Table 1 Classi fication of degree of preoperative severity of PCG cases[10]
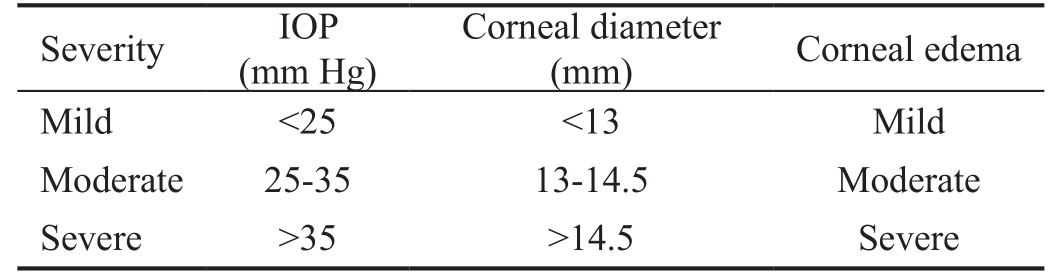
IOP: Intraocular pressure; PCG: Primary congenital glaucoma.
?
Primary congenital glaucoma (PCG) is essentially a surgical disease demanding an apt management by qualified surgeons in well-equipped tertiary centers[1]. Pediatric glaucoma surgery had been altered dramatically in the 1940s owing to the introduction of the angle surgery[2]. Classic fifirst-line options often include angle incisional procedures as goniotomy and trabeculotomy with reported high success rates and minimal hazards[3-4]. Published compelling evidence of high success rate of combined trabeculotomy-trabeculectomy(CTT) had introduced this combined surgery in the paradigm for managing PCG[5]. Yet, there is still a debate concerning the selection of the type of surgery for managing PCG especially in the advanced cases[6].
Unfortunately, these diverse surgical interventions are not always capable of controlling the disease, owing to its hallmark structural defects[7]. Even with the best hands, about 15% to 20% of the fifirst surgeries ultimately fail[8]. When it fails; surgeons become challenged to determine the appropriate next step. Eventually many patients require more than one surgery for long-term control of the intraocular pressure (IOP).Augmented trabeculectomy, glaucoma drainage device (GDD)surgery or cyclodestructive procedures are often proposed as options for re-surgery. So far, there is no solid consensus regarding the surgical archetype after failure of the primary surgery[9].
The current study is a retrospective study of surgical procedures practiced in our community for both the fifirst and the redosurgery in children with PCG with intension to reach a future paradigm for managing these cases.
Ethical Approval The study was registered and approved by the Ethics Committee (Institutional Review Board, IRB),Faculty of Medicine, Mansoura University and adherent to the tents of Declaration of Helsinki. Written informed consent was obtained from the guardians of the patients.
Study Design A retrospective study including patients with PCG attending Mansoura Ophthalmic Center (Department of Ophthalmology at Mansoura University, Egypt) during the period from January 2010 to January 2018. Patients eligible for the study were patients diagnosed with PCG with complete data. Records with follow up less than 6mo after the fifirst surgery and those less than 12mo after the redo-surgery were excluded from the study. Patients with other etiologies of childhood glaucoma were also excluded.
Data Collection Charts of patients diagnosed with PCG during the specified period were retrospectively reviewed.Rosters were used to gather demographic information as age, gender and laterality. The type and the number of both glaucoma surgeries and of anti-glaucomatous drugs (AGD)were obtained for each patient. Clinical data were obtained at presentation, before the second operation and at 6- and 12-month's follow-up point after the fifirst and redo-surgery respectively. Measurement of IOP was obtained at the initial phase of inhalation anesthesia under sevoflurane using TonoPen. Cup disc ratio values were obtained by direct or indirect ophthalmoscope whenever the media permits. Corneal diameter was measured horizontally (white-to-white) by calipers. Corneal edema was evaluated under biomicroscopy and was categorized into mild (detected by direct focal ophthalmoscope), moderate (partially obscuring the iris details)and severe (completely obscuring the iris details). The degree of the preoperative severity was assessed according to the IOP,corneal diameter and corneal edema. Scores from 1 to 3 were given for each parameter; then according to the total score; the eyes were classified as mild for scores from 1-3, moderate for scores 4-6 and severe for scores 7-9 (Table 1)[10].
In preverbal children, various age-matching visual testing measures were used as, the ability to fix and follow light or preferential looking. Results were given as age-matched normal visual acuity (VA) or subnormal VA. Snellen's chart was used in older verbal patients converted to logMAR for statistical analysis. Counting fingers vision, hand movementsand light perception were given the values of 2.0, 3.0 and 4.0 on logMAR charts respectively. Snellen's VA results were categorized as follows: good when VA was ≤0.4, fair for VA between 1 and 0.5 and poor if >1. Refraction was measured by automated retinoscopy (Righton-Retinomax K-plus 2, Tokoyo,Japan) or manual retinoscopy according to the clarity of the media. Recorded surgical complications were analyzed and the number of subsequent surgeries was recorded.
Table 1 Classi fication of degree of preoperative severity of PCG cases[10]
IOP: Intraocular pressure; PCG: Primary congenital glaucoma.
?
Success Criteria The target IOP was defined as IOP>5 mm Hg and ≤21 mm Hg with stability of ocular biometric measurement(corneal diameter, cup disc ratio and corneal clarity). Success was labeled complete if the target IOP was achieved without AGD; and labeled qualified if the target IOP was achieved with AGD. Total success was the sum of complete and qualified success. Failure was defined as IOP<5 mm Hg or >21 mm Hg despite the use of maximum tolerated AGD on two consecutive scheduled visits or the need of further glaucoma surgical intervention apart from tubal repositioning or covering the valve tube with patch. Visual devastating complications or loss of vision were considered as failure of the procedure.
Statistical AnalysisData were analyzed with SPSS version 22 (SPSS, Chicago, IL, USA). The normality of data was first tested using one-sample Kolmogorov-Smirnov test. Qualitative data was described using number and percent. Continuous variables were presented as mean±standard deviation (SD)for parametric data and median (min-max) for non-parametric data. For comparing parametric data within the same group;paired t-test was used to compare between two measurements while repeated measure ANOVA test was used to compare between more than two measurements. One-way ANOVA test was used to compare between more than two groups and independent t-test was used to compare between two groups.Kaplan-Meier survival curves were used to evaluate the survival rate and the failure probabilities. Cox proportionalhazards regression of the baseline factors and their correlations to the failure hazard rate was carried out. In all statistical tests,P value ≤0.05 was considered to be statistically significant.
Demographic and clinical data Complete clinical records were obtained for 272 eyes (153 patients) with PCG with mean age of 19.4±9.7mo; range (2-46mo) with 92 (60%)males. Six patients (3.9% eyes) were older than 3 years old represented late-presentation for PCG. Most of the patients had bilateral presentation (77.8%). Forty-three eyes had mild presentation, 136 moderate and 93 severe. Preoperative cupdisc ratio was available only for 28 eyes with mean 0.5±0.2 and range 0.3-0.7. Baseline VA and refraction values were available in only few cases and were not included. As regard the primary surgical interference; CTT was the most common primary operation carried out in 150 (55%) eyes followed by trabeculotomy in 71 (26%) eyes. Augmented trabeculectomy was performed in 37 (14%) eyes; using either mitomycin C(MMC) in 21 (8%) eyes and Ologen implant in 16 (6%) eyes.Primary Ahmed Glaucoma Valve (AGV) was practiced in a limited number of the eyes (14 eyes, 5%). Table 2 gives details about the baseline clinical data among the four groups of the primary surgeries. There was statistically significant difference between the groups regarding the severity (P<0.001) and the baseline IOP being highest in the primary AGV group(P<0.001).
Table 2 Baseline clinical data of the patients at presentation with success rates at 6th month among the four types of primary surgery n (%)

SD: Standard deviation; min-max: Minimum-maximum; IOP: Intraocular pressure; CTT: Combined trabeculotomy and trabeculectomy; SST:Subscleral trabeculectomy; AGV: Ahmed glaucoma valve. One-way ANOVA test followed by post hoc Bonferroni for pair wise comparison.Chi-square test was used to compare the degree of the severity between the groups.aP≤0.05 vs primary AGV;bP≤0.05 vs augmented SST.
?
Success rate The success rates calculated at 6mo among the different types of primary surgeries are given in details in Table 2. There was statistically significant difference between the four types of primary surgery regarding the success rates in different degrees of severity (P<0.001). The CTT had the highest total success rate in moderate (96.4%) and severe cases(59.3%) while trabeculotomy was the highest in mild cases(96.3%).
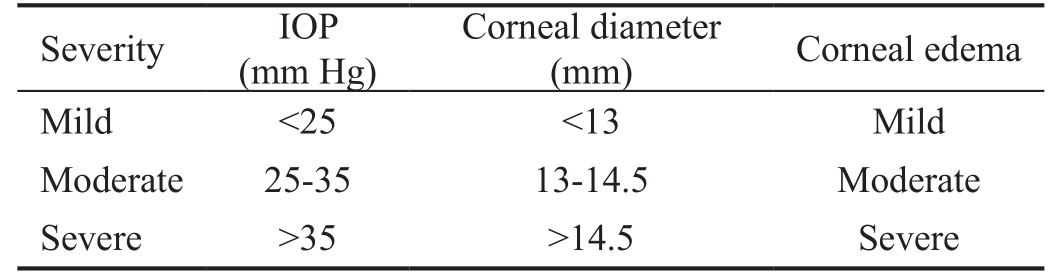
Kaplan Meier curve in Figure 1 demonstrates the log survival curve for the four primary surgeries. The mean survival time was 6.255, 5.517, 4.919 and 3.450mo for CTT, trabeculotomy,augmented trabeculectomy and AGV respectively. The difference was statistically highly significant according to the Log-Rank test (P<0.001).
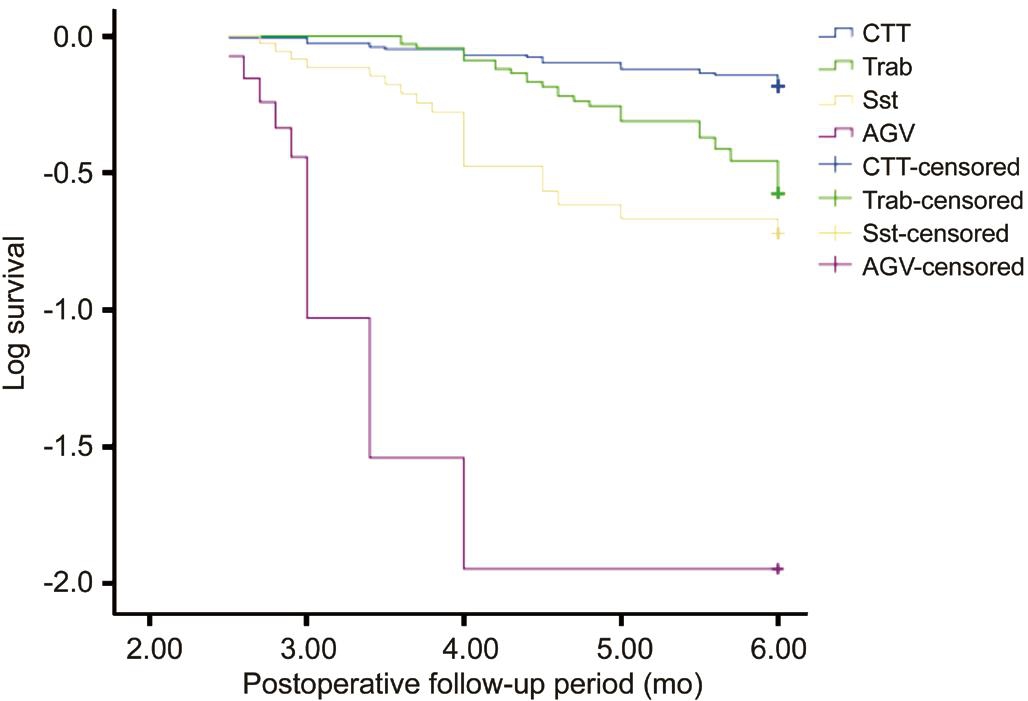
Figure 1 Kaplan-Meier log survival curve for the four types of primary surgery along the follow-up period showing rapid decrease in the curve for primary AGV while more stability in the curves for both CTT and trabeculotomy (trab).
Demographic and clinical data The records of the 63 recurrent cases of PCG (88 eyes) were retrieved for further analysis. The mean interval between the fifirst and the second surgery was 9.76±2.4 (range 6-14)mo. The mean age of the patients was 26.43±10.21mo before the second surgical interference. Forty-one patients were males and 22 were females, with ratio 1.9:1. Thirty-eight patients (60.3%) had unilateral recurrence mostly with severe presentation (59 eyes).Prior to the secondary surgery the mean IOP was 31.8±2.82(range 27-40) mm Hg with mean 2.3±0.463 AGD.
Ahmed valve implantation model fp8 (New World Medical, Inc., Rancho Cucamonga, CA, USA) was used in67 (76%) recurrent eyes; while 21 (24%) eyes had augmented trabeculectomy with Ologen implant soaked in MMC.Table 3 gives details about the baseline demographic and clinical characteristics of the patients before the two types of secondary surgeries. Preoperative VA was deficient in 74 (84%) of the recurrent eyes. The preoperative IOP was statistically higher in the AGV group (P<0.001). The followup period was statistically longer in the valve group of patients(P=0.048).
Table 3 Pre- and postoperative clinical data of recurrent cases of PCG at 1-year follow-up within the two types of second surgeries n (%)
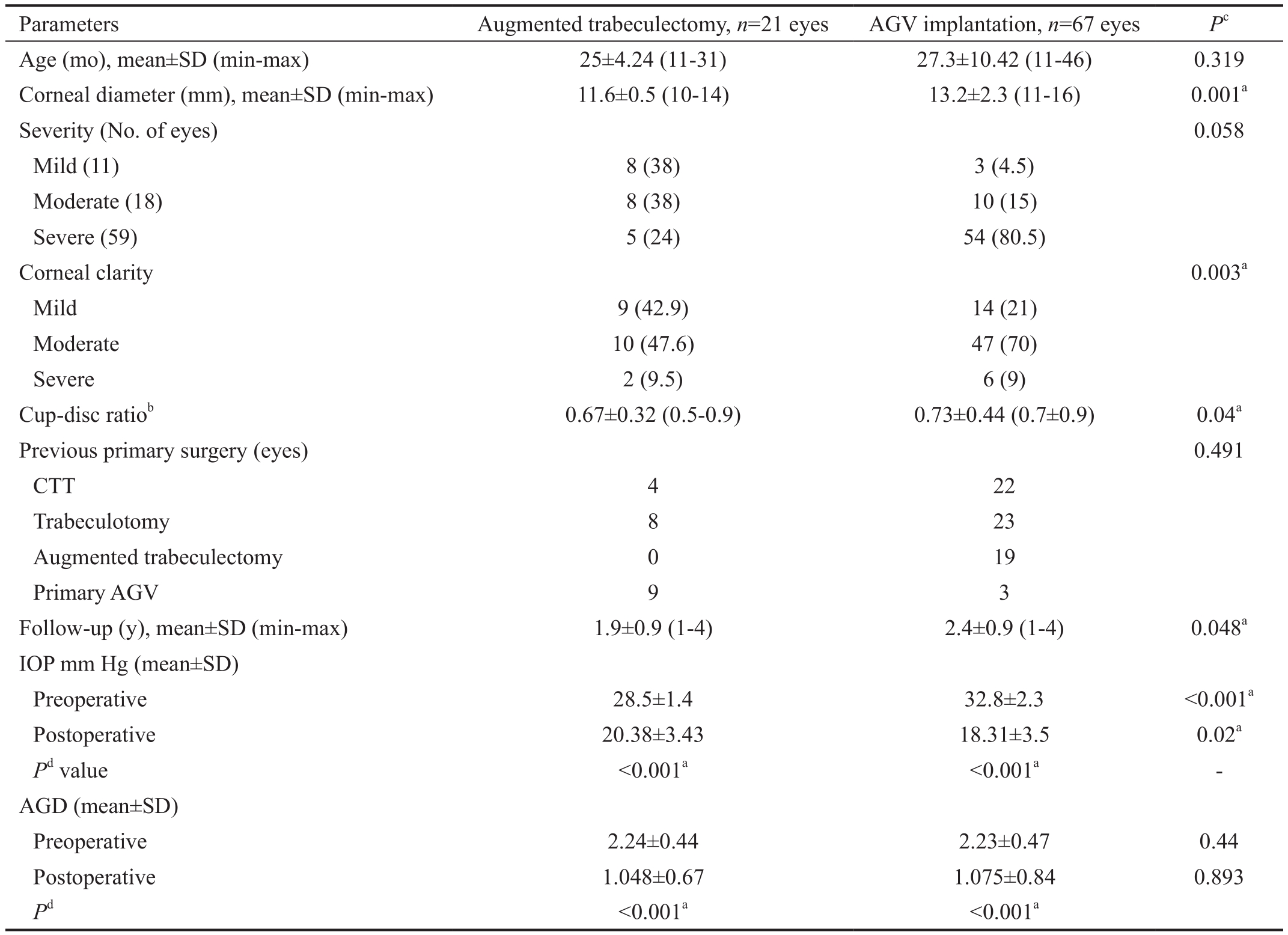
CTT: Combined trabeculotomy and trabeculectomy; SD: Standard deviation; min-max: minimum-maximum; IOP: Intraocular pressure; AGD:Antiglaucomatous drugs; AGV: Ahmed glaucoma valve.asignificance value at P≤0.05.bMeasured in 32 eyes only.cIndependent t-test between the 2 groups;dPaired t-test within each group.
 Age (mo), mean±SD (min-max) 25±4.24 (11-31) 27.3±10.42 (11-46) 0.319 Corneal diameter (mm), mean±SD (min-max) 11.6±0.5 (10-14) 13.2±2.3 (11-16) 0.001a Severity (No. of eyes) 0.058 Mild (11) 8 (38) 3 (4.5)Moderate (18) 8 (38) 10 (15)Severe (59) 5 (24) 54 (80.5)Corneal clarity 0.003a Mild 9 (42.9) 14 (21)Moderate 10 (47.6) 47 (70)Severe 2 (9.5) 6 (9)Cup-disc ratiob 0.67±0.32 (0.5-0.9) 0.73±0.44 (0.7±0.9) 0.04a Previous primary surgery (eyes) 0.491 CTT 4 22 Trabeculotomy 8 23 Augmented trabeculectomy 0 19 Primary AGV 9 3 Follow-up (y), mean±SD (min-max) 1.9±0.9 (1-4) 2.4±0.9 (1-4) 0.048a IOP mm Hg (mean±SD)Preoperative 28.5±1.4 32.8±2.3 <0.001a Postoperative 20.38±3.43 18.31±3.5 0.02a Pd value <0.001a <0.001a -AGD (mean±SD)Preoperative 2.24±0.44 2.23±0.47 0.44 Postoperative 1.048±0.67 1.075±0.84 0.893 Pd <0.001a <0.001a
Age (mo), mean±SD (min-max) 25±4.24 (11-31) 27.3±10.42 (11-46) 0.319 Corneal diameter (mm), mean±SD (min-max) 11.6±0.5 (10-14) 13.2±2.3 (11-16) 0.001a Severity (No. of eyes) 0.058 Mild (11) 8 (38) 3 (4.5)Moderate (18) 8 (38) 10 (15)Severe (59) 5 (24) 54 (80.5)Corneal clarity 0.003a Mild 9 (42.9) 14 (21)Moderate 10 (47.6) 47 (70)Severe 2 (9.5) 6 (9)Cup-disc ratiob 0.67±0.32 (0.5-0.9) 0.73±0.44 (0.7±0.9) 0.04a Previous primary surgery (eyes) 0.491 CTT 4 22 Trabeculotomy 8 23 Augmented trabeculectomy 0 19 Primary AGV 9 3 Follow-up (y), mean±SD (min-max) 1.9±0.9 (1-4) 2.4±0.9 (1-4) 0.048a IOP mm Hg (mean±SD)Preoperative 28.5±1.4 32.8±2.3 <0.001a Postoperative 20.38±3.43 18.31±3.5 0.02a Pd value <0.001a <0.001a -AGD (mean±SD)Preoperative 2.24±0.44 2.23±0.47 0.44 Postoperative 1.048±0.67 1.075±0.84 0.893 Pd <0.001a <0.001a
Intraocular pressure and antiglaucomatous drugs There was statistically significant drop in the postoperative IOP as well as the number of AGD at 12mo compared with the preoperative values for the 2 groups (P<0.001). At the 12th month,the IOP in the AGV cases was statistically lower than that with the augmented trabeculectomy cases (P=0.02). The difference was not significant regarding the number of the postoperative AGD between the 2 groups (P=0.893; Table 3). Topical beta-blockers, carbonic anhydrase inhibitors (CAIS) and prostaglandin analogs were the most frequent drops prescribed.
Visual acuity Postoperative Snellen's VA was recorded in only 32 eyes. In augmented trabeculectomy group, good and fair vision were reported in 2 (9.5%) each and 1 (4.8%) eye with poor VA. In AGV group, good vision was reported in 5 (7.5%) eyes, fair vision in 6 (8.9%) eyes, poor vision in 14 (20.8%) eyes and no light perception in 2 (2.3%) eyes. In other preverbal cases, 11 (52.4%) and 26 (39%) eyes had agematched normal VA in augmented trabeculectomy and AGV groups respectively while 5 (23.8%) eyes after trabeculectomy and 14 (20.8%) in AGV group had subnormal VA.
Refractive errors Postoperative refractive results were available for 69 (78.4%) eyes; 46 (66.7%) were myopic with mean spherical equivalent (SE) of -6.74±0.5 D (range -11.0 to-1.25 D) and 23 (33.3%) eyes were hyperopic with mean of 2.4±0.7 D (range 0.5 to 4.0 D).
Success and failure rates Success rates calculated at oneyear follow-up were statistically insignificant between the two groups (P=0.256). Complete success was recorded in 4 (19%)eyes in trabeculectomy group and 21 (31.3%) of the eyes in AGV group; and qualified success was recorded in 11 (52.4%)and 37 (55.2%) eyes in trabeculectomy and AGV groups respectively (Figure 2). Correlating the success rates to the preoperative severity of the recurrent cases demonstrated that mild cases responds well to both types of surgery (100%success rate for both surgeries), while severe cases showed higher success rates following AGV (87%) than augmented trabeculectomy (20%) (Table 4).
Ocular measurements There was no progression in the corneal diameter following either of the two surgeries.Corneal edema was cleared in 6 (28.6%) eyes following augmented trabeculectomy and in 41 (61.2%) eyes following AGV. Two (3%) eyes developed total corneal scar followed AGV complicated with endophthalmitis and 4 (6%) eyes developed localized corneal opacity over the site of the tube touch. Reversible cupping was documented in 2 (9.5%) eyes following trabeculectomy and in 3 (4.5%) eyes following AGV.
Kaplan-Meier survival analysis Figure 3 showed Kaplan-Meier survival curve analysis of the success rate of both secondary operations throughout the follow-up period. The mean survival time throughout one year was prolonged in AGV group (11.15±0.268mo) than the augmented trabeculectomy(10.4±0.68mo) however the difference was statistically insignificant according to the Log-Rank test (P=0.08). The cumulative probability of total success for the augmented trabeculectomy group was 100%, 67.5% and 65.5% at 3, 6-and 12-months follow-up, respectively. While the cumulative probability of total success for the AGV group was 99%, 87%and 83% at corresponding points of follow-up.
Predictors for success Table 5 presents Cox proportional hazards regression analysis of the secondary surgical outcome according to the preoperative variables. Patients who were younger than 24mo had higher probabilities of failure following both second surgeries. For AGV, the hazard ratio(HR) was 0.37 which increases by 0.6% for each month decrease in age. In augmented trabeculectomy, HR for age was 1.325 with an increase the hazard by 32% for a one month decrease in age. Preoperative severity was another significant risk factor for failure for surgery in augmented trabeculectomy only with a 0.89% higher HR of for severe stage. The HR for other predicting factors remained constant over time.
Complications of the secondary surgeries In the augmented trabeculectomy group, the most common postoperative recorded complication was shallow anterior chamber (AC).Flat AC that required reformation with viscoelastic materials injection was reported in 3 (14.3%) eyes. Severe hyphema requiring surgical evacuation was reported in 2 (9.5%) eyes.
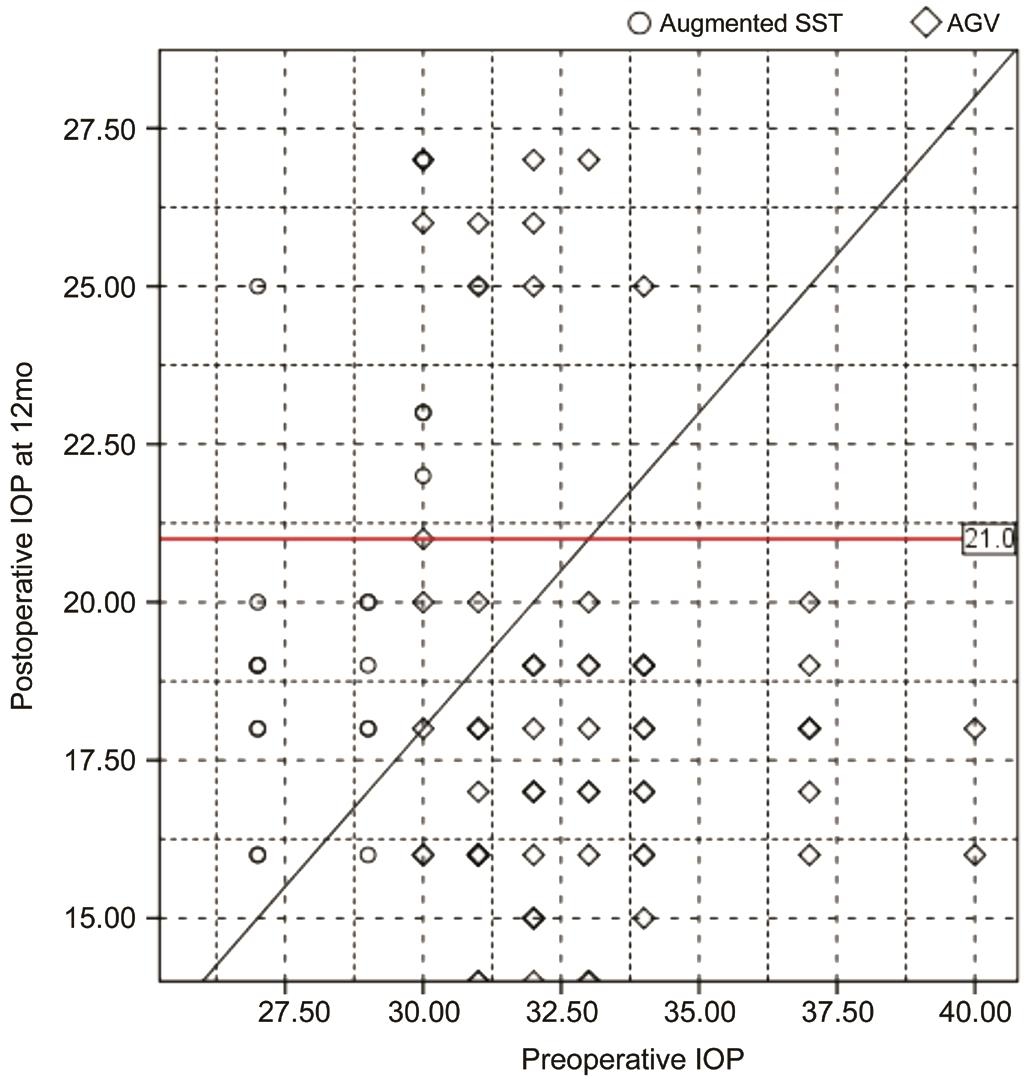
Figure 2 Scatter gram for the pre- and postoperative IOP at 12-month follow-up in both types of secondary surgery
The horizontal redline represents the cut-off values for success (IOP≤21 mm Hg). Dots below the horizontal line represent the eyes reaching the target IOP value.
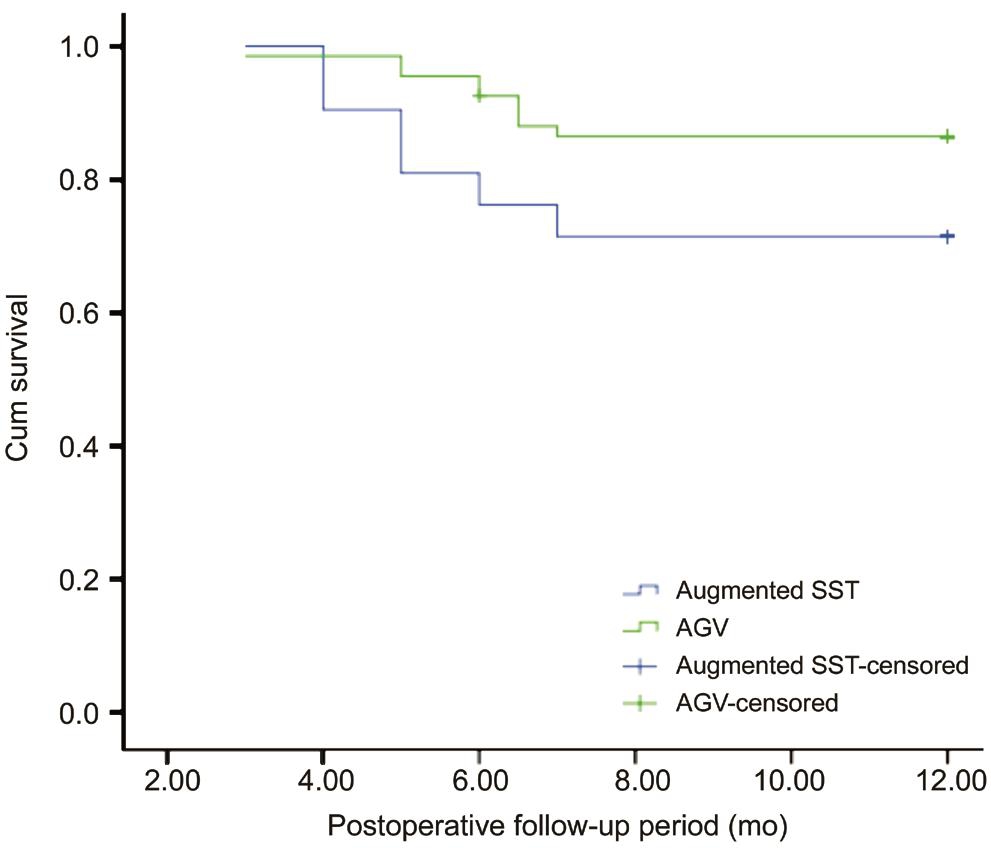
Figure 3 Kaplan-Meier survival curve for eyes with recurrent PCG treated with either augmented trabeculectomy or AGV implantation as second surgery
The success rates for both surgeries declined over time. The rates for AGV declined slower than trabeculectomy.
Table 4 Categorization of the postoperative success rates according to the degree of preoperative severity of the recurrent cases n (%)
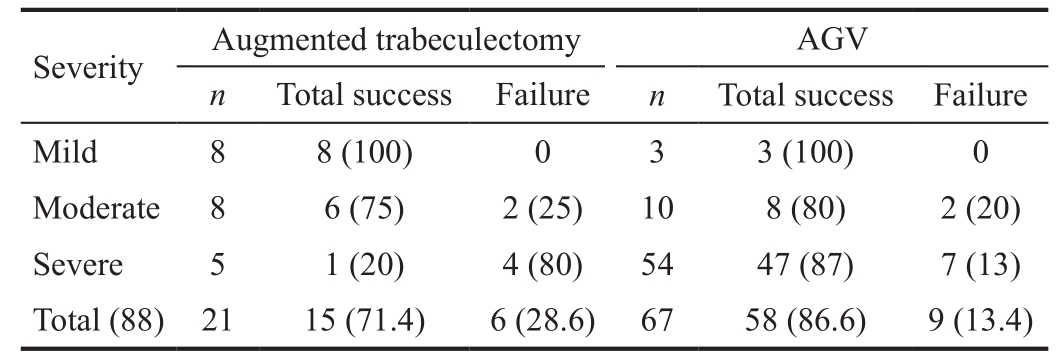
AGV: Ahmed glaucoma valve.
?
Table 5 Cox proportional-hazards regression of the potential factors affecting the surgical outcome at 12mo n (%)
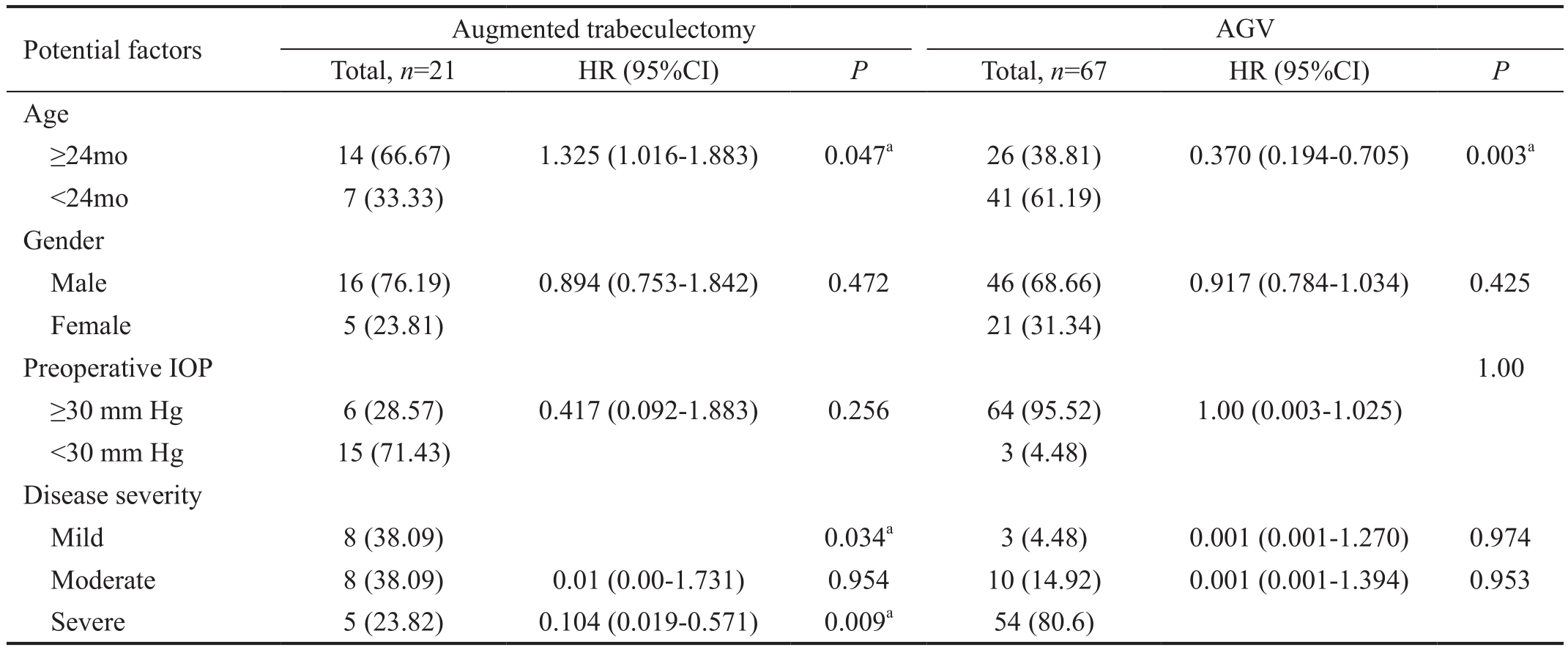
AGV: Ahmed glaucoma valve; CI: confidence interval; HR: Hazard ratio; IOP: Intraocular pressure.aP≤0.05.
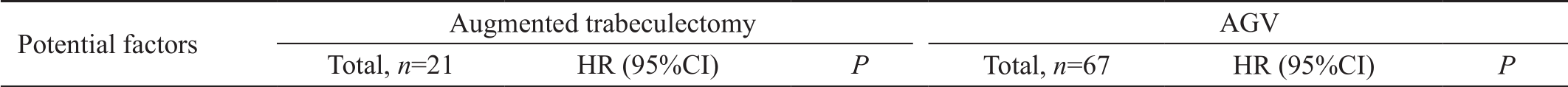 Age≥24mo 14 (66.67) 1.325 (1.016-1.883) 0.047a 26 (38.81) 0.370 (0.194-0.705) 0.003a<24mo 7 (33.33) 41 (61.19)Gender Male 16 (76.19) 0.894 (0.753-1.842) 0.472 46 (68.66) 0.917 (0.784-1.034) 0.425 Female 5 (23.81) 21 (31.34)Preoperative IOP 1.00≥30 mm Hg 6 (28.57) 0.417 (0.092-1.883) 0.256 64 (95.52) 1.00 (0.003-1.025)<30 mm Hg 15 (71.43) 3 (4.48)Disease severity Mild 8 (38.09) 0.034a 3 (4.48) 0.001 (0.001-1.270) 0.974 Moderate 8 (38.09) 0.01 (0.00-1.731) 0.954 10 (14.92) 0.001 (0.001-1.394) 0.953 Severe 5 (23.82) 0.104 (0.019-0.571) 0.009a 54 (80.6)
Age≥24mo 14 (66.67) 1.325 (1.016-1.883) 0.047a 26 (38.81) 0.370 (0.194-0.705) 0.003a<24mo 7 (33.33) 41 (61.19)Gender Male 16 (76.19) 0.894 (0.753-1.842) 0.472 46 (68.66) 0.917 (0.784-1.034) 0.425 Female 5 (23.81) 21 (31.34)Preoperative IOP 1.00≥30 mm Hg 6 (28.57) 0.417 (0.092-1.883) 0.256 64 (95.52) 1.00 (0.003-1.025)<30 mm Hg 15 (71.43) 3 (4.48)Disease severity Mild 8 (38.09) 0.034a 3 (4.48) 0.001 (0.001-1.270) 0.974 Moderate 8 (38.09) 0.01 (0.00-1.731) 0.954 10 (14.92) 0.001 (0.001-1.394) 0.953 Severe 5 (23.82) 0.104 (0.019-0.571) 0.009a 54 (80.6)
In the AGV group, choroidal effusion was the most common complication occurred in 12 (18%) eyes which resolved with medical treatment (systemic and topical steroids and atropine eye drops). Conjunctival erosions over the valve tube was recorded in 6 (9%) eyes; that were treated by suturing and repositioning of the conjunctiva over the valve in 4 eyes and using scleral patch graft in the other 2 eyes. Tube-corneal touch requiring surgical repositioning was reported in 4 (6%) eyes.Severe hyphema was reported in 2 (3%) eyes. Explanation of the valve was carried in 2 (3%) eyes due to developing of endophthalmitis with subsequent development of phthisis bulbi. Recurrent cases were treated with cyclodestructive measures as cyclocryoablation in 1 (16.7%) and 2 (22.2%)eyes after trabeculectomy and AGV groups respectively.Micropulsed diode laser cyclophotocoagulation was reported in 1 (16.7%) and 4 (44.4%) eyes after the failed trabeculectomy and AGV respectively. Exchange of AGV was performed in 1 (11%) eye and secondary valve was implanted in 4 (66.6%)eyes following trabeculectomy in recurrent cases.
Primary and subsequent surgical choices need to be tailored for each patient according to the patient's condition with perspective to the surgeon's experience in addition to accessibility of the appropriate instruments[11-12].
We conducted a retrospective study involving the medical records of the patients with PCG over the past 8y presented in Mansoura Ophthalmic Center a tertiary hospital in our locality.Severity stratification of the included patients was carried out retrospectively depending on the corneal diameter, IOP and corneal edema. Both primary and redo-surgeries were evaluated regarding the success rate in relation to the severity of the cases at 6th and 12th month respectively.
In the current study, none of the patients underwent goniotomy,as the majority of the patients presented late in the course of the disease losing their opportunity to experience the classic fifirst-line procedure. Trabeculotomy, CTT and augmented trabeculectomy were used as primary surgical options for PCG for most of the cases in our study, while primary valve was practiced only in a small percentage of cases (5%).
CTT has gained superb interest as a surgical option for PCG with published satisfactory outcomes advocating it to be considered as the first choice especially in advanced cases[13-14].In our study, the total success rate at 6th month was 82.6%which is consistent with the results reported by Mandal et al[15] where the cumulative success rate of CTT was 80.5%at corresponding follow up point. The compelling results of the CTT may be related to the dual outflow pathway as enlightened by Mandal et al[14]. CTT offers more fl exibility in advanced cases in which the identi fication of Schlemm's canal may become unfeasible during the operation. CTT permits the chances for conversion to trabeculectomy in the same setting[14-15].
At the 6th month, the success rate for trabeculotomy in our study was 56.3% which is much lower than the results reported in a German study[16] reporting 92.6% success rate after one year of follow-up. This may be contributed to the degree of severity of our presented cases. Near half of the cases (46.5%)in the trabeculotomy group were in the moderate category with only 36.4% success rate. In Al-Hazmi et al's study[10],comparable success rates were reported (40% in moderate and 10% for severe cases). They concluded that trabeculotomy might be considered an appropriate choice only for mild cases of PCG in their population. Consistently, in the current study,trabeculotomy achieved total success in 96.3% of the mild eyes.Primary trabeculectomy is still an effective and popular option in some countries. Augmented primary trabeculectomy was applied in 37 (14%) eyes with 48.6% success rate in our series. Comparable results were published in a retrospective study conducted in Nigeria demonstrating significant reduction of IOP[17]. At one year follow-up, Rodrigues et al[18]reported a success rate ranging from 35% to 50% for primary trabeculectomy. Lower success rates were reported in children presenting before one year of age in a long-term study for primary trabeculectomy in PCG conducted by Fulcher et al[19].Success rate following primary AGV in our study (14.3%)were much lower than those published in the literature (63%to 93%) after 1y[20-21]. This may be contributed to the type of glaucoma, as they included heterogeneous types of pediatric glaucoma not only the PCG. Similar low success rates were reported by Ou et al[22] and Djodeyre et al[23] in eyes with congenital glaucoma.
Based on the previous findings, we adopt the following practice guidelines on selecting the primary surgery in our department. Trabeculotomy is the fifirst choice for mild PCG cases. In cases with moderate severity, CTT is to be performed.Augmented trabeculectomy will be used in cases with more severe presentation. Primary AGV was proven suboptimal in primary cases and is no more advised.
So far, there is no solid agreement regarding the ideal surgical algorithm after failure of angle surgery as there is wide distinction in the recommended treatment adopted by various experienced institutions. Unfortunately, studies prospectively comparing the options for secondary surgery are deficient,some recommendations are available based on the limited,retrospective literature[9].
Beck et al[24] compared the results of trabeculectomy augmented with MMC and GDD in pediatric glaucoma before age of two. The cumulative success rate of GDD was higher than that of the trabeculectomy group at 12mo (87% versus 36%respectively). These results are consistent to our results;where the cumulative success rate in AGV was higher at 12mo compared with augmented trabeculectomy (83% versus 65.5%). However, the difference was statistically insignificant(P=0.08). The probability of success declined along the follow up period in both groups with slower rate in Ahmed valve group compared with the trabeculectomy group.
On the contrary, the Armenian Eye Care Project study[25]reported comparable success rates at 18mo follow-up (88%versus 86% for the Ahmed valve and MMC augmented trabeculectomy).
Trabeculectomy in children is frequently confronted with multiple inherited reasons for failure as the existence of thin sclera, thick Tenon's capsule, complexity in recognizing the limbus as well as the exuberant healing response. Thus, the use of antimetabolites as MMC or implants as Ologen had gained much popularity[26]. In our study we implemented the use of Ologen soaked in MMC in some cases with intension to gain a double effect from both. Dada et al[27] suggested that this maneuver offers encouraging short-term control for IOP in primary open angle glaucoma. Min et al[28] found that Ologen soaked in MMC exerted synergistic effect in precluding the exaggerated wound healing especially in cases where encapsulated blebs are more anticipated.
Several published studies favored the selection of GDD in buphthalmic eyes with very thin sclera or in cases where conjunctival scarring is pronounced; assuming that the long-term risk of infection is lower as the bleb is located posteriorly in GDD[29-30]. However, GDDs are not hazardless as they usually require more successive operations than trabeculectomy (46% vs 13%), especially tube repositioning or coverage[22,24]. In the current study, AGV resulted in more serious complications than trabeculectomy. Short followup period in our series; may played some role in masking the well-known long-term hazards of antimetabolites. In our study, though the difference in the success rate between the two second surgeries was statistically insignificant (P=0.256);AGV proved to be superior on trabeculectomy in severe cases where the success rate was 87% and 20% in these cases for the two operations respectively.
Analyzing the preoperative risk factors in the current study;revealed that age was an independent risk factor for failure for both second surgeries. Similar results were published in previous studies suggesting that lower success rates are predicted after trabeculectomy in younger children[24]. Chen et al[26] found older age to be associated with higher rates of survival following secondary AGV. On the other hand, our results showed that the severity of the condition significantly affected the success rates in trabeculectomy but not in AGV.
Cyclodestructive procedures performed in refractory pediatric glaucoma comprise the classic cyclocryotherapy as well as the recently introduced transscleral and endoscopic cyclophotocoagulation. Most of the clinicians had preserved those procedures as a last ditch for treatment after failure of angle procedure and another consecutive modality of surgery owing to their common irreversible complications as retinal detachment, hypotony, loss of vision and phthisis bulbi.Moreover, it is hard to titrate the exact number of sessions required to attain IOP control[9]. In our series, cyclodestructive procedures were used after failure of the second surgeries in eyes with very poor VA. Micropulsed transcleral cyclophotocoagulation, a new modality of cyclodiode laser has been recently introduced with promising short-term results[31].In our study, five cases were treated with this new modality;however, their complete follow-up data is not yet attained.
Scrutinizing the results of the second operations drove us to recommend the use of augmented trabeculectomy in older,recurrent, milder cases with favorable conjunctival condition;while implanting AGV in more severe recurrent cases.
Recurrent cases after primary valve may gain benefit from exchanging the valve or adding another valve. Cyclodestructive procedures are reserved as the third line of treatment for more advanced cases.
To the best of our knowledge, this is the fifirst study in our community evaluating the results for both the fifirst and the redo-surgery in PCG. However, the study was restricted by its retrospective nature, some unavailable data for some cases as refraction and CD ratio, small number of patients in the redosurgery owed to the limit number of the available complete medical records and lack of the follow-up data for the third surgery.
In conclusion, meticulous preoperative assessment of the severity of patients with PCG helps in the selecting the optimal primary and secondary surgery. For primary surgery,trabeculotomy is more effective in mild cases whereas; CTT and augmented SST are appropriate for moderate and severe cases. AGV proved to be superior to augmented SST in severe recurrent cases. Cyclodestructive procedures are better reserved after failure of more than one glaucoma surgery.
Authors' contributions:Mokbel TH and El Hefney EM designed and conceived the study; El Hefney EM, Hagras SM, Badawi AE, El Khouly SE and Gaafar WM performed the surgeries included in the study. Al Nagdy AA, Hagras SM,and Badawi AE collected the data from the records; Hagras SM wrote the manuscript, analyzed the data and shared in the statistics and in final revision; Badawi AE analyzed the data,worked out the statistical part and shared in the manuscript writing and final revision; Kasem MA, El Khouly SE and Gaafar WM shared in analysis and reviewing the manuscript.Mokbel TH; Overall supervision of the study.
Conflicts of Interest: Mokbel TH, None; El Hefney EM,None; Hagras SM, None; Badawi AE, None; Kasem MA,None; Al Nagdy AA, None; El Khouly SE, None; Gaafar WM, None.
1 Kong LK, Fry M, Al-Samarraie M, Gilbert C, Steinkuller PG. An update on progress and the changing epidemiology of causes of childhood blindness worldwide. J AAPOS 2012;16(6):501-507.
2 Moore DB, Tomkins O, Ben-Zion I. A review of primary congenital glaucoma in the developing world. Surv Ophthalmol 2013;58(3):278-285.
3 Yalvac IS, Satana B, Suveren A, Eksioglu U, Duman S. Success of trabeculotomy in patients with congenital glaucoma operated on within 3 months of birth. Eye (Lond) 2007;21(4):459-464.
4 Mendicino ME, Lynch MG, Drack A, Beck AD, Harbin T, Pollard Z,Vela MA, Lynn MJ. Long-term surgical and visual outcomes in primary congenital glaucoma: 360 degrees trabeculotomy versus goniotomy. J AAPOS 2000;4(4):205-210.
5 Khan AO. Trabeculotomy versus trabeculotomy-trabeculectomy for congenital glaucoma. Br J Ophthalmol 2006;90(1):125.
6 Alsheikheh A, Klink J, Klink T, Steffen H, Grehn F. Long-term results of surgery in childhood glaucoma. Graefes Arch Clin Exp Ophthalmol 2007;245(2):195-203.
7 Walton DS, Nagao K, Yeung HH, Kane SA. Late-recognized primary congenital glaucoma. J Pediatr Ophthalmol Strabismus 2013;50(4):234-238.
8 Lee N, Ma KT, Bae HW, Hong SM, Seong GJ, Hong YJ, Kim CY.Surgical results of trabeculectomy and Ahmed valve implantation following a previous failed trabeculectomy in primary congenital glaucoma patients. Korean J Ophthalmol 2015;29(2):109-114.
9 Aldohayab S, Morales J, Edward DP, Abu-amero KK. Update on pediatric glaucoma. Semin Ophthalmol 2013;28(3):131-143.
10 Al-Hazmi A, Awad A, Zwaan J, Al-Mesfer SA, Al-Jadaan I, Al-Mohammed A. Correlation between surgical success rate and severity of congenital glaucoma. Br J Ophthalmol 2005;89(4):449-453.
11 Pakravan M, Homayoon N, Shahin Y, Ali Reza BR. Trabeculectomy with mitomycin C versus Ahmed glaucoma implant with mitomycin C for treatment of pediatric aphakic glaucoma. J Glaucoma 2007;16(7):631-636.
12 Terraciano AJ, Sidoti PA. Management of refractory glaucoma in childhood. Curr Opin Ophthalmol 2002;13(2):97-102.
13 Khan AO. Trabeculotomy versus trabeculotomy-trabeculectomy for congenital glaucoma. Br J Ophthalmol 2006;90(1):125.
14 Mandal AK, Bhatia PG, Gothwal VK, Reddy VM, Sriramulu P,Prasad MS, John RK, Nutheti R, Shamanna BR. Safety and efficacy of simultaneous bilateral primary combined trabeculotomy-trabeculectomy for developmental glaucoma. Indian J Ophthalmol 2002;50(1):13-19.
15 Mandal AK, Matalia JH, Nutheti R, Krishnaiah S. Combined trabeculotomy and trabeculectomy in advanced primary developmental glaucoma with corneal diameter of 14 mm or more. Eye (Lond) 2006;20(2):135-143.
16 Meyer G, Schwenn O, Pfeiffer N, Grehn F. Trabeculotomy in congenital glaucoma. Graefes Arch Clin Exp Ophthalmol 2000;238(3):207-213.
17 Onwasigwe EN, Ezegwui IR, Onwasigwe CN, Aghaji AE.Management of primary congenital glaucoma by trabeculectomy in Nigeria. Ann Trop Paediatr 2008;28(1):49-52.
18 Rodrigues AM, Júnior AP, Montezano FT, de Arruda Melo PA, Prata J Jr. Comparison between results of trabeculectomy in primary congenital glaucoma with and without the use of mitomycin C. J Glaucoma 2004;13(3):228-232.
19 Fulcher T, Chan J, Lanigan B, Bowell R, O'Keefe M. Long-term follow up of primary trabeculectomy for infantile glaucoma. Br J Ophthalmol 1996;80(6):499-502.
20 Morad Y, Donaldson CE, Kim YM, Abdolell M, Levin AV. The Ahmed drainage implant in the treatment of pediatric glaucoma. Am J Ophthalmol 2003;135(6):821-829.
21 O'Malley Schotthoefer E, Yanovitch TL, Freedman SF. Aqueous drainage device surgery in refractory pediatric glaucomas: I. Long-term outcomes. J AAPOS 2008;12(1):33-39.
22 Ou Y, Yu F, Law SK, Coleman AL, Caprioli J. Outcomes of Ahmed glaucoma valve implantation in children with primary congenital glaucoma. Arch Ophthalmol 2009;127(11):1436-1441.
23 Djodeyre MR, Peralta Calvo J, Abelairas Gomez J. Clinical evaluation and risk factors of time to failure of Ahmed Glaucoma Valve implant in pediatric patients. Ophthalmology 2001;108(3):614-620.
24 Beck AD, Freedman S, Kammer J, Jin J. Aqueous shunt devices compared with trabeculectomy with Mitomycin-C for children in the first two years of life. Am J Ophthalmol 2003;136(6):994-1000.
25 Hill R, Ohanesian R, Voskanyan L, Malayan A. The Armenian Eye Care Project: surgical outcomes of complicated paediatric glaucoma. Br J Ophthalmol 2003;87(6):673-676.
26 Chen A, Yu F, Law SK, Giaconi JA, Coleman AL, Caprioli J. Valved glaucoma drainage devices in pediatric glaucoma: retrospective long-term outcomes. JAMA Ophthalmol 2015;133(9):1030-1035.
27 Dada T, Kusumesh R, Bali SJ, Sharma S, Sobti A, Arora V, Panda A.Trabeculectomy with combined use of subconjunctival collagen implant and low-dose mitomycin C. J Glaucoma 2013;22(8):659-662.
28 Min JK, Kee CW, Sohn SW, Lee HJ, Woo JM, Yim JH. Surgical outcome of mitomycin C-soaked collagen matrix implant in trabeculectomy.J Glaucoma 2013;22(6):456-462.
29 Dave P, Senthil S, Choudhari N, Sekhar GC. Outcomes of Ahmed valve implant following a failed initial trabeculotomy and trabeculectomy in refractory primary congenital glaucoma. Middle East Afr J Ophthalmol 2015;22(1):64-68.
30 Ishida K, Mandal AK, Netland PA. Glaucoma drainage implants in pediatric patients. Ophthalmol Clin North Am 2005;18(3):431-442,vii.
31 Kuchar S, Moster MR, Reamer CB, Waisbourd M. Treatment outcomes of micropulse transscleral cyclophotocoagulation in advanced glaucoma. Lasers Med Sci 2016;31(2):393-396.