
·Investigation·
Indications
for penetrating keratoplasty and anterior lamellar keratoplasty during
2010-2017
Xiao-Tong Sun, Hua-Lei Zhai, Jun Cheng, Qian-Qian Kong,
Lin Cong, Lin Li, Wen-Pei Hao
Qingdao Eye Hospital of Shandong
First Medical University, Shandong Eye Institute, Shandong Provincial Key
Laboratory of Ophthalmology-State Key Laboratory Cultivation Base, Qingdao
266071, Shandong Province, China
Correspondence to: Hua-Lei Zhai. Qingdao Eye Hospital
of Shandong First Medical University, 5 Yan’erdao Rd, Qingdao 266071, Shandong
Province, China. zhaihualei0001@126.com
Received:
Abstract
AIM: To review the indications of penetrating keratoplasty (PK) and anterior
lamellar keratoplasty (ALK) at Qingdao Eye Hospital, Shandong Eye Institute,
Qingdao, China, from 2010 to 2017.
METHODS: The data of all patients undergoing PK or ALK from
January 2010 to December 2017 was retrospectively reviewed, with the
indications during 2010-2013 and 2014-2017 compared.
RESULTS: A total of 1869 eyes were included, among which 1405
eyes (75.2%) had PK and 464 eyes (24.8%) had ALK. The leading indications were
suppurative keratitis (36.8%), keratoconus (15.5%), herpes keratitis (13.1%),
and regraft (10.5%). In eyes undergoing PK, the top four indications were
suppurative keratitis (38.7%), herpes keratitis (15.3%), keratoconus (12.6%),
and regraft (12.5%) during 2014-2017, with the proportion of suppurative
keratitis and herpes keratitis decreased while regraft and keratoconus
increased compared with 2010-2013. In eyes with ALK, suppurative keratitis
(30.8%), keratoconus (24.1%), corneal dystrophies and degenerations (10.6%),
and corneal dermoid tumor (9.7%) were the top four indications, and there was
no significant difference for the proportion of each indication between
2010-2013 and 2014-2017.
CONCLUSION: Suppurative keratitis is the most common indication
for PK and ALK at Qingdao Eye Hospital during 2010-2017, followed by
keratoconus, herpes keratitis, and regraft. In eyes treated with PK, the
proportion of suppurative keratitis and herpes keratitis decrease while regraft
and keratoconus increase during 2014-2017 compared with 2010-2013.
KEYWORDS: penetrating keratoplasty; anterior
lamellar keratoplasty; indications
DOI:10.18240/ijo.2019.12.10
Citation: Sun
XT, Zhai HL, Cheng J, Kong QQ, Cong L, Li L, Hao WP. Indications for
penetrating keratoplasty and anterior lamellar keratoplasty during 2010-2017.
Int J Ophthalmol 2019;12(12):1878-1884
INTRODUCTION
Corneal transplantation, also called
keratoplasty, has become the most frequently performed type of
transplantation since the first successful keratoplasty in human being was
reported by Zirm in 1905[1].
Penetrating keratoplasty (PK), a procedure with full-thickness replacement of
the cornea, predominated for more than half a century[2-4]. However, some studies demonstrated that the long-term
corneal graft survival rates following PK were unsatisfactory, which was
attributed mainly to the endothelial immunological allograft rejection and the
continual loss of endothelial cells of the donor corneas[2-3]. This explains why anterior lamellar keratoplasty
(ALK), especially deep anterior lamellar keratoplasty (DALK), has increasingly
been valued in recent years[5].
ALK can preserve the healthy corneal endothelium in cases of keratopathy with the
endothelium uninvolved and thus eliminate the risk of endothelial rejection[6].
The indications for PK and ALK vary
by geographic regions along with economic development and social conditions. In
USA and Europe, keratoconus and corneal edema after cataract surgery were
reported as the leading indications for PK, and ulcerative keratitis was the
major indication for ALK[7-11]. However,
suppurative keratitis and corneal scarring were the leading indications for PK[12-15], and corneal burns and
suppurative keratitis were the dominant indications for ALK[14,16] in some developing countries.
In this study, we reviewed the data
of patients who underwent PK or ALK at Qingdao Eye Hospital, Shandong Eye
Institute, China from 2010 to 2017, with the indications compared between
2010-2013 and 2014-2017.
SUBJECTS AND METHODS
Ethical Approval This study was approved by the
Institutional Review Board of Shandong Eye Institute and conducted in
accordance with the tenets of the Declaration of Helsinki. Informed consent was
obtained from all patients. The medical charts of all patients undergoing PK or
ALK at Qingdao Eye Hospital, Shandong Eye Institute from January 2010 to
December 2017 were retrospectively analyzed. Data of patients, including age,
sex, surgical techniques, and preoperative primary diagnosis, were reviewed.
Diagnostic Categories of Primary
Diseases The diagnoses of diseases for
keratoplasty were divided into 11 categories[14]: suppurative keratitis,
keratoconus, regraft, herpes keratitis, corneal dystrophy and degeneration,
bullous keratopathy, corneal dermoid tumor, corneal scar, corneal burn,
immunologic disorders of the cornea, and others. According to the different
pathogens, suppurative keratitis was further classified into fungal keratitis,
bacterial keratitis, acanthamoeba keratitis, and keratitis with unclear
pathogens. Herpes keratitis included herpes simplex keratitis and herpes zoster
keratitis. Corneal scars included the legacy after a variety of keratitis
(except herpes keratitis), adhesive corneal leucoma, stable corneal scars after
trauma, congenital corneal leucoma, and unexplained corneal opacity. Corneal
burns included chemical burns and thermal burns.
Indication Selection for Penetrating
Keratoplasty or Lamellar Keratoplasty The surgical selection for PK or ALK was
made as follows. PKs were chosen for patients with corneal full-thickness
perforation[17]
or lesions involving Descemet’s membrane (DM) and corneal endothelial layers.
As for the lesions with DM and endothelial layers uninvolved, ALKs were first
chosen, and PK would also be performed when the posterior stroma in proximity
to DM was involved in inflammatory infiltration, especially for some patients
with suppurative keratitis to reduce the risk of recurrence. For keratoconus,
PKs were chosen if there were deep posterior corneal scarring, prior hydrops
with discontinuity in DM, post-PK regrafting, and for the cases with high-steep
average corneal curvature >65 diopter, and ALKs were considered for the
other eyes. ALKs were chosen for patients with corneal dermoid tumor, and ALK
would be transferred to PK only in the cases with the occurrence of corneal
perforation during surgery.
Statistical Analysis SPSS software version 25.0 was used
for statistical analysis. The proportion of indications in keratoplasties,
including PK and ALK, during 2010-2013 and 2014-2017 were analyzed using the
Chi-square test. A P-value of less than 0.05 was considered
statistically significant.
RESULTS
A total of 1869 patients, including
1273 males (68.1%) and 596 females (31.9%) were involved, with a ratio of
2.14:1. The age of patients was from 4mo to 84 years old. PK was performed in
1405 cases (75.2%) and ALK in 464 cases (24.8%; Figure 1). Over the 8y from
2010 through 2017, the leading indications for keratoplasties were suppurative
keratitis (687 cases, 36.8%), keratoconus (289 cases, 15.5%), herpes keratitis
(244 cases, 13.1%), and regraft (197 cases, 10.5%; Table 1).
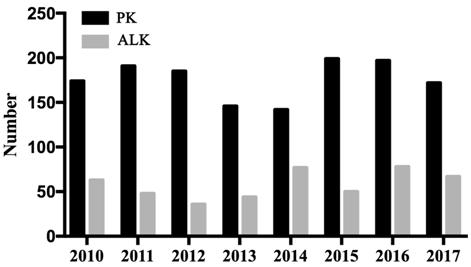
Figure 1 The annual number of PK and
ALK from 2010 to 2017.
Table 1 Indications for keratoplasty
during 2010-2013 and 2014-2017
n (%)
|
Indication |
Time period |
χ2 |
P |
|
|
2010-2013 |
2014-2017 |
|||
|
Suppurative keratitis |
379 (42.7) |
308 (31.4) |
25.889 |
|
|
Keratoconus |
113 (12.7) |
176 (17.9) |
9.578 |
|
|
Herpes keratitis |
131 (14.8) |
113 (11.5) |
11.018 |
|
|
Regraft |
65 (7.3) |
132 (13.4) |
18.475 |
|
|
Bullous keratopathy |
69 (7.8) |
50 (5.1) |
5.646 |
|
|
Corneal dystrophies and
degenerations |
51 (5.7) |
66 (6.7) |
0.749 |
0.387 |
|
Corneal scar |
27 (3.0) |
32 (3.3) |
0.070 |
0.791 |
|
Immunologic disorders of the
cornea |
20 (2.3) |
31 (3.2) |
1.429 |
0.232 |
|
Corneal dermoid tumor |
14 (1.6) |
31 (3.2) |
4.942 |
|
|
Corneal burn |
6 (0.7) |
33 (3.4) |
16.433 |
|
|
Others |
12 (1.4) |
10 (1.0) |
0.448 |
0.503 |
|
Total |
887 (100) |
982 (100) |
|
|
aP<0.05.
Indications for Keratoplasties The proportion of suppurative keratitis
in the indication for keratoplasties declined from 42.7% during 2010-2013 to
31.4% during 2014-2017 (χ2=25.889, P=0.000; Table 1).
Among the suppurative keratitis, fungal infection (499 cases, 72.6%) was much
more than bacterial (72 cases, 10.5%) and amoebic infections (28 cases, 4.1%;
Table 2). There was no statistical difference in the proportion of fungal
keratitis, bacterial keratitis and amoebic keratitis between 2010-2013 and 2014-2017.
The proportion of unclear pathogens declined significantly from 15.6% during
2010-2013 to 9.4% during 2014-2017 (χ2=5.757, P=0.016;
Table 2).
Table 2 Suppurative keratitis as
indication for keratoplasty during 2010-2013 and 2014-2017 n (%)
|
Indications |
Time period |
χ2 |
P |
|
|
2010-2013 |
2014-2017 |
|||
|
Fungal keratitis |
273 (72.0) |
226 (73.4) |
0.155 |
0.694 |
|
Bacterial keratitis |
32 (8.4) |
40 (13.0) |
3.739 |
0.053 |
|
Amoebic keratitis |
15 (4.0) |
13 (4.2) |
0.030 |
0.862 |
|
Unclear pathogen |
59 (15.6) |
29 (9.4) |
5.757 |
|
|
Total |
379 (100) |
308 (100) |
|
|
aP<0.05.
PK or ALK was performed in 289
patients (15.5%) with keratoconus from 2010 through 2017, which was the third
indication of keratoplasties during 2010-2013 and increased to the second place
during 2014-2017 (χ2=9.578, P=0.002; Table 1). There
were 244 patients (13.1%) with herpes keratitis undergoing PK or ALK, which was
the second indication during 2010-2013 and decreased to the fourth place during
2014-2017 (χ2=11.018, P=0.001; Table 1).
As the fifth indication during
2010-2013 and increased to the third indication during 2014-2017 (χ2=18.475,
P<0.001; Table 1), regrafts were performed for 197 patients (10.5%). The
indications for regrafts were graft endothelial dysfunction (61 cases, 31.0%),
graft ulceration (54 cases, 27.4%), graft opacities (33 cases, 16.8 %),
recurrence of the primary diseases (31 cases, 15.7%), and others (18 cases,
9.1%).
Moreover, there were 119 patients
(6.4%) with bullous keratopathy treated by PK, which was the fourth indication
during 2010-2013 and decreased to the sixth place during 2014-2017 (χ2=5.646,
P=0.017; Table 1). The proportions of corneal dermoid tumor (χ2=4.942,
P=0.026; Table 1) and corneal burns (χ2=16.433, P<0.001;
Table 1) increased during 2014-2017 compared with 2010-2013. There was no
statistical difference for the proportion of the other indications during the
two time periods (Table 1).
The proportions of PK and ALK in the
top four indications during 2010-2013 and 2014-2017 are shown in Figure 2. The
proportion of PK in suppurative keratitis (Figure
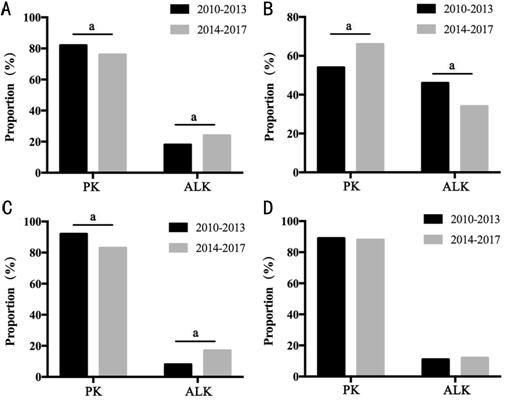
Figure 2 Proportion of PK and ALK in
the top four indications for keratoplasty during 2010-2013 and 2014
Indications for Penetrating
Keratoplasty Suppurative keratitis (544 cases,
38.7%) was the leading indication for PK, followed by herpes keratitis (215
cases, 15.3%), keratoconus (177 cases, 12.6%), regraft (175 cases, 12.5%),
bullous keratopathy (119 cases, 8.5%), corneal dystrophies and degenerations
(68 cases, 4.8%), corneal scar (47 cases, 3.3%), corneal burn (25 cases, 1.8%),
immunologic disorders of the cornea (18 cases, 1.3%), and others (17 cases,
1.2%). Among the top four indications of PK, the proportions of suppurative
keratitis (χ2=20.683, P<0.001) and herpes keratitis
(χ2=4.615, P=0.032) decreased during 2014-2017
compared with 2010-2013 (Table 3). Conversely, the percentages of regraft (χ2=21.493,
P=0.000) and keratoconus (χ2=18.408, P=0.000)
increased during 2014-2017 compared with 2010-2013 (Table 3).
Table 3 Indications for PK during 2010-2013
and 2014-2017
n (%)
|
Indications |
Time period |
χ2 |
P |
|
|
2010-2013 |
2014-2017 |
|||
|
Suppurative keratitis |
311 (44.7) |
233 (32.9) |
20.683 |
|
|
Herpes keratitis |
121 (17.4) |
94 (13.3) |
4.615 |
|
|
Keratoconus |
61 (8.8) |
116 (16.4) |
18.408 |
|
|
Regraft |
58 (7.3) |
117 (16.5) |
21.493 |
|
|
Bullous keratopathy |
69 (7.8) |
50 (7.1) |
3.710 |
0.054 |
|
Corneal dystrophies and
degenerations |
33 (5.7) |
35 (4.9) |
0.029 |
0.865 |
|
Corneal scar |
21 (3.0) |
26 (3.7) |
0.459 |
0.498 |
|
Corneal burn |
6 (0.7) |
19 (2.7) |
6.640 |
|
|
Immunologic disorders of the
cornea |
6 (2.3) |
12 (1.7) |
1.915 |
0.166 |
|
Others |
10 (1.4) |
7 (1.0) |
0.594 |
0.441 |
|
Total |
696 (100) |
709 (100) |
|
|
aP<0.05.
Indications for Anterior Lamellar
Keratoplasty The top four indications for ALK was
suppurative keratitis (143 cases, 30.8%), keratoconus (112 cases, 24.1%),
corneal dystrophies and degenerations (49 cases, 10.6%), and corneal dermoid
tumor (45 cases, 9.7%). Due to the small numbers of corneal scarring and
corneal burns, they were categorized into the others when performing
statistical analyses. There was no statistical difference for the proportion of
each indication between 2010-2013 and 2014-2017 (Table 4).
Table 4 Indications for ALK during
2010-2013 and 2014-2017
n (%)
|
Indications |
Time period |
χ2 |
P |
|
|
2010-2013 |
2014-2017 |
|||
|
Suppurative keratitis |
68 (35.6) |
75 (27.5) |
3.483 |
0.062 |
|
Keratoconus |
52 (27.2) |
60 (22.0) |
1.690 |
0.194 |
|
Corneal dystrophies and
degenerations |
18 (9.4) |
31 (11.3) |
0.444 |
0.505 |
|
Corneal dermoid tumor |
14 (7.3) |
31 (11.3) |
2.079 |
0.149 |
|
Immunologic disorders of the
cornea |
14 (7.3) |
19 (7.0) |
0.023 |
0.879 |
|
Herpes keratitis |
10 (5.2) |
19 (7.0) |
0.570 |
0.450 |
|
Regraft |
7 (3.7) |
15 (5.5) |
0.833 |
0.361 |
|
Others |
8 (4.2) |
23 (8.4) |
3.235 |
0.072 |
|
Total |
191 (100) |
273 (100) |
|
|
DISCUSSTION
Keratoplasty, including PK, ALK, and
endothelial keratoplasty (EK), was the main method for visual rehabilitation
once disease has affected corneal clarity. PK was the most popular keratoplasty
for the treatment of corneal diseases with stroma or endothelial cells involved[4]. The reasons lie in
there was no corneal lamellar interface problems, the surgical technique of PK
was relatively undemanding, and the corneal lesions could be cleared more
easily than ALK, especially in some cases with corneal infections such as
fungal or bacterial keratitis, and thus PK could greatly decrease the risk of
infection recurrence[4].
Compared with PK, ALK leaves the healthy endothelium of the recipient cornea
intact, which decreases the rate of postoperative endothelial rejection,
endothelial loss and subsequent regraft[18]. EK preserves the corneal epithelia,
most or all stroma and corneal nerves, so postoperative immune rejection and
ocular surface complications are rare[19]. In addition, EK provides faster and more predictable
visual rehabilitation and allows patients to resume daily activities sooner[19]. EK has now been
a popular surgery for the treatment of Fuchs dystrophy[8] and endothelial decompensation[10]. Therefore, there
are advantages and disadvantages for different form of keratoplasties, and to
choose PK, ALK, or EK according to the characteristics of keratopathies can
minimize the complications of corneal transplantation.
Only PKs and ALKs are included in
this study, while EK is not included, and the reason mainly lies in that EK is
only used to treat endothelial keratopathies, whose indication was quite
different from that for PK and ALK. The indications for PK and ALK are
keratopathies with corneal stroma involved. In addition, the number of EK
performed at our hospital is still quite limited, with the dominating reason
being the shortage of enough high-quality donor grafts. There are no pre-cut
donor grafts for EKs offered by eye banks, and the donor grafts have to be prepared
during the surgery of EKs. Unavoidably, there will be additional loss in the
number of corneal donors during the procedure of preparing for the donor
grafts. Therefore, EKs was only performed when there are enough high-quality
corneal donors at our hospital, and some patients with endothelial dysfunction
and obvious stromal edema were performed PK but not EK.
There are some discrepancies in the
indications for PK and ALK between the developed and developing countries. In
this study, the data of indications for PK and ALK from 2010 to 2017 were
reviewed, with the indications compared between time periods of 2010-2013 and
2014-2017. Suppurative keratitis was shown to be the leading indication for
keratoplasties during 2014-2017, followed by keratoconus, herpes keratitis, and
regraft, and they accounted for 75.9% in the preoperative indications. In
patients undergoing PK, the top four indications were suppurative keratitis,
herpes keratitis, keratoconus, and regraft, while in patients receiving ALK,
the leading indications were suppurative keratitis, keratoconus, corneal
dystrophies and degenerations, and corneal dermoid tumor.
The proportion of suppurative
keratitis in keratoplasties decreased during 2014-2017 compared with that
during 2010-2013. Suppurative keratitis was the top indication for both PK and
ALK, with the main surgical purpose of eliminating pathogens and controlling
infection. The results are consistent with the report from India[12] and the previous
data from our hospital[13-14]. As the biggest
developing country, there are a large number of farmers and workers in China,
and ocular injuries in labor lead to the high incidence of corneal infection[13-14]. In addition, when some patients
with suppurative keratitis were referred to our hospital, severe corneal
infection and even corneal perforation had occurred due to the previous delayed
diagnosis and improper treatments, which can explain why suppurative keratitis
was the top indication for keratoplasties in this study.
During 2014-2017, there was an
increase for ALK but a decline for PK in the treatment of suppurative keratitis
compared with 2010-2013 (Figure
The proportion of keratitis with
unclear pathogens declined from 15.6% during 2010-2013 to 9.4% during
2014-2017, and the difference was statistically significant. The result was
related to the improvement of laboratory diagnostic techniques and application
of confocal microscopy in recent years, which have greatly increased the
accuracy in the diagnosis of suppurative keratitis with definite pathogens at
our hospital. However, there was no significant difference in the proportion of
fungal keratitis, bacterial keratitis, and amoebic keratitis between the
periods of 2014-2017 and 2010-2013.
Keratoconus was shown as the second
indication for keratoplasties in our series, with a proportion increasing from
12.7% during 2010-2013 to 17.9% during 2014-2017, and the difference was
statistically significant. Keratoconus was reported as the dominating
indication for PK and ALK in some developed countries, such as New Zealand
(41.7%)[8],
Italy (45.1%)[10],
and Arabia (53.1%)[21].
The difference can be attributed to the discrepancies in agricultural and economic
status between the developing and developed countries.
Keratoconus increased from the third
indication for keratoplasties during 2010-2013 to the second place during
2014-2017. The difference in the proportion of keratoconus in PK was
statistically significant but insignificant in ALK. PK had been considered as
the gold standard for the treatment of advanced keratoconus for decades owing
to its safety and good visual acuity outcomes[6]. In our hospital, PKs were
usually preferred for eyes with the mean corneal curvature more than 65
diopters. However, ALK, especially DALK, has become increasingly popular since
it keeps the healthy endothelium of the recipient cornea intact so as to
eliminate endothelial rejection after surgery and prevent postoperative
endothelial loss and subsequent graft failure[22-24]. Several studies have documented that the surgical
effect of DALK is inferior to that of PK[25-26]. Visual outcomes after DALK were comparable with those
after PK[6,18,27]. In a Meta-analysis[22], PK was found to
achieve better visual acuity by calculating best corrected visual acuity. In
this study, an increase in the number of PK and a decline of LK in the
treatment of keratoconus were shown during 2014-2017 compared with 2010-2013.
This may be related to the high proportion of advanced keratoconus patients
with high-steep corneal curvature.
Herpes keratitis was reported as a
major cause of keratoplasty in the previous reports from our hospital[13-14]. In the current study, the
proportion of herpes keratitis in indications for keratoplasties declined from
14.8% during 2010-2013 to 11.5% during 2014-2017, and the difference was
statistically significant. This may be due to the increased number of effective
antiviral agents available for herpes keratitis, so keratoplasties were
eventually avoided for many patients. The proportion of herpes keratitis in PK
procedures decreased during 2014-2017 (13.3%) compared with 2010-2013 (17.4%).
Besides PK, ALK is an alternative and safe procedure for the treatment of
herpes keratitis in patients with the healthy endothelium[28-29], which contributed to the increase of ALK and decrease
of PK in the treatment of herpes keratitis in this study.
There were 196 patients (10.5%) who
underwent regraft, with a similar proportion in keratoplasties from USA
(11.3%-18.0%)[7],
Canada (17.1%)[30],
Italy (11.8%)[10]
and France (13.6%)[11].
In this study, regraft was the fifth indication during 2010-2013 and increased
to the third place in 2014-2017, which is related with the large number of
patients with keratoplasties in the previous years. The difference in the
proportion of regraft was statistically significant in PK between the two time
periods but not significant in ALK.
Endothelial dysfunction (31.0%) was
the dominating reason for regraft, which was similar to the reports from other
countries[31-33]. Graft ulcer
(27.4%) was another important cause of regraft. The ability of corneal grafts
to resist infection is lower than that of a native cornea, which leads to the
occurrence of corneal ulcer after keratoplasty, and some patients failing in
medical treatment had to be regrafted. Moreover, graft opacities (16.8 %) and
recurrence of the primary diseases (15.7%) were also important reasons for
regraft.
In summary, suppurative keratitis
was the leading indication for keratoplasties at Qingdao Eye Hospital from 2010
through 2017, followed by keratoconus, herpes keratitis, and regraft. In
patients treated by PK, there was a decline in the proportion of suppurative
keratitis and herpes keratitis but an increase in keratoconus and regraft
during 2014-2017 compared with 2010-2013. However, there is no statistically
significant difference in the proportion of indications for LK between the two
time periods.
ACKNOWLEDGEMENTS
The authors thank Ping Lin, MTI, for
her linguistic and editorial assistance.
Foundations: Supported by the National Natural
Science Foundation of China (No.81500703); the Natural Science Foundation of
Shandong Province (No.ZR2015YL027); the Innovation Project of Shandong Academy
of Medical Sciences.
Conflicts of Interest: Sun XT, None; Zhai HL, None;
Cheng J, None; Kong QQ, None; Cong L, None; Li L,
None; Hao WP, None.
REFERENCES