Effect of subconjunctival injection with conbercept as an adjuvant to filtration surgery for open angle glaucoma: a prospective randomized interventional 6-month follow-up study
Jing Zhang1, Vikash Vikash2, Ping Wang3, Tian Zheng1, Dong-Lai Chen4, Qing Wang1, Min Ke1
1Department of Ophthalmology, Zhongnan Hospital of Wuhan University, Wuhan 430071, Hubei Province, China
2Department of Gastroenterology and Pathology, Renmin Hospital of Wuhan University, Wuhan 430060, Hubei Province, China
3Department of Ophthalmology, Wuhan Third Hospital-Tongren Hospital of Wuhan University, Wuhan 430060, Hubei Province, China
4Department of Ophthalmology, the Second People's Hospital of Honghu, Honghu 433202, Hubei Province, China
Abstract● AlM: To compare the safety and efficacy of subconjunctival injection with conbercept and 5-fluorouracil (5-FU) for open angle glaucoma (OAG) patients after filtration surgery.● METHODS: As a prospective randomized interventional trial, 36 eyes from 36 patients after OAG surgery were collected and divided randomly into conbercept and 5-FU groups. All patients were subconjunctivally injected with either conbercept (0.2 mL) or 5-FU (0.2 mL) on the 5th day post-operatively. The intraocular pressure (lOP), number of medications used, type of conjunctival bleb, and complications were recorded and analyzed pre-operatively and 1d, 1wk, 1, 3 and 6mo post-injection.● RESULTS: There were significant differences in lOP between the conbercept and 5-FU groups 1mo (conbercept group: 12.17±1.04 mm Hg; 5-FU group: 13.50±2.33 mm Hg,t=2.214, P=0.037), 3mo (conbercept group: 13.00±1.88 mm Hg;5-FU group: 14.50±2.28 mm Hg, t=2.153, P=0.039), and 6mo post-injection (conbercept group: 13.28±2.95 mm Hg; 5-FU group: 15.22±2.49 mm Hg, t=2.140, P=0.040); however, in the number of medications, a prominent difference was not shown between groups on post-injection 6mo (t=1.312,P=0.200). Moreover, there was mild vascularity observed in the conbecept group than the 5-FU group 1d (3a, 3b, 3c:t=8.497, 6.693, 4.515, P=0.000), 1wk (3a, 3b, 3c: t=3.431,6.408, 3.984, P=0.002, 0.000, 0.000), and 1mo post-injection(3a, 3b, 3c: t=2.466, 2.466, 2.503, P=0.019, 0.019, 0.017).Simultaneously, differences from other indicators between the two groups were not demonstrated. Also, there was a lower probability of corneal epithelial stripping in the conbercept group than the 5-FU group (χ2=4.500, P=0.034).● CONCLUSlON: Subconjunctival injection of conbercept has a safe, effective, and tolerable profile for open angle glaucoma patients with distinct conjunctival congestion after filtration surgery.
INTRODUCTION
Currently, filtration surgery, in which the aqueous humour can be drained from the anterior chamber to the bleb formed by the subconjunctival space by creating a guarded fistula, thus resulting in reduction of intraocular pressure (IOP). Filtration surgery is one of the most commonly performed surgical interventions for glaucoma patients who cannot be adequately controlled with medication or laser treatment. Trabeculectomy and ExPress implant surgery, both of which have the same efficacy at reducing IOP[1], are the most common procedures during filtration surgery.
An excessive wound healing response, which gives rise to post-operative subconjunctival and Tenon's capsule scarring through fibroblast proliferation, migration, and contraction,is the main reason for failed filtration surgery[2]. Therefore,increased use of agents, such as 5-fluorouracil (5-FU) and mitomycin-C (MMC), is required to suppress fibroblast activity and increase the success rate of filtration surgery[3]. There is a higher incidence of adverse effects associated with these drugs,including corneal epithelial stripping[4], cystic avascular blebs,bleb leakage, bleb infections, and endophthalmitis[5].It is well-known that anti-vascular endothelial growth factor(VEGF) antibodies can serve as an alternative anti-proliferative and anti-angiogenic agent[6] associated with the precise effect at wound modulation of the filtering bleb, and with fewer adverse effects.
Currently, conbercept [conbercept ophthalmic injection, 10 mg/mL (0.2 mL); Chengdu Kanghong Biotechnologies Co.Ltd., Chengdu, China] is the latest anti-VEGF antibody and a recombinant fusion protein, the vital area of which is composed of the 2nd Ig domain of human VEGFR1, the 3rd and 4th Ig domains of VEGFR2, and the constant Fc region of human IgG1[7]. Moreover, conbercept has a higher binding affinity than natural decoys and monoclonal antibody, and is able to block all isoforms of VEGF-A, VEGF-B, and PIGF.Conbercept had puissant anti-angiogenic and anti-tumor effects by inhibiting VEGF in vitro and in vivo[8].
Some studies have demonstrated the anti-proliferative effects in a variety of anti-VEGF antibodies, such as ranibizumab and bevacizumab[6]. Until now, there have not been any reports demonstrating whether or not conbercept, which is the least expensive anti-VEGF antibody in China, has anti-proliferative action. This study outlines whether or not conbercept has any effects on scarring of filtration blebs, the variation in the IOP,the number of medicines, and the bleb characteristics using the Moorfields bleb grading system (MBGS)[9] for patients with glaucoma after filtration surgery.
SUBJECTS AND METHODS
Ethical Approval Trial registration number: ChiCTRIPC-17011900. A prospective, randomized interventional trial was conducted. All patients were fully informed and voluntarily consented to participate in this study abiding by the institutional guidelines. Institutional Review Board approval was obtained from Zhongnan Hospital of Wuhan University in Wuhan, China. All participants in this study adhered to the tenets of the Declaration of Helsinki. The following principle was embraced: “The refusal of a patient to participate in a study must never interfere with the patient-physician relationship.”
All 36 patients, including 36 eyes, ranged from 18-65 years of age, were represented by both genders, had open angle glaucoma (OAG) and uncontrolled IOP, had been on IOP-lowering medications >1y, and had distinct conjunctival congestion after filtration surgery. The patients were recruited from the Department of Ophthalmology at Zhongnan Hospital of Wuhan University in Wuhan, between Jan 17th, 2017, and Jan 16st, 2018, and were randomly divided into the conbercept and 5-FU groups according to stratified blocked randomization using a random number table (Zhang J). If both eyes were eligible, only the more seriously affected eye was included.
The inclusion criteria were as follows: 1) OAG with uncontrolled IOP by maximum tolerated drugs (>21 mm Hg any time during a 24-hour period, or a >8 mm Hg average daily fluctuation in IOP); 2) poor compliance to medical treatment giving rise to the high probability of glaucoma progression; and 3)progressively glaucomatous optic disc changes or visual field loss.
The exclusion criteria were as follows: 1) other ocular comorbidities, such as keratonosus, lens dislocation, uveitis,retinal diseases, congenital anomalies, or ocular trauma; 2)allergic to conbercept; 3) uncontrolled diabetes or hypertension, or other medical conditions increasing the risk of complications from filter surgery; 4) pregnant or breastfeeding women; and 5) unable to accept the follow-up schedule.
All filtration surgeries were operated by the same surgeon (Ke M) according to the following protocol[10].
A 1-mL syringe with a 29-gauge needle (Ultra-Fine® insulin syringe, 1 mL 29G×1/2; Becton Dickinson and Company,Franklin Lakes, New Jersey, USA) was punctured subconjunctivally adjacent to the bleb,then the scar tissue of the bleb between the conjunctiva and the scleral flap was separated. Subsequently, 0.2 mL of conbercept or 0.2 mL of 5-FU [fluorouracil injection, 10 mL (0.25 g); Tianjin Jin Yao Amino Acid Co. Ltd, Tianjin, China][11] was injected subconjunctivally on the 5th day post-operatively (Zheng T).Then, a wet swab was applied to seal the point following needle removal. Antibiotic eye ointment was instilled in the conjunctival sac and the eye was patched.
Topical tobramycin and dexamethasone eye drops were used 4 times per day for 2wk and tapered off slowly for the following 4-6wk after filtration surgery.
All the patients were examined routinely by the same examiner(Wang Q) blinded pre-operatively and 1d, 1wk, 1, 3, and 6mo post-injection, as follows: corrected distance visual acuity (CDVA) with Snellen's chart (Sanke SL-II, YZB/gui0195-2004; Sanke Medical Co. Ltd., Nanning, China);anterior segment examination with slit-lamp biomicroscopy(66VT YZ5FI, YZB/su 0311 2014; 66 VISION TECH Co.Ltd., Suzhou, China); IOP measurement with a Goldmann applanation tonometer that was calibrated monthly (AT900®;Haag-Streit AG, Koniz, Switzerland); direct funduscopy (66VT YZ6E; 66 VISION TECH Co. Ltd.); gonioscopy (Single Mirror Gonio Lens Diagnostic Lenses Ophthalmic Instruments,LOT 040605; Ocular® Instruments, Inc., Bellevue, WA, USA);visual field perimetry (Humphrey Field Analyzer 740i; Carl Zeiss Meditec, Inc., Dublin, CA, USA); and optic nerve fibrouslayer thickness with optical coherence tomography (CirrusTM HD-OCT 4000; Carl Zeiss Meditec, Inc.). For this analysis, the IOP, number of medications used, type of conjunctival bleb,and complications were recorded by the same investigator(Chen DL) blinded. Conjunctival bleb morphology was graded according to the MBGS grading system by the observer. When describing a bleb, the following three most important aspects were considered: area; height; and vascualarity[9].
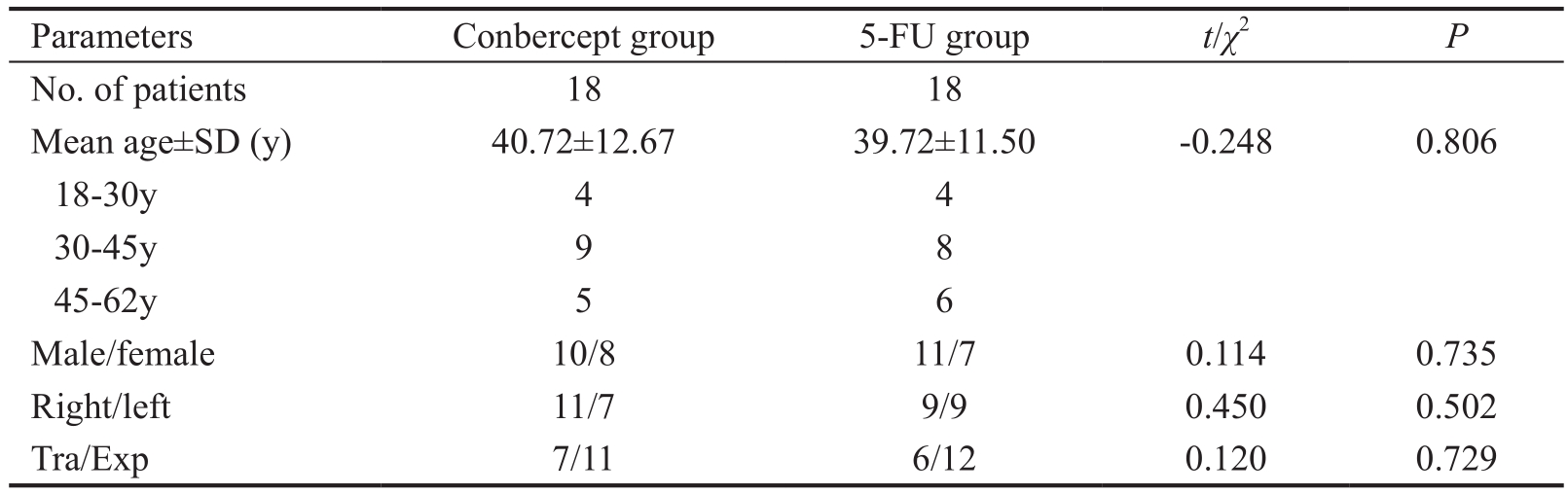
Table 1 Demographic and baseline characteristics of patients
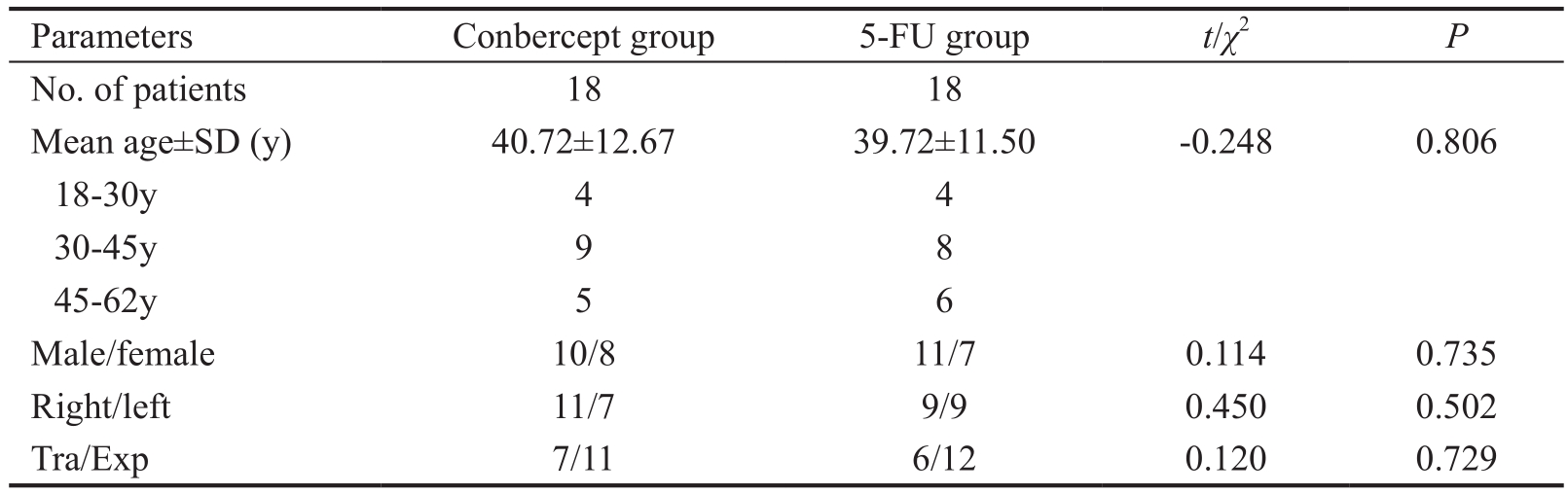
Tra: Trabeculectomy; Exp: ExPress implant surgery.
 No. of patients 18 18 Mean age±SD (y) 40.72±12.67 39.72±11.50 -0.248 0.806 18-30y 4 4 30-45y 9 8 45-62y 5 6 Male/female 10/8 11/7 0.114 0.735 Right/left 11/7 9/9 0.450 0.502 Tra/Exp 7/11 6/12 0.120 0.729
No. of patients 18 18 Mean age±SD (y) 40.72±12.67 39.72±11.50 -0.248 0.806 18-30y 4 4 30-45y 9 8 45-62y 5 6 Male/female 10/8 11/7 0.114 0.735 Right/left 11/7 9/9 0.450 0.502 Tra/Exp 7/11 6/12 0.120 0.729
Table 2 IOP on pre-injection, post-injection 1d, 1wk, 1, 3 and 6mo in both groups mean±SD, mm Hg
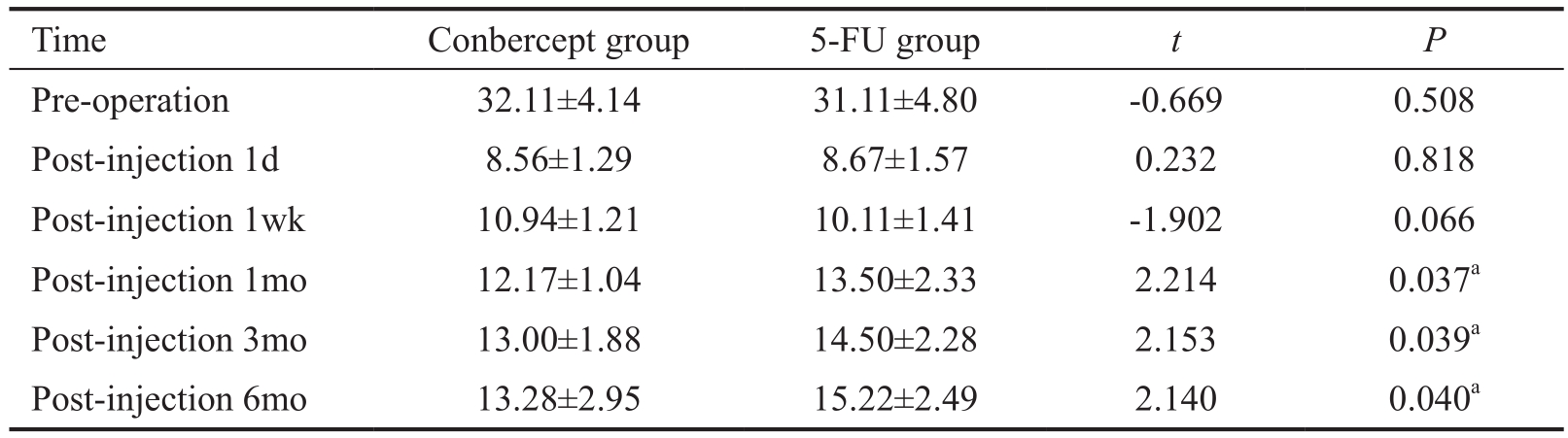
aP<0.05, there was significant difference between conbercept group and 5-FU group in the same viewing time.
 Pre-operation 32.11±4.14 31.11±4.80 -0.669 0.508 Post-injection 1d 8.56±1.29 8.67±1.57 0.232 0.818 Post-injection 1wk 10.94±1.21 10.11±1.41 -1.902 0.066 Post-injection 1mo 12.17±1.04 13.50±2.33 2.214 0.037a Post-injection 3mo 13.00±1.88 14.50±2.28 2.153 0.039a Post-injection 6mo 13.28±2.95 15.22±2.49 2.140 0.040a
Pre-operation 32.11±4.14 31.11±4.80 -0.669 0.508 Post-injection 1d 8.56±1.29 8.67±1.57 0.232 0.818 Post-injection 1wk 10.94±1.21 10.11±1.41 -1.902 0.066 Post-injection 1mo 12.17±1.04 13.50±2.33 2.214 0.037a Post-injection 3mo 13.00±1.88 14.50±2.28 2.153 0.039a Post-injection 6mo 13.28±2.95 15.22±2.49 2.140 0.040a
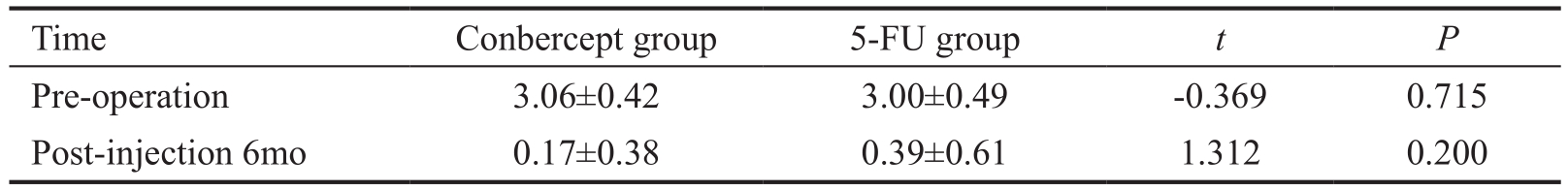
Table 3 No. of medications for pre-operation and post-injection 6mo in both groups mean±SD
 Pre-operation 3.06±0.42 3.00±0.49 -0.369 0.715 Post-injection 6mo 0.17±0.38 0.39±0.61 1.312 0.200
Pre-operation 3.06±0.42 3.00±0.49 -0.369 0.715 Post-injection 6mo 0.17±0.38 0.39±0.61 1.312 0.200
Statistical Analysis The data analysis was performed using SPSS software (version 20.0; SPSS, Inc., Chicago, IL, USA).Independent and paired t-tests were used to evaluate between groups. Proportion material was analyzed using Pearson χ2 tests. A P-value <0.05 was considered statistically significant(Wang P) blinded.
RESULTS
The baseline characteristics of all patients are given in Table 1.There was no statistically significant difference in baseline characteristics between the two groups. All of the patients were of Han ethnicity.
All of the patients had follow-up evaluations. The IOPs between the two groups pre-operatively and 1d, 1w, 1, 3 and 6mo post-injection are summarized in Table 2. In the conbercept group, a statistically significant difference was detected in terms of IOP between pre-operatively compared with 1d (t=23.027, P=0.000), 1wk (t=20.805, P=0.000),1mo (t=19.806, P=0.000), 3mo (t=17.824, P=0.000), and 6mo post-injection (t=15.717, P=0.000). Reduction in the IOP pre-operatively compared with 1d (t=18.851, P=0.000),1wk (t=17.807, P=0.000), 1mo (t=13.999, P=0.000), 3mo(t=13.259, P=0.000), and 6mo post-injection (t=12.469,P=0.000) was statistically significant for the 5-FU group.
The number of medications pre-operatively and 6mo postinjection in both groups is presented in Table 3. Remarkable differences were observed pre-operatively compared with 6mo post-injection in the conbercept (t=21.658, P=0.000)and 5-FU groups (t=14.247, P=0.000). At 6mo post-injection,a significant difference was not demonstrated between the two groups (t=1.312, P=0.200), although the number of medications in the conbercept group was less than the 5-FU group.
The types of conjunctival bleb pre-injection, and 1d, 1wk,1, 3 and 6mo post-injection in both groups were compared in Table 4. One day post-injection there were significant differences in vascularity 3a (t=8.497, P=0.000), 3b (t=6.693,P=0.000), and 3c (t=4.515, P=0.000). One week postinjection striking differences were observed in vascularity 3a(t=3.431, P=0.002), 3b (t=6.408, P=0.000), and 3c (t=3.984,P=0.000). The same results were noted in vascularity 3a, 3b(either t=2.466, P=0.019), and 3c (t=2.503, P=0.017) 1mo post-injection; however, remarkable differences from other indicators were not observed.
Table 4 Types of conjunctival bleb on pre-injection, post-injection 1d, 1wk, 1, 3 and 6mo in both groups mean±SD
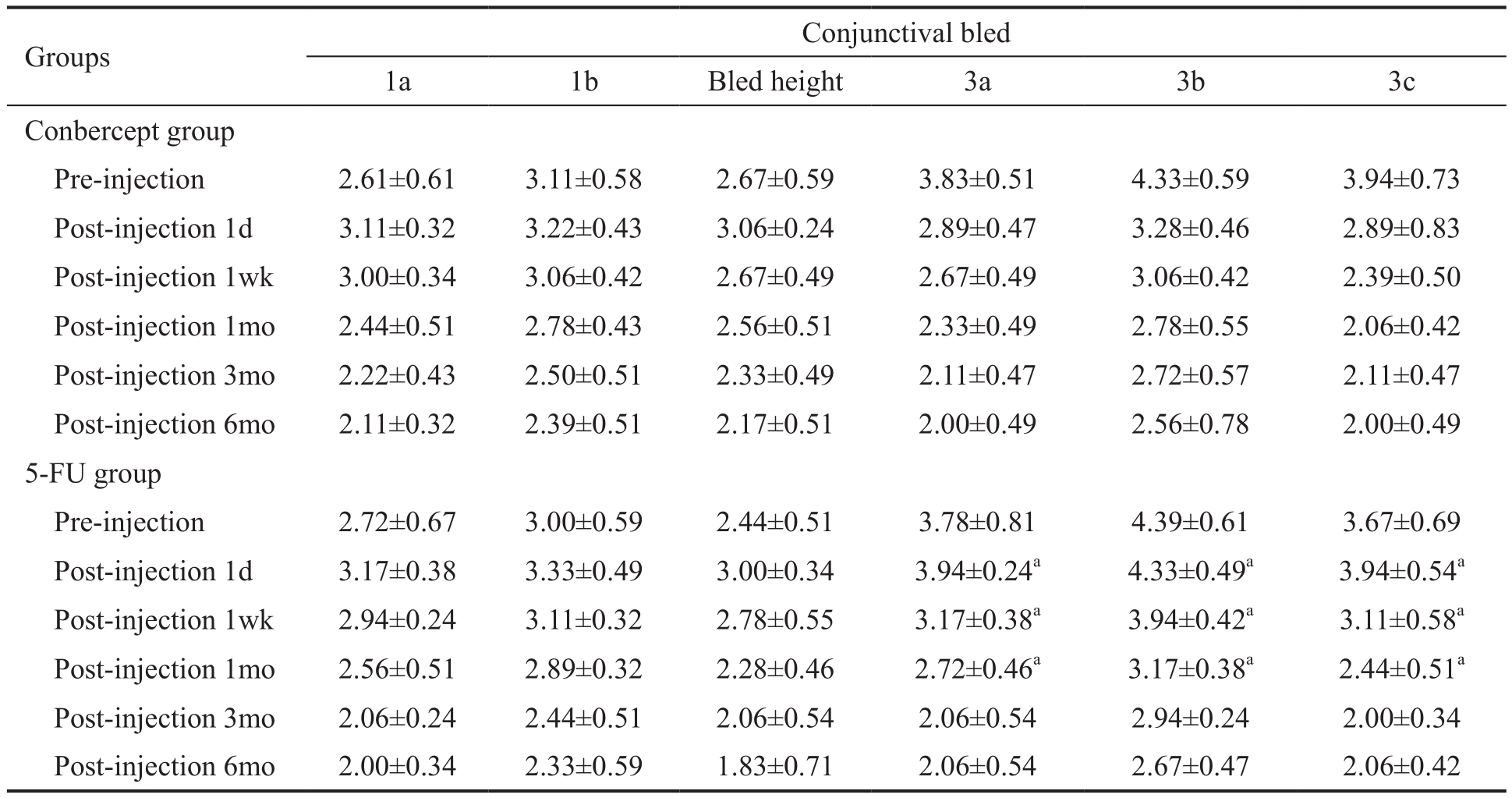
aP<0.05, there was significant difference between conbercept group and 5-FU group in the same viewing time.
 Conbercept group Pre-injection 2.61±0.61 3.11±0.58 2.67±0.59 3.83±0.51 4.33±0.59 3.94±0.73 Post-injection 1d 3.11±0.32 3.22±0.43 3.06±0.24 2.89±0.47 3.28±0.46 2.89±0.83 Post-injection 1wk 3.00±0.34 3.06±0.42 2.67±0.49 2.67±0.49 3.06±0.42 2.39±0.50 Post-injection 1mo 2.44±0.51 2.78±0.43 2.56±0.51 2.33±0.49 2.78±0.55 2.06±0.42 Post-injection 3mo 2.22±0.43 2.50±0.51 2.33±0.49 2.11±0.47 2.72±0.57 2.11±0.47 Post-injection 6mo 2.11±0.32 2.39±0.51 2.17±0.51 2.00±0.49 2.56±0.78 2.00±0.49 5-FU group Pre-injection 2.72±0.67 3.00±0.59 2.44±0.51 3.78±0.81 4.39±0.61 3.67±0.69 Post-injection 1d 3.17±0.38 3.33±0.49 3.00±0.34 3.94±0.24a 4.33±0.49a 3.94±0.54a Post-injection 1wk 2.94±0.24 3.11±0.32 2.78±0.55 3.17±0.38a 3.94±0.42a 3.11±0.58a Post-injection 1mo 2.56±0.51 2.89±0.32 2.28±0.46 2.72±0.46a 3.17±0.38a 2.44±0.51a Post-injection 3mo 2.06±0.24 2.44±0.51 2.06±0.54 2.06±0.54 2.94±0.24 2.00±0.34 Post-injection 6mo 2.00±0.34 2.33±0.59 1.83±0.71 2.06±0.54 2.67±0.47 2.06±0.42
Conbercept group Pre-injection 2.61±0.61 3.11±0.58 2.67±0.59 3.83±0.51 4.33±0.59 3.94±0.73 Post-injection 1d 3.11±0.32 3.22±0.43 3.06±0.24 2.89±0.47 3.28±0.46 2.89±0.83 Post-injection 1wk 3.00±0.34 3.06±0.42 2.67±0.49 2.67±0.49 3.06±0.42 2.39±0.50 Post-injection 1mo 2.44±0.51 2.78±0.43 2.56±0.51 2.33±0.49 2.78±0.55 2.06±0.42 Post-injection 3mo 2.22±0.43 2.50±0.51 2.33±0.49 2.11±0.47 2.72±0.57 2.11±0.47 Post-injection 6mo 2.11±0.32 2.39±0.51 2.17±0.51 2.00±0.49 2.56±0.78 2.00±0.49 5-FU group Pre-injection 2.72±0.67 3.00±0.59 2.44±0.51 3.78±0.81 4.39±0.61 3.67±0.69 Post-injection 1d 3.17±0.38 3.33±0.49 3.00±0.34 3.94±0.24a 4.33±0.49a 3.94±0.54a Post-injection 1wk 2.94±0.24 3.11±0.32 2.78±0.55 3.17±0.38a 3.94±0.42a 3.11±0.58a Post-injection 1mo 2.56±0.51 2.89±0.32 2.28±0.46 2.72±0.46a 3.17±0.38a 2.44±0.51a Post-injection 3mo 2.06±0.24 2.44±0.51 2.06±0.54 2.06±0.54 2.94±0.24 2.00±0.34 Post-injection 6mo 2.00±0.34 2.33±0.59 1.83±0.71 2.06±0.54 2.67±0.47 2.06±0.42
Table 5 Complications in both groups n=18

aP<0.05, there was significant difference between conbercept group and 5-FU group.
 Corneal epithelial stripping 0 4 4.500 0.034a Temporary bleb leak 0 2 2.118 0.146 Encapsulated blebs 1 2 0.364 0.546 Transient anterior chamber shallowing 0 0 Endophthalmitis 0 0 Hypotony (IOP<5 mm Hg) 0 0 Bleb failure (IOP>21 mm Hg) 2 5 1.596 0.206
Corneal epithelial stripping 0 4 4.500 0.034a Temporary bleb leak 0 2 2.118 0.146 Encapsulated blebs 1 2 0.364 0.546 Transient anterior chamber shallowing 0 0 Endophthalmitis 0 0 Hypotony (IOP<5 mm Hg) 0 0 Bleb failure (IOP>21 mm Hg) 2 5 1.596 0.206
Complications The complications which occurred in both groups are recorded in Table 5. No patients had intraoperative complications. Corneal epithelial stripping occurred in four eyes of the 5-FU group and none in the conbercept group (χ2=4.500, P=0.034). In two eyes of the 5-FU group,temporary bleb leakage was demonstrated, whereas temporary bleb leakage was not reported in the other group (χ2=2.118,P=0.146). The formation of encapsulated blebs, which would result in localizing filtering blebs and an elevated IOP disappeared in one eye from the conbercept group and two eyes from the 5-FU group (χ2=0.364, P=0.546). The IOP of two eyes from the conbercept group and five eyes from the 5-FU group were exceeded 21 mm Hg (χ2=1.596, P=0.206).In both groups, no transient anterior chamber shallowing,endophthalmitis, and hypotony was reported.
DISCUSSION
It is well-documented that one of the common reasons for failing to control IOP is excessive wound healing and overscarring after filtration surgery, which may occur at the surfaces of the Tenon capsule, under the conjunctiva, and above the intermediate episclera; the failure rate can reach 15%-30%[5,12-13].
Fibroblasts, which play a significant role in scar formation in filtering blebs, are regarded as the primary effector cells of wound healing and in the Tenon capsule[12]. Furthermore,according to some reports, use of IOP-lowering medications pre-operatively >1y is associated with a prominent increase in the content of granulocyte-macrophage colony, other inflammatory cells, and fibroblasts in the conjunctiva and Tenon capsule specimen of filtering surgery[14]. Also, there is an increased rate of IOP dysregulation, lower achievement ratio of surgery, and higher frequency of filtering bleb scarring[15] for the same patients post-operatively. Maximum proliferation of subconjunctival fibroblasts are detected in histologic studies on the 3rd-5th post-operative days[13]. Currently, the most frequently used anti-proliferative drugs which inhibit scarring are 5-FU and MMC. There is a definite therapeutic effect, but there are some side effects associated with 5-FU and MMC, such as corneal epithelial stripping, bleb leakage, transient anterior chamber shallowing, and encapsulated blebs[11,13,16].
Therefore, a safe agent with low toxicity has long been an important matter for filtration surgery of OAG.
Cheng et al[17] reported that bevacizumab improves the outcome of filtration surgery and reduces complications significantly. Furthermore, bevacizumab dramatically inhibited the angiogenic factor (VEGF) and inflammation factors (TGF-β1 and TGF-β2). Noh et al[18] reported that ranibizumab, as an angiogenesis inhibitor, could inhibit fibroblast proliferation and migration from the human Tenon capsule in vitro. Sufficient evidence has demonstrated that VEGF has an effect on fibroblastic activity, not only via angiogenesis,but also directly[19]. Regarded as a mediator and regulator[20],VEGF promotes inflammatory cells to reach the center of the reparative process, which increases fibroblasts migration. The higher the VEGF levels in the aqueous of glaucoma patients who have undergone filtration surgery, as well as the levels of other cytokines, the higher the risk of scarring[13,17]. It has been demonstrated from recent surveys that angiogenesis inhibitors impact scar formation in the skin by altering collagen deposition and reducing wound healing[21], which improves the density of blood vessels by increasing the content of VEGF[22]. Therefore, an anti-VEGF drug which restrains not only neovascularization, but also suppresses scar formation enhances its efficacy.
Ming et al[23] had reported 7-17d in the holding aspect and 11.93±2.23d in average survival time for filtering blebs on the surface of vascularization in rats. Concurrently, proliferating fusiform or star-shaped fibroblasts were noted 5d postoperatively and expanding blood vessels upon the filtering bleb were discovered 7d post-operatively. Given these findings,the designers chose to inject the drug into the subconjunctiva on the 5th day post-operatively to inhibit vascularization and fibroblast proliferation.
Also, the complications from the subconjunctival injection of anti-VEGF drugs, such as bevacizumab and ranibizumab,were fewer than anti-proliferative drugs. Akkan and Cilsim[24]indicated that there was inhibition on scar formation of filtering blebs after filtration surgery for glaucoma patients; however, it was incontestable that the drugs were too expensive in China.The newest and less expensive anti-VEGF drug (conbercept) is affordable. Therefore, we made a plan to determine whether or not conbercept is safe and effective in suppressing the scarring process through subconjunctival injection after filtration surgery.
In our study, significant reductions of IOPs were reported 1d,1wk, 1, 3 and 6mo post-injection in comparison with preoperatively in the conbercept group. There were significant decreases in IOPs in the conbercept group in comparison with the 5-FU group 1, 3 and 6mo post-injection. Moreover, 6mo post-injection the number of medications for decreasing IOP was less than pre-operatively in each group; however, there was no statistical diversity observed between both groups 6mo post-injection. Moreover, there were less values of vascularity 3a, 3b, and 3c in the conbercept group than the 5-FU group 1d,1wk, and 1mo post-injection. Simultaneously, the statistical differences between the two groups for other indices, such as bleb area 1a, 1b, and height, at the same viewing time were not demonstrated. There was more frequent corneal epithelial stripping in the 5-FU group than the conbercept group.
Hence, the congestion extent of filtering blebs and conjunctiva was distinct prior to 5-FU, although there were no noticeable differences in alleviating IOP, number of medications, and bleb area 1a, 1b and height between subconjunctival injection of conbercept and 5-FU for OAG patients undergoing filtration surgery who had used long-term lowering IOP medications.There were fewer complications for subconjunctival injection of conbercept than 5-FU.
In summary, nearly all data proved that subconjunctival injection of conbercept has a safe, effective, and tolerable profile. Although our study provides insight into advantages of subconjunctival injection of conbercept for glaucoma after surgery, there is still some work to be done, such as comparing the curative effect of the other anti-VEGF drugs (bevacizumab or ranibizumab), increasing the number of clinical samples and lengthening the observation time.
ACKNOWLEDGEMENTS
Conflicts of Interest: Zhang J, None; Vikash V, None; Wang P, None; Zheng T, None; Chen DL, None; Wang Q, None;Ke M, None.
REFERENCES
1 Wang W, Zhou MW, Huang WB, Gao XB, Zhang XL. Ex-PRESS implantation versus trabeculectomy in Chinese patients with POAG:fellow eye pilot study. Int J Ophthalmol 2017;10(1):56-60.
2 Khaw PT, Occleston NL, Schultz G, Grierson I, Sherwood MB,Larkin G. Activation and suppression of fibroblast function. Eye (Lond)1994;8(2):188-195.
3 Yamanaka O, Kitano-Izutani A, Tomoyose K, Reinach PS. Pathobiology of wound healing after glaucoma filtration surgery. BMC Ophthalmol 2015;15(Suppl 1):157.
4 Wu KY, Lai YH, Yang YC, Wu WC, Hong SJ. 5- fluorouracil-induced apoptosis changes in cultured corneal epithelial cells. J Ocul Pharmacol Ther 2016;32(3):155-162.
5 Zahid S, Musch DC, Niziol LM, Lichter PR. Risk of endophthalmitis and other long-term complications of trabeculectomy in the collaborative initial glaucoma treatment study (CIGTS). Am J Ophthalmol 2013;155(4):674-680.e1.
6 Lytvynchuk L, Sergienko A, Lavrenchuk G, Petrovski G.Antiproliferative, apoptotic, and autophagic activity of ranibizumab,bevacizumab, pegaptanib, and a flibercept on fibroblasts: implication for choroidal neovascularization. J Ophthalmol 2015;2015:1-10.
7 Wu ZG, Zhou P, Li XX, Wang H, Luo DL, Qiao HY, Ke X, Huang J.Structural characterization of a recombinant fusion protein by instrumental analysis and molecular modeling. PLoS One 2013;8(3):e57642.
8 Wang F, Bai YJ, Yu WZ, Han N, Huang L, Zhao M, Zhou AY, Zhao MW, Li XX. Anti-angiogenic effect of KH902 on retinal neovascularization.Graefes Arch Clin Exp Ophthalmol 2013;251(9):2131-2139.
9 Wells AP, James K, Birchall W, Wong T. Information loss in 2 bleb grading systems. J Glaucoma 2007;16(2):246-250.
10 Shum JW, Choy BN, Ho WL, Chan JC, Lai JS. Consensual ophthalmotonic reaction in Chinese patients following augmented trabeculectomy or ExPRESS shunt implantation. Medicine 2016;95(29):e4190.
11 Liu W, Wang JR, Zhang MM, Tao Y, Sun Y. Comparison of subconjunctival mitomycin C and 5-fluorouracil injection for needle revision of early failed trabeculectomy blebs. J Ophthalmol 2016;2016:1-6.
12 Rubin B, Chan CC, Burnier M, Munion L, Freedman J.Histopathologic study of the Molteno glaucoma implant in three patients.Am J Ophthalmol 1990;110(4):371-379.
13 Masoumpour MB, Nowroozzadeh MH, Razeghinejad MR. Current and future techniques in wound healing modulation after glaucoma filtering surgeries. Open Ophthalmol J 2016;10:68-85.
14 Galbis-Estrada C, Pinazo-Durán MD, Cantú-Dibildox J, Marco-Ramírez C, Díaz-Llópis M, Benítez-del-Castillo J. Patients undergoing Long-term treatment with antihypertensive eye drops responded positively with respect to their ocular surface disorder to oral supplementation with antioxidants and essential fatty acids. Clin Interv Aging 2013;8:711-719.
15 Boimer C, Birt CM. Preservative exposure and surgical outcomes in glaucoma patients: the PESO study. J Glaucoma 2013;22(9):730-735.
16 Chen DZ, Koh V, Sng C, Aquino MC, Chew P. Complications and outcomes of primary phacotrabeculectomy with mitomycin C in a multiethnic Asian population. PLoS One 2015;10(3):e0118852.
17 Cheng GW, Xiang H, Yang GX, Ma JM, Zhao JL. Bevacizumab inhibits angiogenesis and inflammation in rat filtration surgery model.Cell Biochemistry and Biophysics 2015;73(1):71-77.
18 Noh SM, Abdul Kadir SH, Crowston JG, Subrayan V, Vasudevan S.Effects of ranibizumab on TGF-β1 and TGF-β2 production by human Tenon's fibroblasts: an in vitro study. Mol Vis 2015;21:1191-1200.
19 Park YM, Kim CD, Lee JS. Effect of bevacizumab on human tenon's fibroblasts cultured from primary and recurrent pterygium. Korean J Physiol Pharmaco 2015;19(4):357-363.
20 Jang HJ, Tsoyi K, Kim YM, Park EJ, Park SW, Kim HJ, Lee JH, Chang KC.(S)-1-α-naphthylmethyl-6, 7-dihydroxy-1, 2, 3, 4-tetrahydroisoquinoline(CKD712), promotes wound closure by producing VEGF through HO-1 induction in human dermal fibroblasts and mouse skin. Br J Pharmacol 2013;168(6):1485-1496.
21 Wang P, Jiang LZ, Xue B. Recombinant human endostatin reduces hypertrophic scar formation in rabbit ear model through down-regulation of VEGF and TIMP-1. Afr Health Sci 2016;16(2):542-553.
22 Wang CG, Wang QQ, Gao WD, Zhang ZJ, Lou YT, Jin HM, Chen XF, Lei B, Xu HZ, Mao C. Highly efficient local delivery of endothelial progenitor cells significantly potentiates angiogenesis and full-thickness wound healing. Acta Biomaterialia 2018;69:156-169.
23 Ming P, Wang L, Wang D, et al. Dynamic changes of morphology and histopathology of conjunctival filtering bleb after anti-glaucoma filtering surgery in rat. Chin J Exp Ophthalmol 2014;32(10):886-890.
24 Akkan JU, Cilsim S. Role of subconjunctival bevacizumab as an adjuvant to primary trabeculectomy. J Glaucoma 2015;24(1):1-8.
Correspondence to: Min Ke. Department of Ophthalmology,Zhongnan Hospital of Wuhan University, No.169, Donghu Road, Wuhan 430071, Hubei Province, China. keminyk@163.com Received: 2018-03-23 Accepted: 2018-08-01
● KEYWORDS: filtration surgery; conbercept; 5- fluorouracil;open angle glaucoma
DOl:10.18240/ijo.2019.02.08
Citation: Zhang J, Vikash V, Wang P, Zheng T, Chen DL, Wang Q, Ke M. Effect of subconjunctival injection with conbercept as an adjuvant to filtration surgery for open angle glaucoma: a prospective randomized interventional 6-month follow-up study. Int J Ophthalmol 2019;12(2):235-240
 No. of patients 18 18 Mean age±SD (y) 40.72±12.67 39.72±11.50 -0.248 0.806 18-30y 4 4 30-45y 9 8 45-62y 5 6 Male/female 10/8 11/7 0.114 0.735 Right/left 11/7 9/9 0.450 0.502 Tra/Exp 7/11 6/12 0.120 0.729
No. of patients 18 18 Mean age±SD (y) 40.72±12.67 39.72±11.50 -0.248 0.806 18-30y 4 4 30-45y 9 8 45-62y 5 6 Male/female 10/8 11/7 0.114 0.735 Right/left 11/7 9/9 0.450 0.502 Tra/Exp 7/11 6/12 0.120 0.729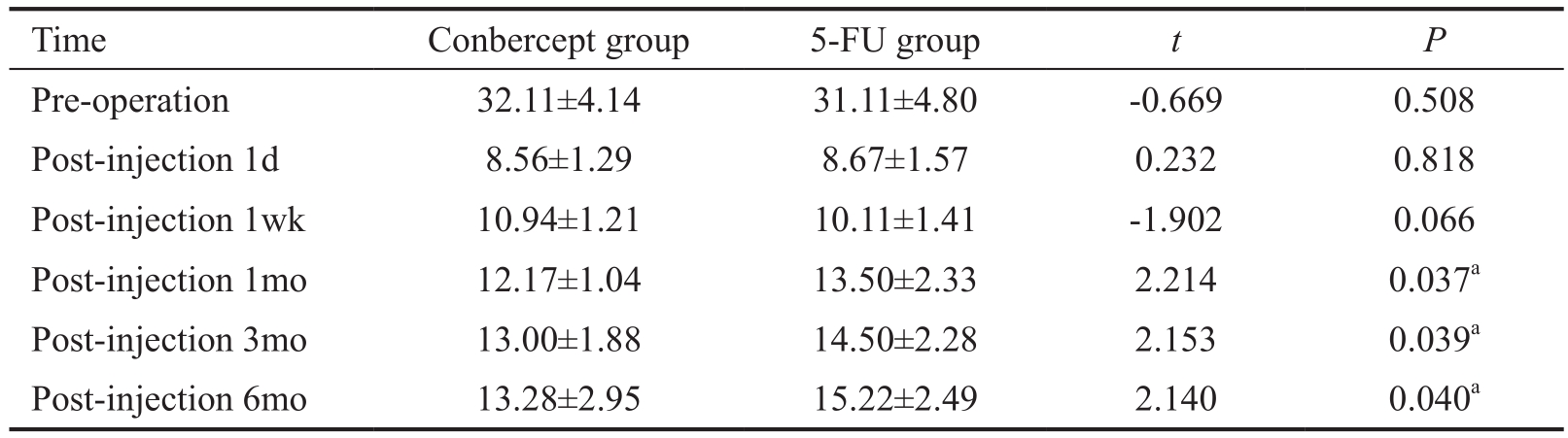
 Pre-operation 32.11±4.14 31.11±4.80 -0.669 0.508 Post-injection 1d 8.56±1.29 8.67±1.57 0.232 0.818 Post-injection 1wk 10.94±1.21 10.11±1.41 -1.902 0.066 Post-injection 1mo 12.17±1.04 13.50±2.33 2.214 0.037
Pre-operation 32.11±4.14 31.11±4.80 -0.669 0.508 Post-injection 1d 8.56±1.29 8.67±1.57 0.232 0.818 Post-injection 1wk 10.94±1.21 10.11±1.41 -1.902 0.066 Post-injection 1mo 12.17±1.04 13.50±2.33 2.214 0.037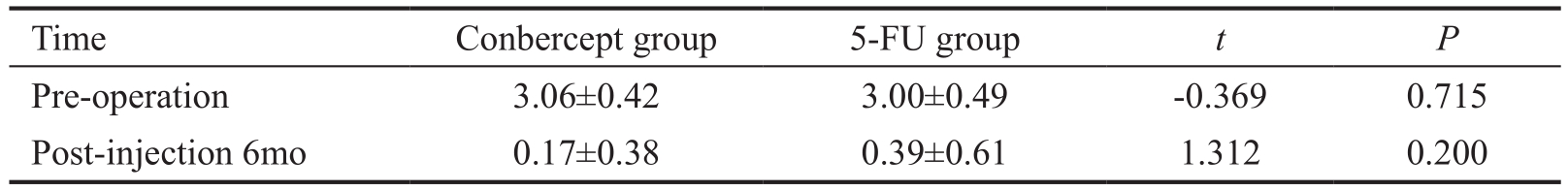
 Pre-operation 3.06±0.42 3.00±0.49 -0.369 0.715 Post-injection 6mo 0.17±0.38 0.39±0.61 1.312 0.200
Pre-operation 3.06±0.42 3.00±0.49 -0.369 0.715 Post-injection 6mo 0.17±0.38 0.39±0.61 1.312 0.200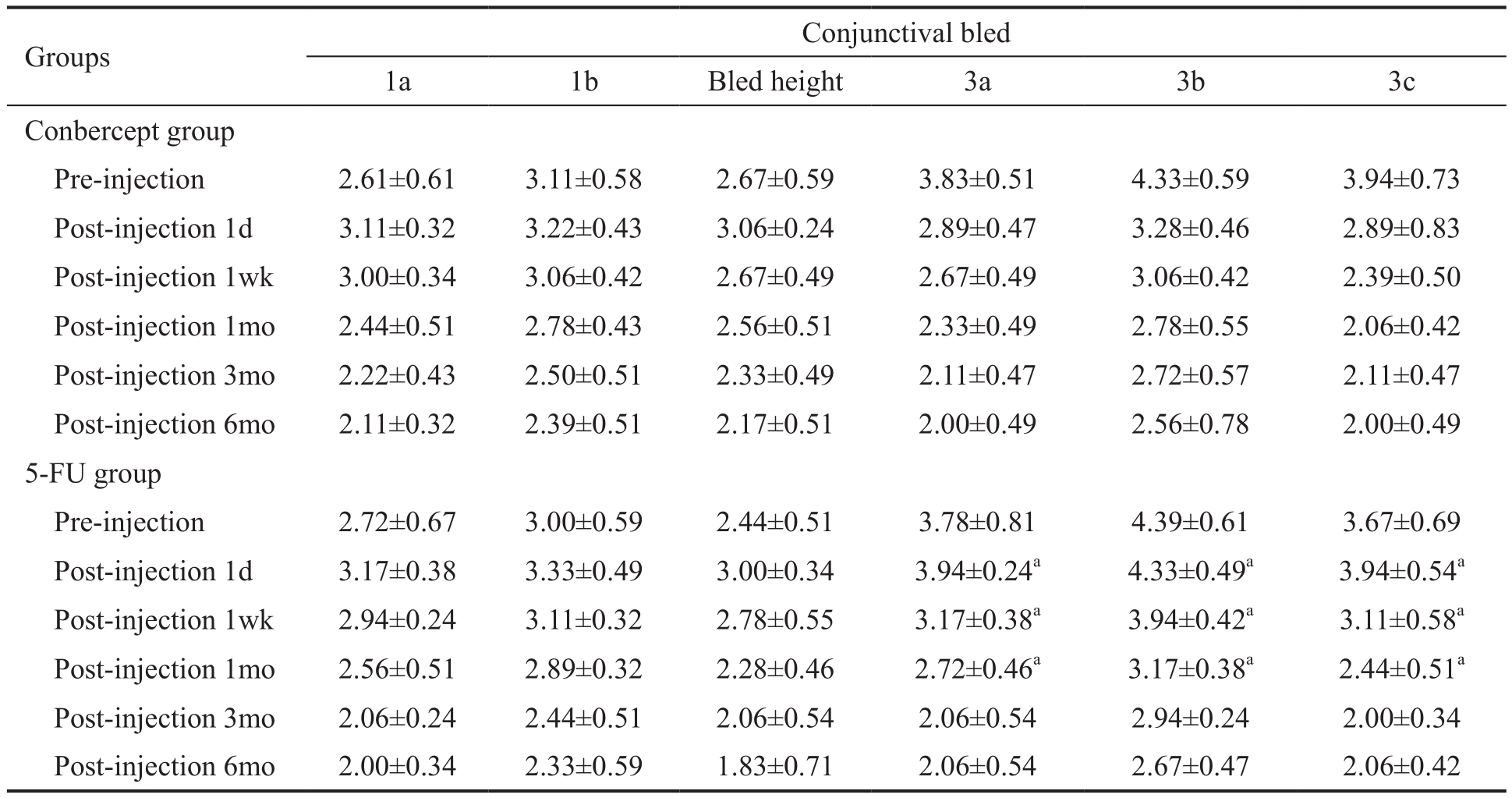
 Conbercept group Pre-injection 2.61±0.61 3.11±0.58 2.67±0.59 3.83±0.51 4.33±0.59 3.94±0.73 Post-injection 1d 3.11±0.32 3.22±0.43 3.06±0.24 2.89±0.47 3.28±0.46 2.89±0.83 Post-injection 1wk 3.00±0.34 3.06±0.42 2.67±0.49 2.67±0.49 3.06±0.42 2.39±0.50 Post-injection 1mo 2.44±0.51 2.78±0.43 2.56±0.51 2.33±0.49 2.78±0.55 2.06±0.42 Post-injection 3mo 2.22±0.43 2.50±0.51 2.33±0.49 2.11±0.47 2.72±0.57 2.11±0.47 Post-injection 6mo 2.11±0.32 2.39±0.51 2.17±0.51 2.00±0.49 2.56±0.78 2.00±0.49 5-FU group Pre-injection 2.72±0.67 3.00±0.59 2.44±0.51 3.78±0.81 4.39±0.61 3.67±0.69 Post-injection 1d 3.17±0.38 3.33±0.49 3.00±0.34 3.94±0.24
Conbercept group Pre-injection 2.61±0.61 3.11±0.58 2.67±0.59 3.83±0.51 4.33±0.59 3.94±0.73 Post-injection 1d 3.11±0.32 3.22±0.43 3.06±0.24 2.89±0.47 3.28±0.46 2.89±0.83 Post-injection 1wk 3.00±0.34 3.06±0.42 2.67±0.49 2.67±0.49 3.06±0.42 2.39±0.50 Post-injection 1mo 2.44±0.51 2.78±0.43 2.56±0.51 2.33±0.49 2.78±0.55 2.06±0.42 Post-injection 3mo 2.22±0.43 2.50±0.51 2.33±0.49 2.11±0.47 2.72±0.57 2.11±0.47 Post-injection 6mo 2.11±0.32 2.39±0.51 2.17±0.51 2.00±0.49 2.56±0.78 2.00±0.49 5-FU group Pre-injection 2.72±0.67 3.00±0.59 2.44±0.51 3.78±0.81 4.39±0.61 3.67±0.69 Post-injection 1d 3.17±0.38 3.33±0.49 3.00±0.34 3.94±0.24
 Corneal epithelial stripping 0 4 4.500 0.034
Corneal epithelial stripping 0 4 4.500 0.034