP<0.0001 comparison with GAT.
In the next
part of the statistical analysis, the study group was divided into two groups
depending on CCT: less than
600 μm (n=47)
and greater than 600 μm (n=19). Bland-Altman plots
were used to evaluate the agreement among RT, Pascal DCT and reference GAT
readings. Figure
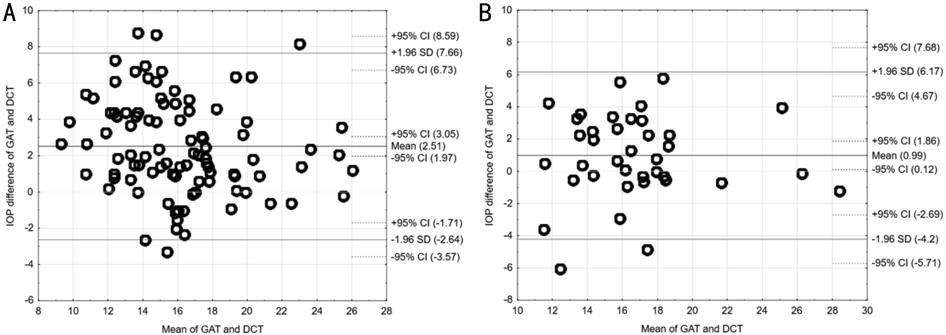
Figure 1
Agreement between the Goldmann applanation tonometry (GAT) method and dynamic contour
tonometry (DCT) in eyes with CCT<600 µm (A) and CCT≥600 µm (B).
Figure 2
shows the
agreement between RT and GAT IOP readings in both groups (less than 600 μm and
greater than 600 μm), respectively. Based on the graphs, we can
conclude that the IOP RT results were lower on average by
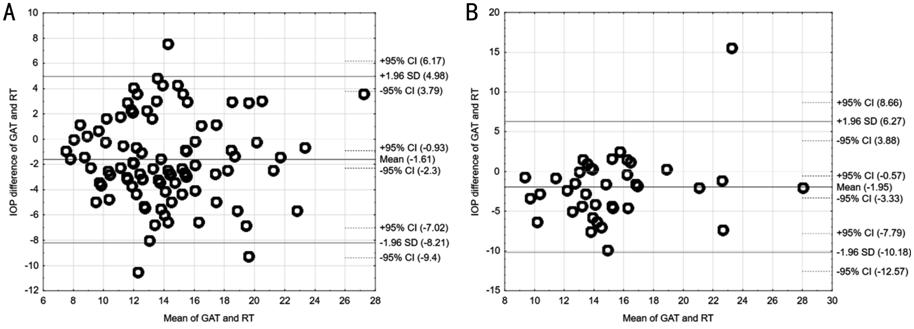
Figure 2
Agreement between the Goldmann applanation tonometry (GAT) method and rebound
tonometry (RT) in eyes with CCT<600 µm (A) and CCT≥600 µm (B).
We conclude
that the highest agreement was demonstrated for GAT and DCT IOP values in the
group with CCT≥600 μm and GAT and RT results in the group with
CCT<600 μm. The lowest consistency of measurements were
demonstrated for GAT and DCT IOP readings in the group with CCT<600 μm.
Because
available data suggest that corneal thickness may significantly affect IOP measurements,
we analysed the relationship between IOP values obtained by different
measurement methods and CCT. Simple regression analysis showed that CCT has a
significant impact on IOP measured with all devices in groups with corneal
thickness below 600 μm. The strongest positive correlations were
observed between CCT and RT IOP values (R=+0.351, P=0.0005).
Similarly, positive correlations were also detected between CCT and GAT and DCT
IOP measurements (R=+0.24, P=0.019 and R=+0.224; P=0.029, respectively).
This finding indicates that the IOP measurements are higher for thicker
corneas. A similar relationship was not observed in the group of eyes with
thicker corneas (greater than 600 μm).
Another
parameter that can significantly affect the IOP measurement is corneal
curvature. To verify this relation, a correlation analysis between IOP
measurements and values describing corneal curvature (D/mm) was performed. We
found no correlation between IOP values and keratometry results in groups with
CCT<600 μm independent of the IOP technique used. In parallel,
some positive correlations were found between GAT IOP values and keratometry
results in the group with CCT≥600 μm (R=+0.369; P=0.005). This finding
indicates that the steeper curvature of the cornea, the higher IOP values
detected with GAT.
DISCUSSION
Among the
many available methods of IOP tonometry, GAT still maintains an unchanging
position as the reference method. However, in some cases, measurements with
this method may be difficult, for example due to the lack of cooperation
(children) or irregularity of the corneal surface or even fluorescein allergy.
Accordingly, other methods, such as DCT or RT, could be more convenient.
Several studies have demonstrated that the measurements obtained with individual
methods may differ significantly. In our study, similar to results reported by
Rosentreter et al[8], the
highest IOP values were obtained with DCT, and the lowest were noted with the
RT. We observed significant differences in IOP values among all three
measurement techniques. The measurements performed with DCT were significantly
higher in relation to GAT. A similar relationship was observed by other authors
where DCT measurements were 0.9
On the other
hand, we observed the lowest consistency of measurements for GAT and DCT in the
group with CCT<600 μm. The results presented by Andreanos et al[9] indicate
that the biggest differences between GAT and DCT IOP measurements were observed
in the group with corneal thickness less than 500 μm. Similar
conclusions were drown by Özcura et al[11] in case of
patients with keratoconus (mean CCT in the examined group was 423.06±59.64 μm), which is
consistent with our study. It seems reasonable that the lower CCT, the larger
the difference between the two methods. Interestingly, for eyes with CCT
greater than 600 μm, high agreement between GAT and DCT IOP values
was observed in our study. The mean differences in IOP readings between both
methods were respectively lower. We hypothesize that in cases of corneas with
increased CCT due to decompensation or various dystrophies, both tonometry
methods are comparable.
According to
the literature, CCT influences not only GAT measurements but also other
tonometry methods[3,9,11,15]. It has been observed that biomechanical parameters of
the cornea should be taken into consideration in IOP assessment. We considered
the effect of two corneal parameters (CCT and corneal curvature) on IOP
measurements in this study. Our observations have shown that CCT has a
significant influence on IOP measurement using three different tonometers in
groups of individuals with corneal thickness within normal limits and those
with CCT under 600 μm. This observation has been previously reported by
other authors[3]. Of note,
IOP values measured by the RT method present the highest positive correlation
with CCT as described by Özcura et al[11,15]. On the
other hand, other reports that indicate that the CCT value does not impact DCT
measurements and offers an advantage of DCT over GAT[9-10,16-17]. Our study results show the CCT does not influence DCT
measurements exclusively in individuals with thick corneas, whereas IOP
readings positively correlate with CCT in eyes with corneal thickness within
normal limits. A similar observation was introduced by Francis et al[18] who described a correlation between DCT and CCT. It was
later confirmed that the influence of CCT on DCT measurement is weaker than for
GAT[19]. However, this phenomenon seems to diminish with
increase of CCT. Precise analyses revealed that the agreement between GAT and
DCT measurements increases in thicker corneas[18-21]. This
finding is consistent with our results where we concluded that DCT could be an
alternative for GAT in thicker corneas.
In this
study, no significant correlations were observed between corneal curvature and
tonometry findings in eyes with CCT less than 600 μm. This
finding is in concordance with the results of Özcura et al[15]. Similarly, Lanza et al[22] presented no
significant correlation between corneal curvature and all tonometry methods
analysed (GAT, DCT and RT). On the other hand, Salvetat et al[3] observed a
significant connection between corneal curvature and RT measurements for CCT
557.6±34.9 μm, while no correlation with GAT findings was noted.
Interestingly, we observed that in caseswith CCT greater than 600 μm, the
refractive power of the cornea (steep corneal curvature) had a significant
impact on GAT results. This finding could be attributed to increased hysteresis
and distribution of the tear film in steeper corneas[23]. In comparison, a positive correlation between corneal
curvature and GAT measurements as an independent factor influencing GAT
measurements has been described previously[24]. This finding served as a basis for recommendations of
double GAT measurements in cases of corneas with significant differences in the
corneal radius between flat and steep meridians[25]. Andreanos et al[9] observed a
significant difference between GAT and DCT, which was larger for flat corneas.
To
summarize, significantly higher IOP values are obtained by DCT than by GAT in
nonglaucomatous subjects. Accordingly, the lowest values were observed for RT.
The limitations of the RT are highly related with CCT values in patients with
CCT within normal limits. In contrast, the corneal curvature has no impact on
IOP measurements assessed by different tonometry techniques in case of individuals
with CCT under 600 μm. The ophthalmologist needs be aware of the impact
of corneal parameters on the IOP measurement technique and should take it into
consideration for both diagnostics and monitoring. The individualized approach
for the patient seems reasonable.
ACKNOWLEDGEMENTS
Authors’
contributions: Zakrzewska A performed data acquisition, data analysis
and literature search. Zakrzewska A is responsible for manuscript preparation
and editing. Wiącek MP performed data analysis, statistical analysis and
literature search. Wiącek MP took an active part in preparation and editing of
the manuscript. Machalińska A gave the concept of this research, and is
responsible for its’ design. Machalińska A performed data analysis, literature
search, and is responsible for preparation, editing and review of the
manuscript. Machalińska A is also a supervisor of this research.
Conflicts of Interest: Zakrzewska
A, None; Wiącek MP, None; Machalińska
A, None.
REFERENCES