·Letter
to the Editor·
The
application of ultra-wide-field fundus autofluorescence in early metastatic
choroidal tumor screening
Pan-Pan Ye1,2, Jia Xu1,2, Zhi-Tao
Su1,2, Xiao-Yun Fang1,2, Ke Yao1,2
1Eye Center, the Second Affiliated
Hospital, School of Medicine, Zhejiang University, Hangzhou 310009, Zhejiang
Province, China
2Eye Hospital, Zhejiang University,
Hangzhou 310009, Zhejiang Province, China
Correspondence to: Ke Yao. No.88 Jiefang Road, Second
Affiliated Hospital, School of Medicine, Zhejiang University, Hangzhou 310009,
Zhejiang Province, China. xlren@zju.edu.cn
Received: 2019-06-30
Accepted: 2019-09-18
DOI:10.18240/ijo.2019.12.22
Citation: Ye
PP, Xu J, Su ZT, Fang XY, Yao K. The application of ultra-wide-field fundus
autofluorescence in early metastatic choroidal tumor screening. Int J
Ophthalmol 2019;12(12):1978-1981
Dear Editor,
I am Dr. Ke Yao, from Eye Center,
the Second Affiliated Hospital, School of Medicine, Zhejiang University,
Hangzhou, China. I write to present three cases with metastatic choroidal tumor
using an ultra-wide-field scanning laser ophthalmoscope.
Metastatic choroidal tumor is the
most common intraocular malignancy and accounts for approximately 1%-8% of
patients with systemic malignancy[1-3].
It presents as the first sign of a systemic malignant tumor in up to a third of
patients with cancer. Most choroidal metastases locate posterior to the equator
of the retina and some in the peripheral retina. The tumor appears as a flat,
undetectable lesion at the early stage, and the patient may be asymptomatic. As
the tumor grows, it becomes an elevated and visible choroidal mass and may
result in serous retinal detachment and optic disc edema. Thus, an accurate and
prompt diagnostic method should be used in early choroidal metastasis screening
to avoid misdiagnosis and missed diagnosis.
The main methods o f detecting
choroidal tumor include ophthalmoscopic examination, ultrasonography (US),
optical tomography coherence (OCT), fundus fluorescein angiography (FFA), and
indocyanine green angiography (ICGA)[4]. However,
due to poor health conditions or allergic reactions, it is usually difficult to
perform FFA or ICGA in patients with systemic malignancy. Fundus
autofluorescence (FAF) captures lipofuscin autofluorescence in retinal pigment
epithelium (RPE) cells and provides a noninvasive image detection technique for
such patients[5-6]. An
ultra-wide-field scanning laser ophthalmoscope offers green wavelength imaging
for recording FAF, providing a good tool for detecting peripheral, slight, and
early lesions of metastatic choroidal tumor.
Case 1
A 61-year-old woman had complained of decreased
vision in her left eye for one month. She had been diagnosed with breast cancer
and undergone mastectomy four years earlier. Her best corrected visual acuity
(BCVA) was 0.8 in the
right eye and 0.1 in the left.
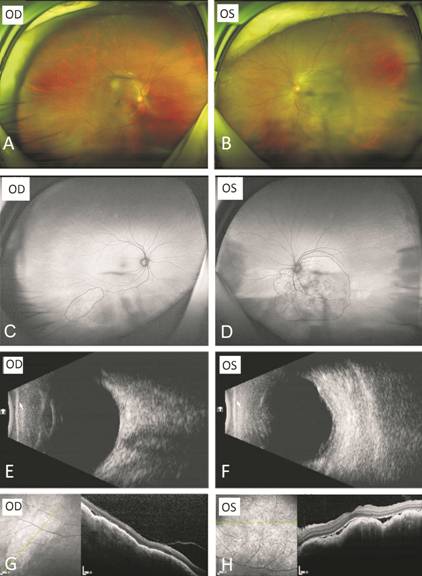
The ultra-wide-field retinal image showed a yellowish, irregular, flat mass in
the posterior pole of the retina, with an obscure boundary in the left eye and
no visible lesion in the right (Figure 1). The ocular B-ultrasound found an
irregular flat mass with a medium-to-high reflectivity beneath the posterior
pole of the retina in the left eye and no obvious positive sign in the right.
FAF found a mixture of hyper- and hypofluorescent dots in the central and
inferior midperiphery retina of the left eye. An oval lesion with a mixture of
hyper- and hypofluorescence was observed in the inferotemporal retina of the
right eye. OCT showed a dome-shaped elevation with a slight subretinal fluid
corresponding to the lesion in the left eye and a slight elevation in the right
eye. The patient was transferred to a tumor hospital for further treatment.
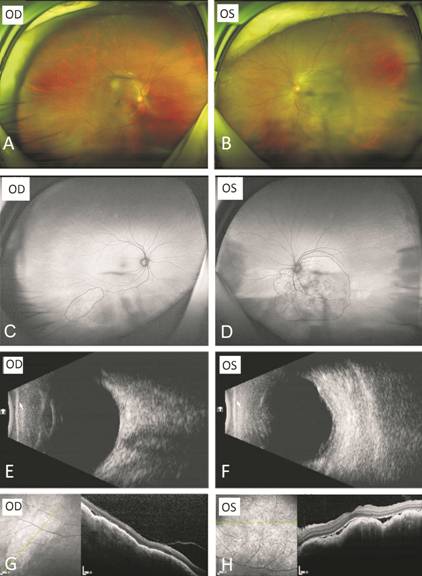
Figure 1 Ophthalmic findings in Case
1
A, B: An ultra-wide-field fundus photograph showed no
visible lesions in the right eye (A) and a yellowish, irregular, flat mass with
obscure boundary in the posterior pole of the retina in the left eye (B). C, D:
FAF found an oval lesion with a mixture of hyper- and hypofluorescence in the
inferotemporal retina of the right eye (C) and a mixture of hyper- and
hypofluorescent dots in the central and inferior midperiphery retina of the
left eye (D). E: B-ultrasound results of the right eye. F: B-ultrasound results
of the left eye revealed an irregular flat mass with a medium-to-high
reflectivity. G, H: OCT showed a slight elevation of the lesion in the right
eye (G) and a dome-shaped elevation with slight subretinal fluid corresponding
to the lesion in the left eye (H).
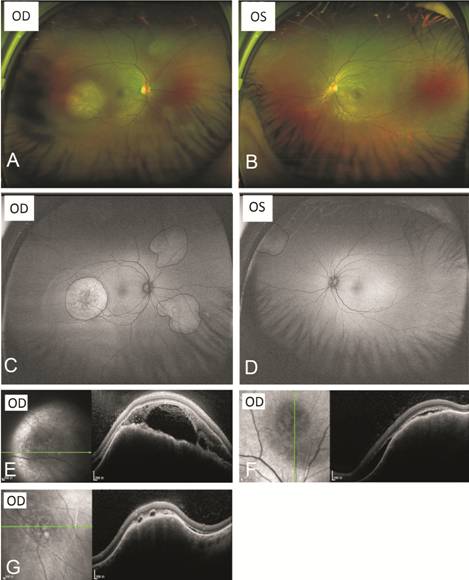
Case 2 A 35-year-old woman had complained of blurred vision
in her right eye for 10d. She had suffered from systemic lupus erythematosus
for nine months. Since then, she had taken steroids on doctor’s orders. Her
BCVA was 1.0 in both
eyes. Three lesions were found by the ultra-wide-field retinal image: one pale
yellow lesion with white dots in the temporal part of the macula, one in the
superonasal quadrant, and one in the inferonasal quadrant of the retina (Figure
2). FAF showed the macular lesion was a hyperfluorescent plaque with central
hypofluorescent dots, and the other two were hyperfluorescent in the right eye.
A hyperfluorescent lesion was also found in the superonasal quadrant of the
left eye. The patient had no previous history of diagnosed tumor. OCT revealed
a dome-shaped elevation of the choroidal tumor and subretinal fluid with
hyper-reflective foci in the right eye. However, OCT failed to detect the
lesion in the left eye because it was too peripheral. Because of these
findings, a metastatic choroidal tumor was suspected, and a systemic
examination found non-small-cell lung cancer with metastasis to the lymph
nodes.
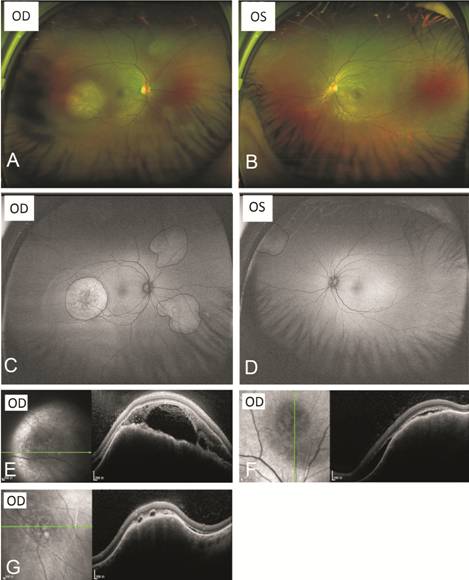
Figure 2 Ophthalmic findings in Case
2 A, B: An ultra-wide-field image found three lesions
in the right eye (A) and an obscure lesion in the left eye (B). C: FAF showed
the macular lesion was a hyperfluorescent plaque with central hypofluorescent
dots, and the other two were hyperfluorescent in the right eye. D: FAF found a
hyperfluorescent lesion in the superonasal quadrant of the left eye. E-G: OCT
revealed a dome-shaped elevation with subretinal fluid in correspondence to the
three lesions in the right eye.
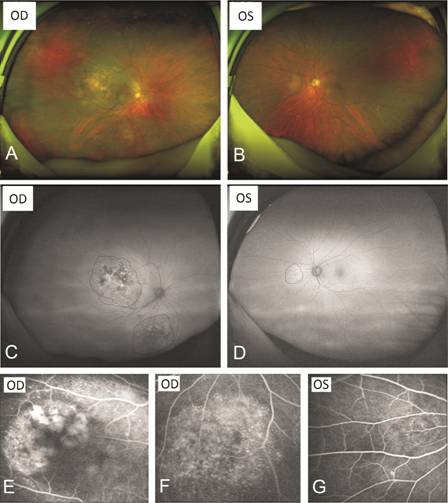
Case 3 A 71-year-old woman was referred for decreased vision
with metamorphopsia in her right eye for one month. She had had pulmonary
nodules for one year. Her BCVA was 0.2 in
the right eye and 1.0 in the
left. Two lesions were found in the right eye: one dome-shaped choroidal mass
in the posterior pole and one in the inferior retina (Figure 3). The posterior
lesion was found to be isoechoic by B-ultrasound. One lesion was also found in
the nasal retina of the left eye. The ultra-wide-field FAF showed that the
lesions in the right eye were interphase masses with hyper- and
hypofluorescence and that the lesion in the left eye was a hyperfluorescent
patch. FFA showed hypofluorescence in the early phase and hyperfluorescence
with pinpoints and leakage areas on the masses in the late phase. Because of
these findings, metastatic choroidal tumor was suspected, and a systemic
examination was performed. A pulmonary biopsy confirmed lung adenocarcinoma,
and the patient underwent pneumonectomy and chemotherapy.
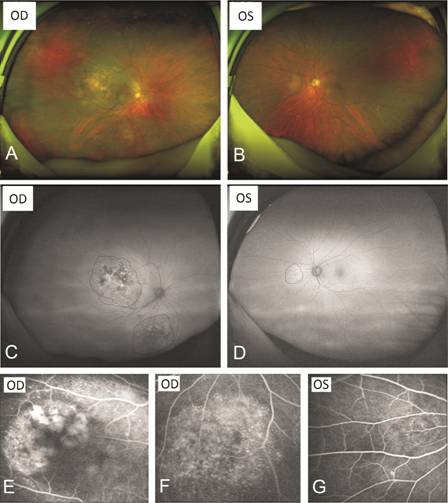
Figure 3 Ophthalmic findings in Case
3
A: An ultra-wide-field image of the right eye showed
one dome-shaped choroidal mass in the posterior pole and one in the inferior
retina. B: An ultra-wide-field image of the left eye found a lesion in the
nasal retina. C, D: Ultra-wide-field FAF revealed that the lesions in the right
eye were interphase masses with hyper- and hypofluorescence (C) and that the
lesion in the left eye was a hyperfluorescent patch (D). E-G: FFA showed
hyperfluorescent in the late phase, with pinpoints and leakage areas on the
lesions.
DISCUSSION
The clinical diagnosis tools for
choroidal metastasis have improved over decades, including fundoscopy, US, FFA,
ICGA and OCT. FFA and ICGA, particularly ultra-wide-field angiography, play an
important role in the differential diagnosis of choroidal tumor. Case 1 and
Case 2 patients had positive reaction to sodium fluorescein skin test and
therefore could not receive FFA examination. OCT provides useful information
for tumor morphology and has the advantage in detecting small choroidal lesions
before they are clinical visible[4]. The OCT
characteristics of choroidal metastasis include irregular anterior surface of
lesion, subretinal fluid and choriocapillaris compression[4].
FAF imaging is a rapid, noninvasive
technique that can evaluate photoreceptor and RPE cells function[7-8]. It can be used to detect
lipofuscin and other fluorophores. Reduced FAF indicates a dysfunction of
photoreceptors or RPE cells, whereas increased FAF implies the abnormal
accumulation of fluorophores. In normal eye, it shows a diffuse background
autofluorescence; normal macula appears a decreased autofluorescene with the
intensity being the least at the fovea due to the blockage by luteal pigments
such as lutein and zeaxanthin; the optic disc appears dark owing to the absence
of autofluorescent material while the retinal vessels show dark due to the
absorption of light by the pigments of the blood[9].
It was found that the abnormal accumulation of lipofuscin could be secondary to
damaged lysosomal activity with incomplete degeneration[7-8]. In these cases, the flat, early lesions showed
uniformly hyperfluorescent in the FAF pattern, and the larger, dome-shaped ones
showed hyperfluorescent interphased with hypofluorescence. A possible
explanation is that lipofuscin accumulation in the early stage leads to
hyperfluorescence and, after a period of time, the dysfunctional photoreceptor
or RPE cells cause the decreased autofluorescence. The results were consistent
with previous reports[5-7].
The Optos Tx200 ultra-wide-field
imaging device can capture up to 200 degrees of retina (approximately 82% of
the retinal area) in one image[10]. Patients with
peripheral lesion usually have no complaints regarding visual function until
the lesions grow and invade the macular area. Also, the lesion in the
peripheral retina is easily overlooked with a normal color fundus pattern and
can not be readily scanned or focused upon by OCT. The contrast between lesions
and normal retina in the FAF pattern is obviously enhanced in comparison to a
color photograph pattern. For the patients in Cases 1 and 2, it was easy to
find lesions in the symptomatic eyes, but the fellow eyes also had suspected
lesions, which could not be readily found in a normal color photograph pattern.
The superonasal lesion in the left eye of Case 2 can’t be detected by OCT
because it was too peripheral. In this circumstance, ultra-wide-field FAF
imaging pattern can provide an excellent way to capture lesions in the
peripheral retina at a very early stage.
In patients with a known history of
primary tumor, it is necessary to detect the fundus to exclude choroidal
metastasis. The keys to the prognosis are early detection and early treatment.
In patients with multiple suspect choroidal lesions but no previous history of
tumor, it is important to conduct a systemic examination, especially of the lung
and breast. We can first screen by the FAF pattern of ultra-wide-field imaging
and subsequently verify the presumed lesion by OCT.
In conclusion, ultra-wide-field FAF
is a valuable noninvasive tool for the early diagnosis for metastatic choroidal
tumor, especially for occult and peripheral lesions, and is effective in early
choroidal metastasis screening.
ACKNOWLEDGEMENTS
Authors’ contributions: Ye PP drafted the manuscript. Xu J,
Su ZT and Fang XY collected the data. Yao K revised the manuscript. Each author
of this manuscript has contributed substantially to the research, preparation
and production of the paper and approves of its submission to the journal.
Foundation: Supported by Zhejiang Natural
Science Foundation Project of China (No.LY18H120001).
Conflicts of Interest: Ye PP, None; Xu J, None; Su ZT,
None; Fang XY, None; Yao K, None.
REFERENCES
|
1 Konstantinidis L, Rospond-Kubiak I,
Zeolite I, Heimann H, Groenewald C, Coupland SE, Damato B. Management of patients
with uveal metastases at the liverpool ocular oncology centre. Br J
Ophthalmol 2014;98(1):92-98.
https://doi.org/10.1136/bjophthalmol-2013-303519
PMid:24169654
|
|
|
|
2 Arepalli S, Kaliki S, Shields CL.
Choroidal metastases: origin, features, and therapy. Indian J Ophthalmol
2015;63(2):122-127.
https://doi.org/10.4103/0301-4738.154380
PMid:25827542 PMCid:PMC4399120
|
|
|
|
|
3 Maheshwari A, Finger PT. Cancers of the
eye. Cancer Metastasis Rev 2018;37(4):677-690.
https://doi.org/10.1007/s10555-018-9762-9
PMid:30203109
|
|
|
|
|
4 Mathis T, Jardel P, Loria O, Delaunay B,
Nguyen AM, Lanza F, Mosci C, Caujolle JP, Kodjikian L, Thariat J. New
concepts in the diagnosis and management of choroidal metastases. Prog Retin
Eye Res 2019;68:144-176.
https://doi.org/10.1016/j.preteyeres.2018.09.003
PMid:30240895
|
|
|
|
|
5 Collet LC, Pulido JS, Gündüz K, Diago T,
McCannel C, Blodi C, Link T. Fundus autofluorescence in choroidal metastatic lesions:
a pilot study. Retina 2008;28(9):1251-1256.
https://doi.org/10.1097/IAE.0b013e318188c7d0
PMid:19430391
|
|
|
|
|
6 Almeida A, Kaliki S, Shields CL. Autofluorescence
of intraocular tumours. Curr Opin Ophthalmol 2013;24(3):222-232.
https://doi.org/10.1097/ICU.0b013e32835f8ba1
PMid:23429597
|
|
|
|
|
7 Ishida T, Ohno-Matsui K, Kaneko Y, Tobita
H, Hayashi K, Shimada N, Mochizuki M. Autofluorescence of metastatic
choroidal tumor. Int Ophthalmol 2009;29(4):309-313.
https://doi.org/10.1007/s10792-008-9234-2
PMid:18528641 PMCid:PMC2714453
|
|
|
|
|
8 Natesh S, Chin KJ, Finger PT. Choroidal
metastases fundus autofluorescence imaging: correlation to clinical, OCT, and
fluorescein angiographic findings. Ophthalmic Surg Lasers Imaging 2010;41(4):
406-412.
https://doi.org/10.3928/15428877-20100426-03
PMid:20438045
|
|
|
|
|
9 Kawali A, Pichi F, Avadhani K, Invernizzi
A, Hashimoto Y, Mahendradas P. Multimodal imaging of the normal eye. Ocul
Immunol Inflamm 2017;25(5):721-731.
https://doi.org/10.1080/09273948.2017.1375531
PMid:29083979
|
|
|
|
|
10 Patel M, Kiss S. Ultra-wide-field fluorescein
angiography in retinal disease. Curr Opin Ophthalmol 2014;25(3):213-220.
https://doi.org/10.1097/ICU.0000000000000042
PMid:24614144
|
|