Clinical outcomes with large macular holes using the tiled transplantation internal limiting membrane pedicle flap technique
Li-Ping Wang, Wen-Tao Sun, Chun-Ling Lei, Jin Deng
Department of Ophthalmology, Shaanxi Ophthalmic Medical Center, Xi'an Fourth Hospital, Affiliated Guangren Hospital,School of Medicine, Xi'an Jiaotong University, Xi'an 710004,Shaanxi Province, China
Abstract● AlM: To report the surgical technique and efficacy of the tiled transplantation internal limiting membrane (lLM)pedicle flap technique after vitrectomy for 33 patients with large macular hole (MH).● METHODS: This study was a prospective noncontrolled interventional study. All patients were treated by vitrectomy, the tiled transplantation lLM pedicle flap and gas tamponade.All patients underwent visual acuity measurements and optical coherence tomography (OCT), during preoperative and the follow-up visits postoperative.● RESULTS: Two high-myopic patient had flap dislocation during surgery. The thorough closure of MH following the tiled transplantation lLM pedicle flap technique was ultimately achieved in 31 patients observed by OCT imaging (93.94%) 1wk after surgery. Visual acuity improved from 1.51±0.31 (logMAR) preoperative to 0.92±0.30 6mo after surgery (P=0.000). There were no significant changes in OCT finding during the follow-up period from 1mo to 6mo after surgery.● CONCLUSlON: The tiled transplantation lLM pedicle flap technique provides bridge for retinal gliosis to achieve successful closures of the large MHs, and the microenvironment of this technique is more similar to the normal physiological conditions.
INTRODUCTION
M acular hole (MH) is the full thickness defect of the retinal neuroepithelium in the macular fovea leading to the loss of central vision[1]. Vitrectomy, internallimiting membrane (ILM) peeling, and gas tamponade is a well established method for the treatment of idiopathic MHs.Despite ILM removal, surgical closure of large MH remains challenging. There were many methods for treating large MHs have been reported, such as inverted ILM flap technique,using whole blood as an adhesive to aid in the fixation of an autologous neurosensory retinal free flap[2], the transplantation of lens capsular flap and the autologous serum application[3],and so on. Michalewska et al[4] first reported the inverted ILM flap technique can improve the postoperative visual acuity and the closure rate (98%) of MHs larger than 400 μm in diameter[5]. The closure rate of myopic MHs was 80% using this technique was reported by Kuriyama et al[6]. Michalewska et al[4,7] also reported that this technology stimulated the glial cells proliferation, establishing bridges between retinal tissue defects in the holes.
If the inverted ILM flap can play a role as a bridge to promote proliferation of glial cells, then we speculate that the tiled transplantation ILM pedicle flap can play the same role. In our clinical report, we describe the clinical effects of tiled transplantation ILM pedicle flap technique in the treatment of large MHs (diameter greater than 400 μm) including idiopathic, in myopic eyes and traumatic MHs.
SUBJECTS AND METHODS
Ethical Approval This study is a prospective noncontrolled interventional study conducted at the Xi'an No.4 Hospital,Xi'an, China. Institute Ethics Committee approval was obtained.The study followed the principles of the Declaration of Helsinki.Each patient was informed about the risks and benefits of the surgery and their written informed consent was obtained.
We analyzed the medical records of patients using pars plana vitrectomy (PPV) and the tiled transplantation ILM pedicle flap technique for the treatment of large MHs in the Xi'an No.4 Hospital, between September 2016 and May 2018.The inclusion criteria were as follows: minimum diameter of MH≥400 μm; clinical presentation of MH without retinal detachment (RD); intraocular pressure (IOP) <21 mm Hg.Exclusion criteria were a history of RD or proliferative vitreoretinopathy, any kind of retinal surgery, vitreous hemorrhage, optic atrophy, ocular tumors, and glaucoma.
All patients underwent a comprehensive ophthalmological examination before and after surgery, including determining the best corrected visual acuity (BCVA; recorded in snellen visual acuity ratios and was converted to logMAR units for statistical analysis), axial length (Master), IOP (Auto-tonometer TX-20, Canon, Tokyo, Japan), and the posterior segment biomicroscopy using a 90 diopter (D) lens on a slit lamp. The anatomic status of MH preoperative and postoperative were checked using optical coherence tomography (OCT; Spectralis HRA+OCT, Heidelberg, Germany). At least 6mo follow-up period was required after the surgery.
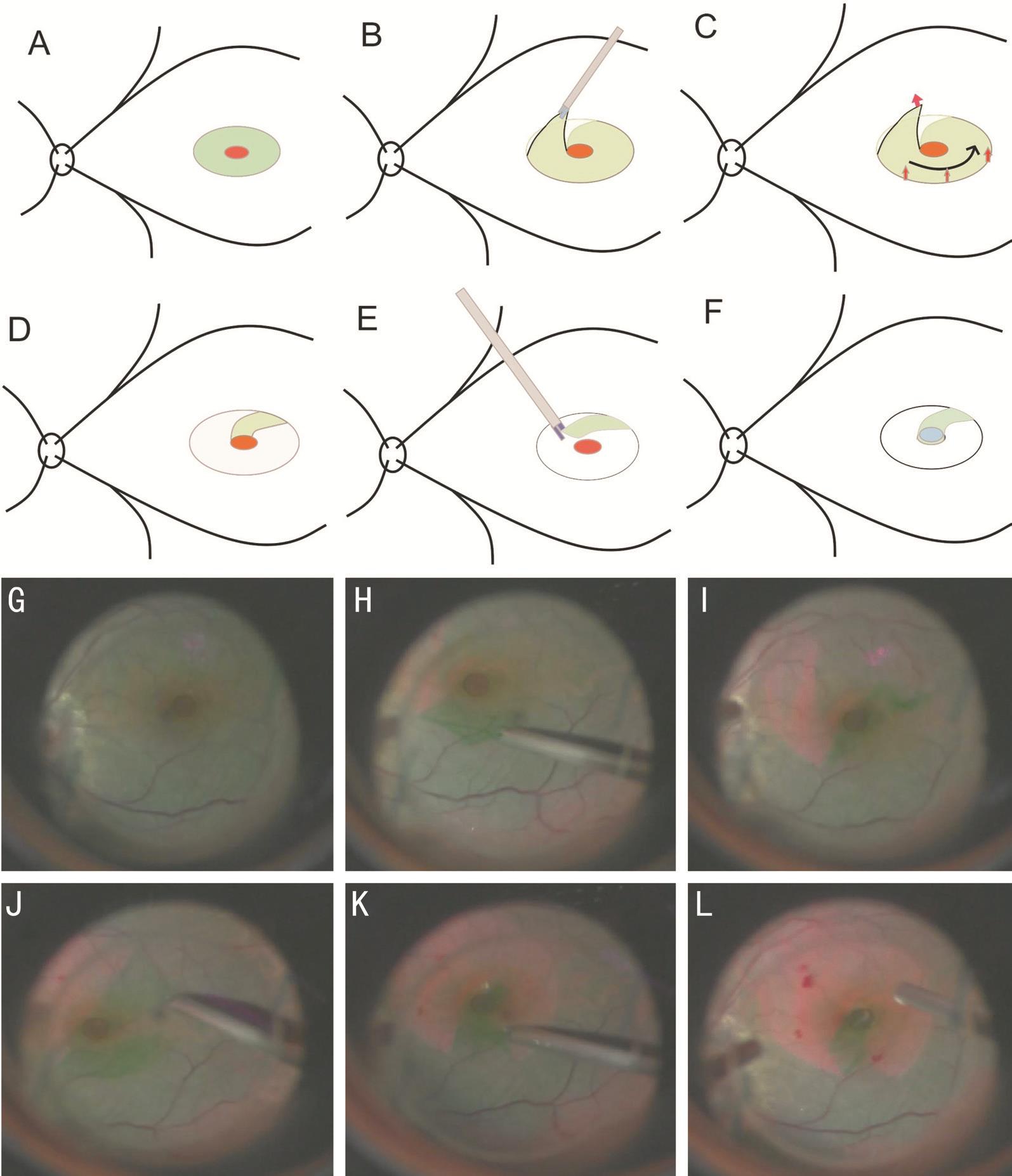
Surgical ProcedureA standard 23-gauge PPV (Constellation Vision System, Alcon Laboratories, Inc., Fort Worth, TX,USA) with the tiled transplantation ILM pedicle flap technique was performed in all patients by a single experienced surgeon.Separate vitrectomy was performed in eyes without cataracts and pseudophakic eyes, and phacoemulsi fication (PEA) with intraocular lens (IOL) implantation were performed in cataract eyes additionally. After a core vitrectomy, posterior vitreous detachment was created assisted by triamcinolone acetonide,followed by removal of the residual posterior vitreous cortex.In order to more clearly visibility, the ILM was stained with a 0.125% solution of indocyanine green (ICG), as described by Shah et al[8]. After that, the ILM was grasped and peeled off in a circumferential pattern for about 2-3 disk diameter around the MH using ILM forceps, leaving a pedunculated ILM flap.Then, the ILM flap was gently peeled off along the edge of the circle, and the width of flap should be larger than or equal to the MH diameter. Then the ILM pedicle flap was tiled over the MH, and was carefully fl attened to make sure it was properly positioned. The sodium chondroitin sulfate-sodium hyaluronate(Alcon corporation, Inc., Fort Worth, TX, USA) was placed on the pedicle flap to stabilize it when needed (Figure 1).
To avoid the ILM flap being washed away, we need gentle operation and the lowest level of perfusion pressure (30 cm H2O) that the vitrectomy machine allowed during the airfluid exchange. In all patients, the sterilized air was filled in the vitreous cavity to secure the position of the ILM flap.Each patient was required to remain face down for at least 7d postoperatively. All patients underwent IOP, visual acuity measurements, slit-lamp examinations, OCT and indirect ophthalmoscopy assessments, during the follow-up period at 1d, 1wk and at 1, 3, 6mo postoperatively.
Statistical analysis was performed by SPSS 25.0 for windows(SPSS, Inc., Chicago, IL, USA). Numerical variables were presented as mean±standard deviation (SD). BCVAs at different time points (baseline, 1 and 6mo after surgery)were compared pair wisely by post-hoc tests after analysis of repeated measures ANOVA using general linear model. A value of P<0.05 was considered to be statistically significant.
RESULTS
In all, 24 women (72.7%) and 9 men (27.3%) were included in our study. The age of patients ranged from 19 to 71y (mean 56.82±10.72y). This study involved 19 right eyes and 14 left eyes. At least 6mo follow-up period was required after the surgery. All the 33 patients displayed large MHs, including one traumatic MH, nine high-myopic MHs, and twenty-three idiopathic MHs. The preoperative visual acuity in the affected eye ranged from 20/2000 to 20/200. The shape of some holes approximately resemble truncated cone. In these eyes the minor diameter (D) of MHs ranged from 429 to 767 mm with a mean of 602 mm. The major D of MHs ranged from 765 to 1573 mm with a mean of 1189 mm. The axial length of all patients ranged from 20.97 to 30.15 mm (mean 23.94±2.75 mm). The axial length of high-myopic patients ranged from 25.95 to 30.15 mm(mean 28.10±1.42 mm). Fourteen patients received PPV, PEA and IOL implantation, while eight patients previously had pseudophakic eyes preoperative, and eleven patients retained the transparent lens in the surgery. Surgeon stained the ILM with a 0.125% solution of ICG in all patients. Of 31 patients underwent successful tiled transplantation ILM pedicel flap.Two high-myopic patients had flap dislocation during surgery.No surgical complications were found in all patients.
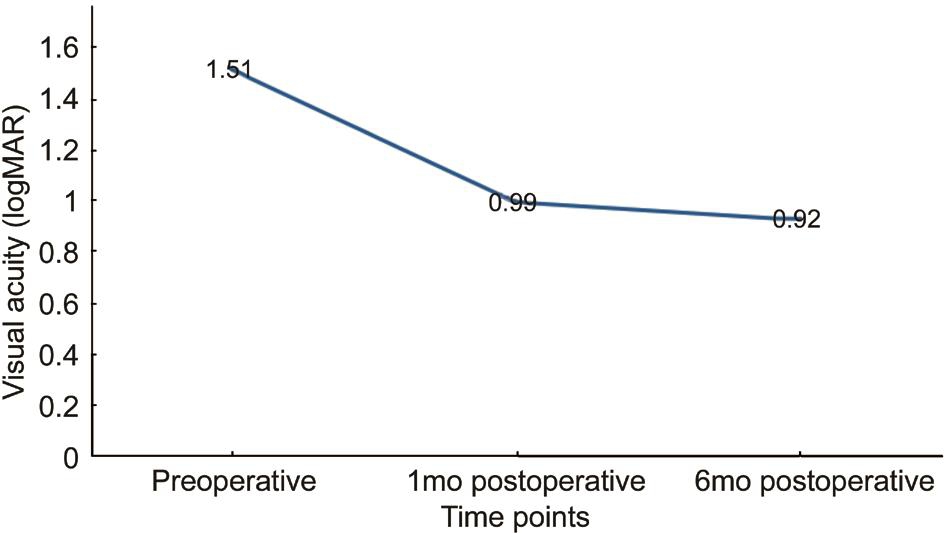
Complete closure (defined as no neurosensory defect at the fovea on OCT) was observed in 21 eyes three days after surgery. The complete closure was observed in 31 eyes three days to seven days after surgery. The complete closure of MH was ultimately bringed about in 31 patients examinated by OCT imaging (93.94%) by 1wk postoperative. Visual acuity improved from 1.51±0.31 logMAR (range: 20/2000-20/200; median Snellen acuity: 20/500) preoperatively to 0.99±0.32 logMAR (range: 20/1000-20/50; median Snellen acuity: 20/160) 1mo after surgery (P=0.000), and to 0.92±0.30 logMAR (range: 20/500-20/40; median Snellen acuity: 20/160) 6mo after surgery (P=0.000). There was no significant difference in visual acuity between 1mo after surgery and 6mo after surgery (P=0.544; Figure 2).
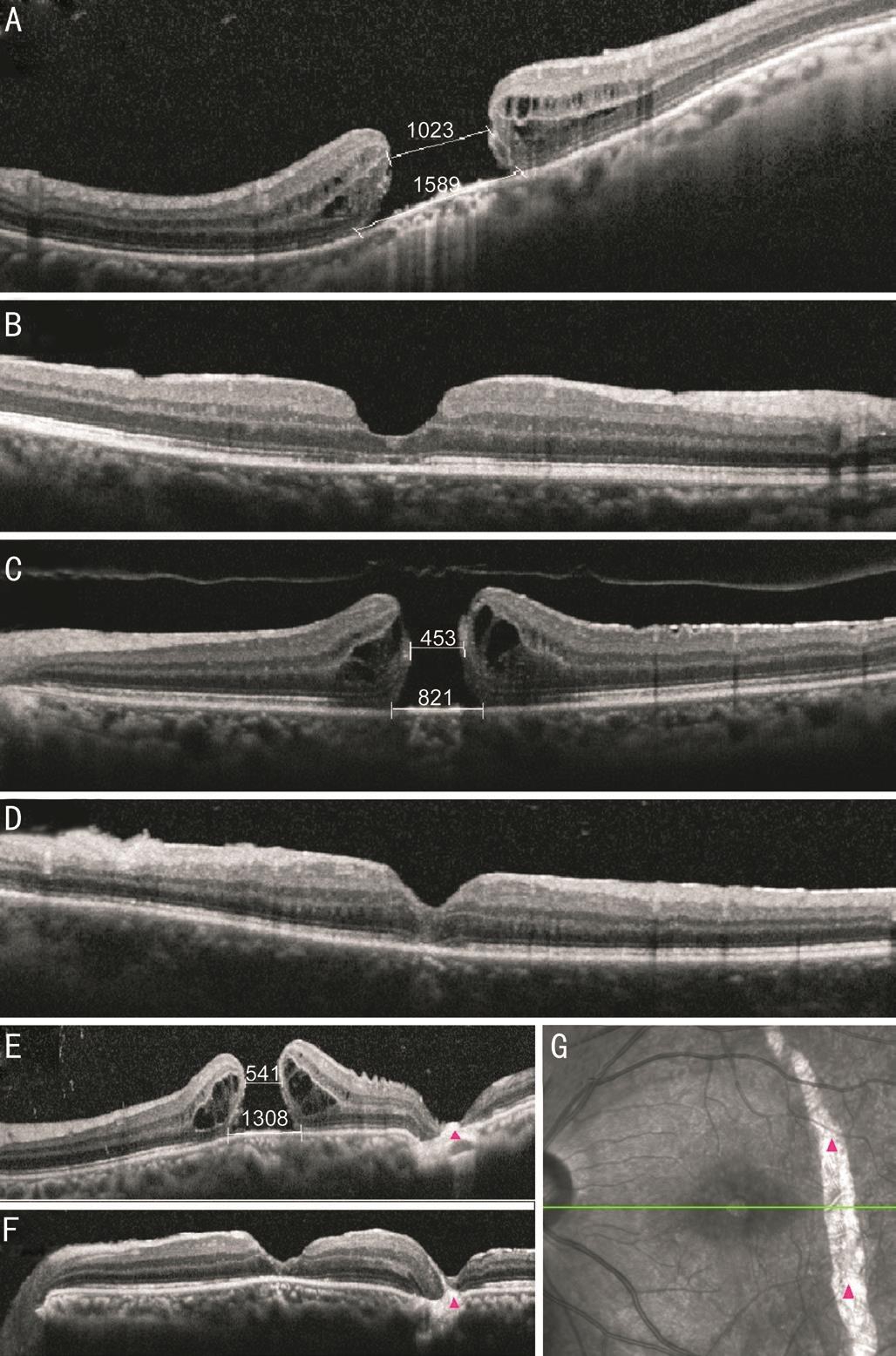
In our study, there were two closure types of MHs such as U-type (Figure 3B) and V-type (Figure 3D, 3F) in nineteen eyes and fourteen eyes, respectively. Linear configuration analogous to transplanted ILM tissues were detected in ten eyes determined by OCT 1mo after the surgery. There were no significant changes in OCT finding during the follow-up period from 1 to 6mo after surgery.
DISCUSSION
Kelly and Wendel[9] reported that the closure rate of MHs was 58% when ILM peeling assisted PPV was first introduced to manage idiopathic MH, and have improved to 86%-100%assisted by ILM staining technique[10]. Chuang et al[11] reported that the closure rate of MHs was 87% in patients with high myopia by vitrectomy and ILM peeling. However, the closure rate of MH and improvement of visual acuity were not as good as those in non-high myopia. Longer axial length may increase the risk of anatomic reduction failure[12]. Large MHs(minimum D >400 μm), however, appeared to be lower closuer rate than the idiopathic forms. In addition, about 19%-39% of the anatomically closed large MHs were actually fl at-open[13-15].
The traditional ILM peeling only release the tangential traction,but cannot compensate for tissue shortening in large MHs. The rate of closure for large idiopathic MHs had increased to 98%along the recent advent of the inverted ILM flap technique, and to 100% in a report for high myopic MHs[4,7]. Michalewska et al[4] hypothesized that the inverted ILM flap technique could improve MHs closure rates and enhance closure by stimulating glial cells proliferation. Müller cells play a key role in supporting the normal function of neurons and are the major glial cells in the retina[16]. The mechanisms for tissue repair in the MHs by inverted ILM flap technique were as follows:Müller cell fragments in the inverted ILM can proliferate along the inverted ILM flap and induce glial cell hyperplasia in the retina. The inverted ILM served as basement membrane and scaffolds for tissue proliferation, thus providing an environment to instruct the photoreceptors to assume correct position during the reconstruction process[4].
We also achieved successful closures of the large MH in our reports, and we did not see any excessive gliosis during the 6mo follow-up period, which displayed as high reflection area in OCT[17-18]. Although we did not see any excessive gliosis,long-term follow-up will be required to examine excessive gliosis in the retina. We speculate that the mechanisms for tissue repair in the MHs by the tiled transplantation ILM pedicle flap technique are the same as inverted ILM flap technique. It is hypothesized theoretically that the tiled transplantation ILM pedicle flap technique is more advantageous than inverted ILM flap technique, because the microenvironment of former is more similar to the normal physiological conditions, for example, the MHs directly contact the same surface of the ILM the same as normal physiological conditions. The ILM has two sides, one side facing the vitreous and the other side facing the nerve fiber layer of the retina. These two sides are very different. The side facing the vitreous (A side) is completely smooth, and the side facing the nerve fiber layer (B side) is obviously irregular, the reason for the irregularity is that the branching protrusion of the Müller cell is attached to the inner limiting membrane. Our tiled translocation ILM flap technique is obviously not the same as the previously reported various inverted ILM flap techniques.In our technique, the B side of ILM flap is still facing the nerve fiber layer, thus creating a condition that is closest to the normal anatomy for the growth of the MH, which is why the excellent anatomic results with visual improvement are obtained in these cases. However, in the previously reported of inverted ILM flap technique, the B side of ILM is oriented towards the vitreous, which is the significant difference between our technology and their technology. So we speculate that the tiled transplantation ILM pedicle flap technique provides an better environment to instruct the photoreceptors to assume correct position during the reconstruction process,theoretically better than the inverted ILM flap technique.Further comparative and prospective studies involving more patients will be needed to determine the actual efficacy of the technique.
This technique is also an easy-to-use technique that we break down its main process into two parts. The first step is to peel a circular area about 2 papilla disc in size along the edge of the MH, the starting position avoiding the edge of the hole and the vessel. The second step, then to make a pedicled ILM flap, and the width of flap should be larger than the MH diameter. The purpose of the first step is to relax the pull of the ILM on the
MH. The second step is to build a bridge for closing the MH.And the advantage of the pedicled ILM flap compared to the free ILM flap is that the former is not easily detached.
In our report, spontaneous detachment of the flap occurred in two of thirty-three eyes during the air- fluid exchange. The eye axis of the high myopia is significantly longer, and the ILM of high myopia is thinner than the normal eyes. We found that the ILM of high myopia is very tightly bound to the retina and is not easily separated, so it is difficult to get a large and strong enough flap. It may be that the above two reasons why the two high myopia patients had dislocation of the ILM flap during surgery. To address this same problem, Shin et al[19]used perfluoro-n-octane to assist the covering of the MH with a single sheet of ILM flap. In our cases, we did not use per fl uoro-n-octane. In our experience, we found that in order to prevent the detachment of the flap during surgery, should pay attention to the following aspects. Fifirst, try to peel off a larger ILM flap at the first time, otherwise the usable ILM will become less and less. we gently tiled the flap on the MH, try to make them stick to each other. Second, we found that lowering the perfusion pressure might help to avoid the flap from being washed away during air-fluid exchange. Third, if necessary,low molecular weight hyaluronic acid was used to keep the ILM pedicle flap stable and leave it in place at the end of the procedure.
Imai and Azumi[20] found an expansion of RPE atrophy happened 1wk after ICG staining, suggesting that ICG-stained ILM flaps may cause RPE injury. However, Hirano et al[21]reported that they observed that the preoperative chorioretinal atrophy did not enlarge up to 6mo postoperative. In our study,we have observed no dilatation of the chorioretinal atrophy up to 6mo postoperative. We need further observations to assess the safety of using ICG staining in the surgery. SF6, C3F8 and sterile air are the most commonly used gas fillers for MH surgery. Intraocular gases can isolate and seal to area of the hole; intraocular gases can produce mechanical tamponade and promote the healing of the hole due to the buoyancy of the gas[22]. Comparative studies reported that room air had the similar closure rate to SF6 and C3F8[23-25]. The advantage offilling sterile air is economical and convenient. The patient adhered to face-down for 7d after surgery. In our study, we found that there is also a high anatomic success rate using sterile air. We observed that the macular fovea after the closure of the MH was similar to the letter U, some resembling the letter V. No change in morphology after 6mo of observation.We have not found any difference in prognosis between the two types until now, which require longer observation and further research.
In conclusion, our clinical outcomes suggest that the tiled transplantation ILM pedicle flap technique was beneficial for the treatment of large MHs, including idiopathic, high myopia and traumatic MHs. Using the tiled transplantation ILM pedicle flap technique provides another option for patients with large MHs.
ACKNOWLEDGEMENTS
Thanks to Zheng-Rong Lian and Cai-Hong Sun for their assistance of thesis methodology.
Foundation: Supported by the Shaanxi Provincial Social Development Scientific and Technological Project(No.2016SF-133).
Conflicts of Interest: Wang LP, None; Sun WT, None; Lei CL,None; Deng J, None.
REFERENCES
1 Aaberg TM, Blair CJ, Gass JD. Macular holes. Am J Ophthalmol 1970;69(4):555-562.
2 Liu PK, Chang YC, Wu WC. Management of refractory macular hole with blood and gas-assisted autologous neurosensory retinal free flap transplantation: a case report. BMC Ophthalmol 2018;18(1):230.
3 Peng J, Chen C, Jin H, Zhang H, Zhao P. Autologous lens capsular flap transplantation combined with autologous blood application in the management of refractory macular hole. Retina 2018;38(11):2177-2183.
4 Michalewska Z, Michalewski J, Adelman RA, Nawrocki J. Inverted internal limiting membrane flap technique for large macular holes.Ophthalmology 2010;117(10):2018-2025.
5 Mahalingam P, Sambhav K. Surgical outcomes of inverted internal limiting membrane flap technique for large macular hole. Indian J Ophthalmol 2013;61(10):601-603.
6 Kuriyama S, Hayashi H, Jingami Y, Kuramoto N, Akita J, Matsumoto M. Efficacy of inverted internal limiting membrane flap technique for the treatment of macular hole in high myopia. Am J Ophthalmol 2013;156(1):125-131.e1.
7 Michalewska Z, Michalewski J, Dulczewska-Cichecka K, Nawrocki J.Inverted internal limiting membrane flap technique for surgical repair of myopic macular holes. Retina 2014;34(4):664-669.
8 Shah SP, Manjunath V, Rogers AH, Baumal CR, Reichel E, Duker JS.Optical coherence tomography-guided facedown positioning for macular hole surgery. Retina 2013;33(2):356-362.
9 Kelly NE, Wendel RT. Vitreous surgery for idiopathic macular holes.Arch Ophthalmol 1991;109(5):654-659.
10 Shukla D, Kalliath J, Neelakantan N, Naresh KB, Ramasamy K. A comparison of brilliant blue G, trypan blue, and indocyanine green dyes to assist internal limiting membrane peeling during macular hole surgery.Retina 2011;31(10):2021-2025.
11 Chuang LH, Chen YP, Wang NK, Yeung L, Chen KJ, Hwang YS, Wu WC,Chen TL, Lai CC. Macular hole repair by vitrectomy and internal limiting membrane peeling in highly myopic eyes. Retina 2014;34(10):2021-2027.
12 Huisingh C, McGwin G Jr. Re: Conart et al: Outcomes of macular hole surgery with short-duration positioning in highly myopic eyes: a casecontrol study (Ophthalmology 2014;121:1263-1268). Ophthalmology 2015;122(9):e55-e56.
13 Imai M, Iijima H, Gotoh T, Tsukahara S. Optical coherence tomography of successfully repaired idiopathic macular holes. Am J Ophthalmol 1999;128(5):621-627.
14 Kang SW, Ahn K, Ham DI. Types of macular hole closure and their clinical implications. Br J Ophthalmol 2003;87(8):1015-1019.
15 Michalewska Z, Michalewski J, Cisiecki S, Adelman R, Nawrocki J. Correlation between foveal structure and visual outcome following macular hole surgery: a spectral optical coherence tomography study.Graefes Arch Clin Exp Ophthalmol 2008;246(6):823-830.
16 Bringmann A, Pannicke T, Grosche J, Francke M, Wiedemann P,Skatchkov SN, Osborne NN, Reichenbach A. Müller cells in the healthy and diseased retina. Prog Retin Eye Res 2006;25(4):397-424.
17 Daniel E, Toth CA, Grunwald JE, Jaffe GJ, Martin DF, Fine SL,Huang JY, Ying GS, Hagstrom SA, Winter K, Maguire MG. Risk of scar in the comparison of age-related macular degeneration treatments trials.Ophthalmology 2014;121(3):656-666.
18 Goldenberg D, Goldstein M, Loewenstein A, Habot-Wilner Z. Vitreal,retinal, and choroidal findings in active and scarred toxoplasmosis lesions:a prospective study by spectral-domain optical coherence tomography.Graefes Arch Clin Exp Ophthalmol 2013;251(8):2037-2045.
19 Shin MK, Park KH, Park SW, Byon IS, Lee JE. Per fluoro-N-octaneassisted single-layered inverted internal limiting membrane flap technique for macular hole surgery. Retina 2014;34(9):1905-1910.
20 Imai H, Azumi A. The expansion of RPE atrophy after the inverted ILM flap technique for a chronic large macular hole. Case Rep Ophthalmol 2014;5(1):83-86.
21 Hirano M, Morizane Y, Kawata T, Kimura S, Hosokawa M, Shiode Y, Doi S, Hosogi M, Fujiwara A, Shiraga F. Case report: successful closure of a large macular hole secondary to uveitis using the inverted internal limiting membrane flap technique. BMC Ophthalmol 2015;15:83.
22 Casini G, Loiudice P, De Cillà S, Radice P, Nardi M. Sulfur hexa fl uoride(SF6) versus perfluoropropane (C3F8) tamponade and short term facedown position for macular hole repair: a randomized prospective study.Int J Retina Vitreous 2016;2:10.
23 Hasegawa Y, Hata Y, Mochizuki Y, Arita R, Kawahara S, Kita T,Noda Y, Ishibashi T. Equivalent tamponade by room air as compared with SF6 after macular hole surgery. Graefes Arch Clin Exp Ophthalmol 2009;247(11):1455-1459.
24 Kim SS, Smiddy WE, Feuer WJ, Shi W. Outcomes of sulfur hexafluoride (SF6) versus perfluoropropane (C3F8) gas tamponade for macular hole surgery. Retina 2008;28(10):1408-1415.
25 Briand S, Chalifoux E, Tourville E, Bourgault S, Caissie M, Tardif Y,Giasson M, Boivin J, Blanchette C, Cinq-Mars B. Prospective randomized trial: outcomes of SF6 versus C3F8 in macular hole surgery. Can J Ophthalmol 2015;50(2):95-100.
Co- first authors: Li-Ping Wang and Wen-Tao Sun.
Correspondence to:Wen-Tao Sun. Department of Ophthalmology,Shaanxi Ophthalmic Medical Center, Xi'an Fourth Hospital,Affiliated Guangren Hospital, School of Medicine, Xi'an Jiaotong University, Xi'an 710004, Shaanxi Province, China.245135237@qq.com
Received: 2018-10-08 Accepted: 2018-12-10
● KEYWORDS: tiled transplantation ILM pedicle flap; macular hole; vitrectomy
DOl:10.18240/ijo.2019.02.10
Citation: Wang LP, Sun WT, Lei CL, Deng J. Clinical outcomes with large macular holes using the tiled transplantation internal limiting membrane pedicle flap technique. Int J Ophthalmol 2019;12(2):246-251