
·Brief
Report·
IOL
repositioning using iris sutures: a safe and effective technique
Tomaso Caporossi, Ruggero Tartaro, Fabrizio GS Franco,
Francesco Barca, Lucia Finocchio, Daniela Bacherini, Dario Giorgio, Fabrizio
Giansanti, Stanislao Rizzo
Department of Surgical and
Translational Medicine, Eye Clinic, University of Florence, Azienda Ospedaliera
Universitaria Careggi, Florence 50314, Italy
Correspondence to: Ruggero Tartaro. Department of
Ophtalmology, University Hospital Careggi-Florence, Via Largo Palagi 1,
Florence 50139, Italy. ruggerotartaro@yahoo.it
Received:
Abstract
This retrospective
non-comparative consecutive case series study was conducted at Azienda
Ospedaliera Universitaria Careggi, Florence, Italy and describes a useful
intraocular lens (IOL) repositioning technique using iris sutures. In our
study, 41 consecutive cases of posteriorly dislocated IOLs were surgically
treated between January 2015 and May 2017. Six of the cases were post-traumatic
luxations, and 20 patients had pseudoexfoliation syndrome. All the patients
underwent pars plana vitrectomy and same IOL repositioning using iris sutures.
The mean follow-up was 12.2mo. The mean preoperative best corrected visual
acuity (BCVA) was 0.10±0.15 logMAR, whereas the mean postoperative BCVA was
0.08±0.14 logMAR. The mean postoperative BCVA did not change significantly from
the preoperative BCVA. The final mean spherical equivalent was -0.44±0.49 SD.
Three lenses (7.31%) were found tilted during post-operative follow-up. Two
eyes (4.87%) had postoperative cystoid macular edema. No eyes had
endophthalmitis, hypotony, retinal or choroidal detachment. The iris fixation
technique seems to be a safe and valid option for the management of dislocated IOLs.
KEYWORDS: IOL
luxation; pars plana vitrectomy; cystoid macular edema
DOI:10.18240/ijo.2019.12.21
Citation: Caporossi T, Tartaro R, Franco FGS,
Barca F, Finocchio L, Bacherini D, Giorgio D, Giansanti F, Rizzo S. IOL
repositioning using iris sutures: a safe and effective technique. Int J
Ophthalmol
2019;12(12):1972-1977
INTRODUCTION
Intraocular lens (IOL) luxation is a
rare and challenging complication and may be spontaneous or associated with traumas.
Untreated cases could develop chronic cystoid macular edema (CME), anterior
uveitis, or retinal detachment, as Faria et al[1]
showed. Surgery for IOL luxation is often challenging, and different techniques
have been described in the literature: scleral fixation, iris enclavation,
anterior chamber IOLs. Many surgeons decide to remove the previously implanted
IOL and carry out secondary implantation using anterior chamber IOLs, iris claw
IOLs, and scleral fixation IOLs; other surgeons use the same dislocated IOL
(either a three-piece IOL or a single piece IOL) suturing it to the iris. Our
study focuses on the efficacy and the safety of IOL repositioning using iris
sutures.
SUBJECTS AND METHODS
Ethical Approval This is a retrospective
non-comparative consecutive case series study. Institutional Review Board
(IRB)/Ethics Committee approval was obtained, and the study is following the
Declaration of Helsinki. All the patients signed informed consent to
participate in the study.
We operated 41 consecutive cases of
posteriorly dislocated IOLs between January 2015 and May 2017. All cases lacked
sufficient capsule support to allow sulcus placement alone. Six eyes had a
post-traumatic luxation, and 20 patients had pseudoexfoliation syndrome (PXS).
The patients with diabetes were not excluded except those with diabetic macular
edema. We had 2 diabetic patients, one of whom with iridodonesis. Moreover,
another non-diabetic patient had an iridodonesis.
All the patients underwent pars
plana vitrectomy (PPV) and IOL iris suturing by the same surgeon (Caporossi T).
The data collected included demographic information, details on cataract
extraction surgery, visual acuity, refraction, endothelial count, intraocular
pressure (IOP), ocular biometry (measured using the IOLMaster, Carl Zeiss
Meditec AG), information on fixation surgery, macular optical coherence
tomography (OCT) examination, assessment of the lens centering using anterior
segment OCT, and intraoperative and postoperative complications.
Surgical Technique All surgical procedures were
performed using a retrobulbar block with ropivacaine 10% and lidocaine 2%,
mixed in equal volumes and with hyaluronidase. The 25-gauge PPV (Alcon surgical
Inc.) commenced with core and peripheral vitrectomy, with careful attention to
freeing the IOL from the surrounding vitreous. In the case of capsular
remnants, they were removed with vitreoretinal forceps and vitrectomy probe;
when IOL was inside the capsular bag, a chandelier was placed to perform a
bimanual technique to remove the IOL from the bag with two vitreoretinal
forceps. Once freed from the vitreous and the bag the IOL was manipulated with
vitreoretinal forceps to obtain the right anterior to posterior orientation of
the optical plate. Then a 25-gauge light probe was placed in contact with the
central anterior part of the optical plate to lift the IOL above the iris
plane, where the IOL was engaged, then pupillary capture miosis was induced
with intracameral acetylcholine, followed by intracameral instillation of
dispersive viscoelastic (VISCOAT®, Alcon 5 surgical Inc.). Once the
haptic was stabilised, 2 vertical side-ports at 2 and 10 o’clock were
performed, and the lens was oriented horizontally for ease of suturing. While
raising the IOL upwards by pressing the optic plate with a light probe to
emphasize the haptic shape through the iris, a 10-0 polypropylene (Prolene®,
Ethicon) suture was then passed through the cornea side-port and the
mid-peripheral iris proximal to the haptic and then again through the iris
distal to the haptic and out through the cornea (Figure 1).
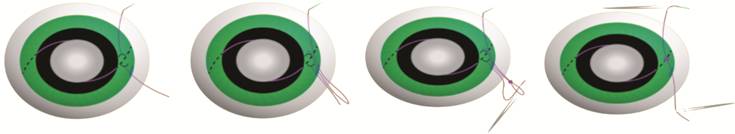
Figure 1 The IOL repositioning
technique.
With a vitreoretinal forceps, the
suture was conducted through the side-port to prepare a knot. The tip of a
clamp was rotated around the suture and then tied into the proximal end of the
suture. Another clamp was used to grab the distal end of the suture and then
pull it to tighten the slipknot. This manoeuvre was repeated three times. The
second haptic was sutured similarly to achieve a 2-point fixation. The
stability of the fixation was then assessed, and the optic plate was gently
pushed through the pupil into the posterior chamber. Iridectomy was performed
to reduce the possibilities of a post-operative pupillary block. The remnants
of VISCOAT® were removed from the anterior chamber and exchanged
with a balanced salt solution; the corneal limbal incisions were hydro-sutured.
A partial fluid-air exchange was performed, and the PPV trocars were removed.
Subtenon dexamethasone and tobramycin were administered.
Statistical Analysis For the statistical analysis, best
corrected visual acuity (BCVA) was converted from Snellen to logMAR.
Statistical analysis was performed using SPSS software version18.0 (SPSS, Inc.,
Chicago, IL, USA). The relationship between the preoperative and postoperative
BCVA was compared using paired and unpaired Student’s t-test. The
distributions for variables were expressed as a mean±standard deviation (SD).
Statistical significance was defined as P value <0.05.
RESULTS
Forty-one eyes of 41 consecutive
patients were included in this study. Mean age was 70.12±10.16y. The mean
follow-up was 12.2mo. Six of the cases were post-traumatic luxations, and 20
patients had PXS. In 2 eyes a capsular tension ring was found inside the bag
and was removed through the corneal side port. No IOL was changed during
surgery, and all the IOLs were sutured to the iris. The lens characteristics
were: n=6 mono-piece acrylic IOLs, n=27 3-pieces acrylic IOLs, n=8
mono-piece PMMA IOLs. The mean preoperative BCVA was 0.10±0.15 logMAR, whereas
the mean postoperative BCVA was 0.08±0.14 logMAR (Tables 1 and 2).
Table 1 Patient characteristics
(mono-piece IOL)
|
Patient |
Age |
PXS |
IOL type |
Capsular tension ring |
Preop. IOP |
Postop. IOP |
Preop. BCVA logMAR |
Postop. BCVA logMAR |
Postop. spherical refractive error |
Postop. cylindrical error |
|
4 |
55 |
No |
Acryilic mono-piece in the bag |
No |
11 |
17 |
0.10 |
0.10 |
0.00 |
0.50 |
|
5 |
45 |
No |
Acryilic mono-piece in the bag |
No |
10 |
15 |
0.00 |
0.00 |
-1.50 |
-1.00 |
|
7 |
76 |
No |
PMMA mono-piece in the sulcus |
No |
14 |
13 |
0.30 |
0.00 |
0.00 |
-1.50 |
|
12 |
76 |
No |
PMMA mono-piece in the sulcus |
No |
13 |
17 |
0.00 |
0.00 |
-1.00 |
0.50 |
|
14 |
55 |
No |
PMMA mono-piece in the sulcus |
No |
11 |
16 |
0.30 |
0.30 |
-1.00 |
0.00 |
|
15 |
67 |
No |
Acryilic mono-piece in the bag |
No |
12 |
18 |
0.00 |
0.00 |
-1.75 |
3.00 |
|
16 |
57 |
Yes |
Acryilic mono-piece in the bag |
No |
10 |
15 |
0.40 |
0.40 |
0.00 |
0.50 |
|
18 |
67 |
Yes |
PMMA mono-piece in the sulcus |
No |
14 |
13 |
0.10 |
0.00 |
0.00 |
2.00 |
|
23 |
65 |
No |
PMMA mono-piece in the sulcus |
No |
10 |
15 |
0.00 |
0.00 |
0.00 |
-1.50 |
|
24 |
67 |
No |
Acryilic mono-piece in the bag |
No |
12 |
15 |
0.10 |
0.10 |
-0.25 |
0.00 |
|
25 |
78 |
No |
PMMA mono-piece in the bag |
No |
13 |
15 |
0.00 |
0.00 |
0.00 |
2.00 |
|
28 |
65 |
No |
PMMA mono-piece in the bag |
No |
12 |
14 |
0.00 |
0.00 |
-0.50 |
0.50 |
|
35 |
67 |
No |
PMMA mono-piece in the bag |
No |
13 |
18 |
0.00 |
0.00 |
-0.25 |
-3.00 |
|
39 |
76 |
No |
Acryilic mono-piece in the bag |
No |
12 |
12 |
0.00 |
0.00 |
0.00 |
-0.25 |
|
Mean |
65.42 |
|
|
|
|
|
0.09 |
0.06 |
-0.45 |
0.13 |
Table 2 Patient characteristics
(3-pieces IOL)
|
Patient |
Age |
PXS |
IOL type |
Capsular tension ring |
Preop. IOP |
Postop. IOP |
Preop. BCVA logMAR |
Postop. BCVA logMAR |
Postop. spherical error |
Postop. cylindrical error |
|
1 |
65 |
0 |
Acrylic 3-pieces in the bag |
No |
15 |
18 |
0.10 |
0.10 |
0 |
0.5 |
|
2 |
67 |
No |
Acrylic 3-pieces in the bag |
No |
12 |
22 |
0.00 |
0.10 |
-0.5 |
-1 |
|
3 |
63 |
No |
Acrylic 3-pieces in the bag |
No |
12 |
14 |
0.10 |
0.00 |
0.5 |
-1 |
|
6 |
88 |
0 |
Acrylic 3-pieces in the bag |
Yes |
11 |
14 |
0.00 |
0.00 |
-1 |
0 |
|
8 |
83 |
0 |
Acrylic 3-pieces in the bag |
No |
11 |
13 |
0.30 |
0.00 |
0 |
-1 |
|
9 |
76 |
0 |
Acrylic 3-pieces in the bag |
No |
14 |
15 |
0.10 |
0.00 |
-1 |
0.5 |
|
10 |
74 |
0 |
Acrylic 3-pieces in the bag |
No |
12 |
15 |
0.50 |
0.50 |
0 |
-1.5 |
|
11 |
72 |
0 |
Acrylic 3-pieces in the bag |
No |
15 |
28 |
0.00 |
0.00 |
-1 |
-1.5 |
|
13 |
54 |
0 |
Acrylic 3-pieces in the bag |
No |
12 |
16 |
0.10 |
0.10 |
0.5 |
0 |
|
17 |
65 |
0 |
Acrylic 3-pieces in the bag |
Yes |
11 |
14 |
0.00 |
0.00 |
-0.75 |
0 |
|
19 |
87 |
0 |
Acrylic 3-pieces in the bag |
No |
11 |
11 |
0.50 |
0.50 |
1 |
-2 |
|
20 |
65 |
1 |
Acrylic 3-pieces in the bag |
No |
14 |
15 |
0.00 |
0.00 |
-0.5 |
0.5 |
|
21 |
45 |
1 |
Acrylic 3-pieces in the bag |
No |
12 |
14 |
0.30 |
0.30 |
2 |
0 |
|
22 |
75 |
0 |
Acrylic 3-pieces in the bag |
No |
11 |
15 |
0.00 |
0.00 |
-0.25 |
-0.25 |
|
26 |
76 |
0 |
Acrylic 3-pieces in the bag |
No |
12 |
12 |
0.00 |
0.00 |
-0.25 |
0.5 |
|
27 |
84 |
0 |
Acrylic 3-pieces in the bag |
No |
10 |
15 |
0.00 |
0.00 |
0 |
2 |
|
29 |
78 |
0 |
Acrylic 3-pieces in the bag |
No |
11 |
14 |
0.00 |
0.00 |
0 |
2 |
|
30 |
71 |
0 |
Acrylic 3-pieces in the bag |
No |
11 |
14 |
0.10 |
0.10 |
-0.5 |
0.5 |
|
31 |
65 |
1 |
Acrylic 3-pieces in the bag |
No |
14 |
15 |
0.00 |
0.00 |
0 |
-1.5 |
|
32 |
76 |
0 |
Acrylic 3-pieces in the bag |
No |
12 |
14 |
0.00 |
0.00 |
1 |
-0.25 |
|
33 |
84 |
0 |
Acrylic 3-pieces in the bag |
No |
14 |
18 |
0.00 |
0.00 |
0 |
-1 |
|
34 |
75 |
0 |
Acrylic 3-pieces in the bag |
No |
12 |
18 |
0.00 |
0.00 |
0.5 |
-1 |
|
36 |
76 |
0 |
Acrylic 3-pieces in the bag |
No |
11 |
12 |
0.30 |
0.30 |
-1 |
0 |
|
37 |
66 |
0 |
Acrylic 3-pieces in the bag |
No |
14 |
18 |
0.00 |
0.00 |
-0.5 |
2 |
|
38 |
78 |
1 |
Acrylic 3-pieces in the bag |
No |
12 |
15 |
0.00 |
0.00 |
-0.5 |
0 |
|
40 |
76 |
0 |
Acrylic 3-pieces in the bag |
No |
14 |
15 |
0.10 |
0.00 |
1 |
-0.25 |
|
41 |
75 |
0 |
Acrylic 3-pieces in the bag |
No |
15 |
15 |
0.30 |
0.30 |
0 |
-0.25 |
|
Mean |
72.55 |
|
|
|
|
|
0.10 |
0.09 |
-0.04 |
-0.14 |
In both mono-piece and 3-pieces group,
we have not found statistically significant differences between pre and postop
BCVA (P=0.212 and P=0.168 respectively). The differences between
postoperative BCVA in the patients with one-piece or 3-pieces IOL were not
statistically significant (P=0.682).
All eyes improved their uncorrected
visual acuity, 9 eyes (21.9%) had final BCVA of 20/20 (0 logMAR), and 38 eyes
(92%) had final postoperative BCVA better than 20/40 (>0.30 logMAR). The
mean postoperative spherical error was -0.18 diopters (D) ±0.71 SD. Three
lenses (7.31%) were found tilted during postoperative follow-up. One patient
(with a mono-piece-IOL) had lost the iris suture in one of the haptics and
later underwent a second operation to reposition it in the same position.
Another patient with a 3-piece acrylic IOL was found with a bent haptic, and he
then underwent an IOL change with a new 3- piece acrylic foldable IOL (AR40e®,
AMO surgical); the third patient maintained a tilted 3-pieces IOL with a final
BCVA of 20/40 (0.30 logMAR). Two eyes (4.87%) had postoperative CME that
affected visual acuity recovery: the first patient recovered with non-steroid
anti-inflammatory drug (NSAID) eye drops for 2mo; the second, after 2mo of
NSAID therapy with no change of CME, underwent Ozurdex (Allergan inc.)
implantation with good resolution of the CME and a final visual acuity
improvement after 3mo. The 2 diabetic patients did not develop CME. Two eyes
(4.87%) had postoperative vitreous bleeding: one had spontaneous resolution
after 2wk of observation, but the second needed a second PPV to resolve it.
Mean preoperative IOP was
Table 3 Postoperative complications
(mono-piece IOL)
|
Patient |
IOP elevation |
Iridocyclitis |
Cystoid macular edema |
Postop. IOL dislocation |
|
4 |
No |
No |
No |
No |
|
5 |
No |
No |
No |
No |
|
7 |
No |
No |
No |
No |
|
12 |
No |
No |
No |
No |
|
14 |
No |
No |
No |
No |
|
15 |
No |
No |
No |
Yes |
|
16 |
No |
No |
No |
No |
|
18 |
No |
No |
No |
No |
|
23 |
No |
No |
No |
No |
|
24 |
No |
No |
No |
No |
|
25 |
No |
No |
Yes |
No |
|
28 |
No |
No |
No |
No |
|
35 |
No |
No |
No |
No |
|
39 |
No |
No |
No |
No |
Table 4 Postoperative complications
(3-pieces IOL)
|
Patient |
IOP elevation |
Iridocyclitis |
Cystoid macular edema |
Postop. IOL dislocation |
|
1 |
No |
No |
No |
No |
|
2 |
Yes |
Yes |
No |
No |
|
3 |
No |
No |
No |
No |
|
6 |
No |
No |
No |
No |
|
8 |
No |
No |
No |
No |
|
9 |
No |
No |
No |
No |
|
10 |
No |
No |
No |
No |
|
11 |
Yes |
No |
No |
No |
|
13 |
No |
No |
No |
Yes |
|
17 |
No |
No |
No |
No |
|
19 |
No |
No |
No |
No |
|
20 |
No |
No |
No |
No |
|
21 |
No |
Yes |
Yes |
Yes |
|
22 |
No |
No |
No |
No |
|
26 |
No |
No |
No |
No |
|
27 |
No |
No |
No |
No |
|
29 |
No |
No |
No |
No |
|
30 |
No |
No |
No |
No |
|
31 |
No |
No |
No |
No |
|
32 |
No |
No |
No |
No |
|
33 |
No |
No |
No |
No |
|
34 |
No |
No |
No |
No |
|
36 |
No |
No |
No |
No |
|
37 |
No |
No |
No |
No |
|
38 |
No |
No |
No |
No |
|
40 |
No |
No |
No |
No |
|
41 |
No |
No |
No |
No |
In the mono-piece IOLs group, the
difference between the preoperative IOP and the postoperative IOP was
statistically significant (P<0.05). We had numerous cases of 1wk IOP
elevation although no ocular hypertension (defined as IOP>
In the 3-pieces IOLs group the
difference between the pre-operative IOP and the postoperative IOP were
statistically significant (P<0.05). We had numerous cases of one-week
IOP elevation although only in two cases we have ocular hypertension (22 and
DISCUSSION
In this retrospective study, we have
included cases of luxated IOLs where we performed the repositioning of the same
IOL using iris suture fixation. Our paper, compared to the article by Faria et
al[1], who has already described this
technique, has the added value that we have also used this technique in
one-piece IOLs. We have described and discussed the results in a differential manner
in the two groups mono-piece IOLs and 3-pieces IOLs. We have registered a BCVA
improvement and IOL stability in most of the patients. The management of a
luxated IOL is challenging, and surgeons have performed different techniques.
Anterior chamber IOLs are very simple to implant, but they could cause
secondary glaucoma, chronic inflammation or endothelial decompensation as Evans
et al[2], Kumar et al[3],
Kavuncu et al[4] and Neuhann et al[5] showed. Iris-claw lenses are often implanted but large
corneal incisions (about
Furthermore, the penetrating needle
through the iris stroma damages its microvascular structure causing
extravasation of inflammatory mediators. Cohen et al[17]
conducted a review of patients with CME following PPV for retained lens pieces
and revealed that 8% of eyes with a sulcus-fixated posterior chamber IOL
implanted after cataract extraction developed CME. In our study, we found only
2 cases (4.8%) of CME, in both of the cases it was resolved with medical
therapy. Comparing the latest reviews of scleral-sutured IOL outcome, CME has
been reported as an early postoperative complication between 6.4%-12% as
Lockington et al[18] and Sindal et al[19] respectively showed. However, when using anterior
chamber IOLs implants, that may be associated with IOP elevation and glaucoma
development, posterior-chamber iris sutured IOLs seem to be better tolerated.
In our series, we found only two patients with postoperative IOP elevation that
was resolved with topical therapy. Sindal et al[19]
wrote that, in literature, retinal detachments ware reported as a complication
in 4.5% of the patients that underwent a secondary IOL implantation. We had no
cases of retinal detachment in our study, in fact, we performed a careful
vitreous base shaving vitrectomy with triamcinolone staining to avoid vitreal
traction, which may cause the development of retinal tears, during the IOL
repositioning manoeuvres.
Furthermore, we performed argon
laser retinopexy in the case of retinal tears. Regarding the sulcus IOLs the
haptics are positioned in a virtual space between the anterior bag and the
posterior surface of the iris; moreover, the lack of fixation and the length of
the haptics, that in a mono-piece IOL hardly covers the white to white (WTW)
distance, facilitates the movement and the iris rubbing. However, by fixing the
IOL to the iris, we do have not only stabilisation of the IOL movements but
also an iris sphincter movement reduction with less shrinking of the iris
against the edge of the IOL haptics.
Furthermore, we had an expected
post-operative myopic error due to the more anterior position of the IOL: the
mean postoperative spherical equivalent was -0.44±0.49 SD. The more anterior
position of the lens caused a myopic shift, which was acceptable for all the
patients.
Faria et al[1]
published this technique before us, although they used only in the case of
3-pieces IOLs. Similarly to us, they had a myopic shift in all the patients.
Differently from us, they reported a higher percentage of ocular hypertension
(16.6%) and a case of postoperative hyphema. As in our paper, they[1] have not found any case of endothelial dysfunction or
synechiae. Conversely, they have not reported postoperative dislocation,
whereas we reported 3 cases (1 patient with a mono-piece IOL and 2 patients
with a 3-pieces-IOL). Differently, from Faria et al[1]
we have not found any retinal complications such as retinal detachment or
epiretinal membranes.
In conclusion, related to our report
the iris fixation technique seems to be a safe and valid option for the
management of luxated IOLs. In our experience the functional outcomes are
outstanding: we did not have intraoperative complications, endothelial
dysfunction, and pigment dispersion. We had IOL stability after 12.2mo, no
surgically-induced astigmatism increasing, and we experienced a definite
advantage of using the same IOL in a closed eye without new corneal incisions.
Our technique does not require large
corneal incisions, and for that, we found very encouraging visual and
refractive outcomes. We observed a small percentage of complications, which
were manageable. We also described mono-piece acrylic and PMMA IOL suturing to
the iris, and we reported good results concerning visual acuity and avoiding
complications.
ACKNOWLEDGEMENTS
Conflicts of
Interest: Caporossi T, None; Tartaro R, None; Franco FGS, None;
Barca F, None; Finocchio L, None; Bacherini D, None; Giorgio
D, None; Giansanti F, None; Rizzo S, None.
REFERENCES