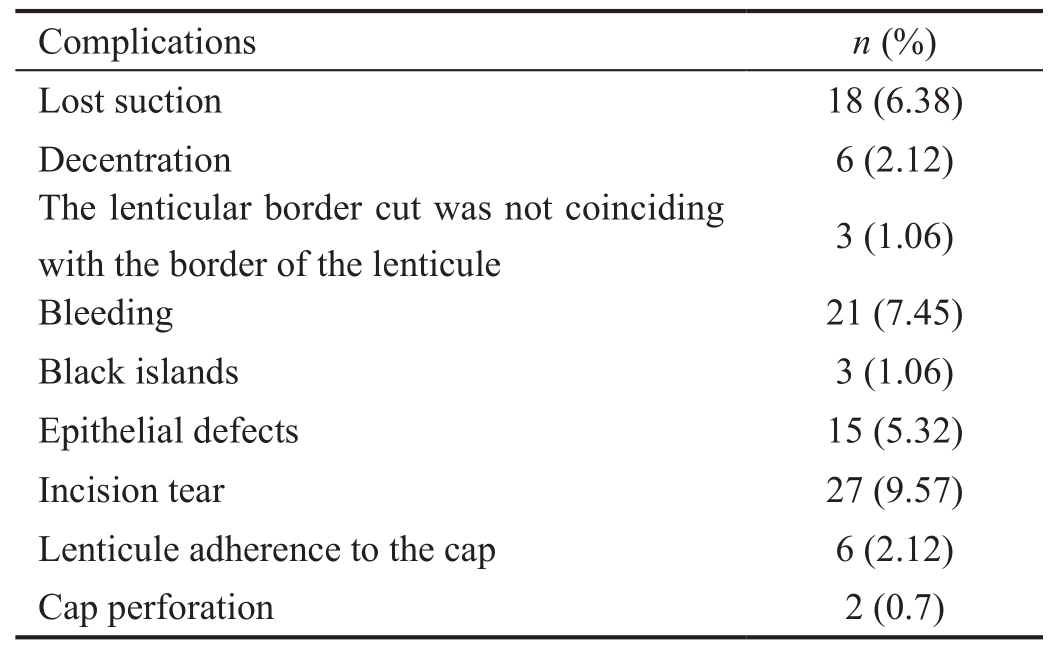
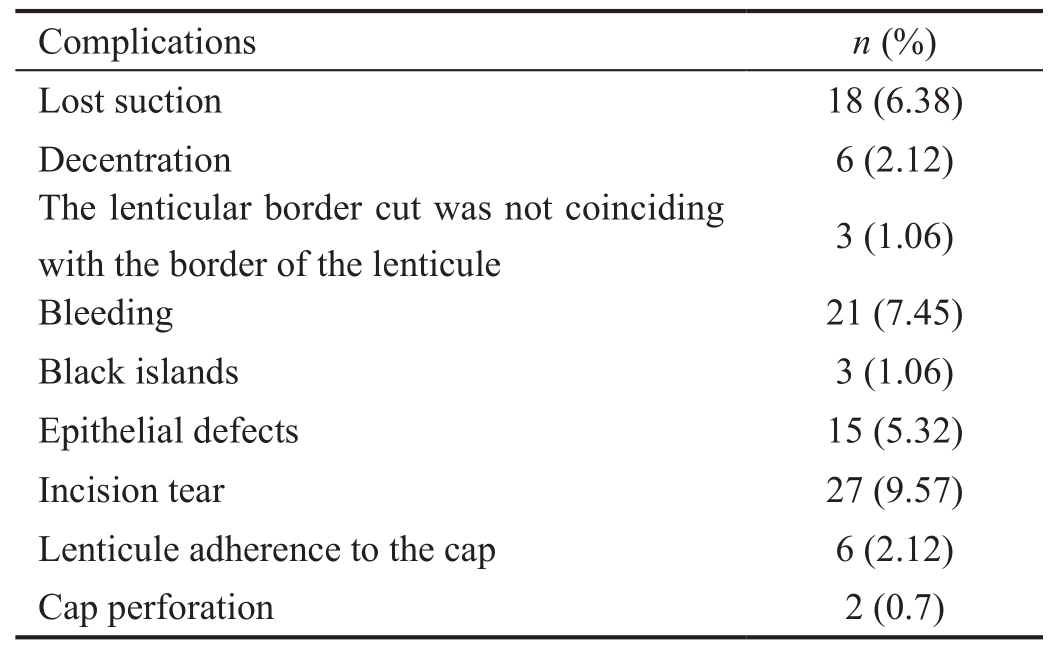
Table 1 Incidence of intraoperative SMILE complications
?
F emtosecond laser technique has been used recently to create laser-assisted in situ keratomileusis (LASIK)corneal flaps with high predictability, safety, and accuracy[1-2].Refractive lenticule extraction (ReLEx) is a single laser refractive procedure without the use of an excimer laser[3-4].Small incision lenticule extraction (SMILE) is a variation of ReLEx without retractable flap and accurate ablation[4].
SMILE procedure is to create a lenticule of corneal stroma using femtosecond laser, which is then extracted through a 3 mm incision. SMILE avoids all the flap complications that may occur with LASIK including: free caps, incomplete,irregular or thin flaps and buttonholes. SMILE is a technique of removing rather than ablating tissue. The main advantages of SMILE are to preserve the strong anterior corneal lamellae with a better long-term biochemical stability as well as less postoperative dry eye due to preservation of corneal nerve endings, and thus faster and more comfortable visual recovery[4-9]. SMILE is a safe, efficacious and predictable method of refractive correction[10-12] with a good centration of treatment than LASIK[13].
The aim of this study is to report the incidence of SMILE intraoperative complications and their management.
Ethical Approval Ebsar EYE CENTER Review Board (IRB)/Ethics Committee approval was obtained. This study adhered to the tenets of the Declaration of Helsinki. The nature of the procedure was explained, and preoperative written informed consent was obtained from the patients.
This is a retrospective consecutive interventional clinical study.This study conducted on patients with myopia and myopic astigmatism, who underwent SMILE procedure. The procedure was done at Ebsar Eye Centre in the period from September 2015 to November 2016.
Patients with stable refractive error for at least 1-year, stable tear film, discontinuation of contact lens for at least 1wk prior to surgery and central corneal thickness >500 μm were included in this study.
Cases with central corneal thickness <500 μm, keratoconus,central corneal opacities, ocular surface disease and sever dry eye were excluded.
All patients underwent unaided and best-corrected visual acuity (BCVA), manifest and cycloplegic refraction,applanation tonometry, slit lamp examination, dilated fundus examination using indirect ophthalmoscope and +90d with slit lamp biomicroscopy and Shceimp flug corneal tomography(OCULUS Pentacam®, OCULUS Inc., Germany).
All the surgeries were performed by one surgeon (Hamed AM), for both eyes in one setting, except one patient who underwent monocular surgery.
Surgical Procedure Topical anesthesia using benoxinate hydrochloride 0.4% eye drops was applied. The eye was sterilized. Centration was achieved by asking the patient to look at the fixation flashing green light of the VisuMax FS laser system (Carl Zeiss Meditec, Jena, Germany). Docking of the eye with the curved interface cone and suction fixation were applied. The following femtosecond laser parameters were used: 140 μm cap thickness, 7.5 mm anterior-plane cut diameter, 6.5 mm optical zone of lenticule, 160 nJ of energy with lenticule side-cut angles at 135°. A 3.0 mm entrance wound was created centered between 9 and 12 o'clock in all cases. The spot distance and tracking spacing are 4.5/4.5 μm for the posterior lenticule plane, 2.5/2.5 μm for the lenticule side-cut, 4.5/4.5 μm for the anterior lenticule plane and 2.5/2.5 μm for the entrance wound side-cut.
The femtosecond laser created in a spiral-in fashion the deep surface of the lenticule, the lenticule border, the superficial surface in a spiral-out fashion and the small incision in that order. Suction is then released, and the eye is undocked.
The Duckworth & Kent SMILE Double Ended Dissector with Spoon Tip was inserted into the pocket through the incision.Dissection of the superficial surface of the lenticule was done.Then it was guided below the deep surface to dissect of the deep surface of the lenticule and then used to fold the lenticule to one side. The lenticule was extracted through the incision using SMILE lenticular removal forceps (Duckworth and Kent, Product Number: 2-836).
Postoperative Care Antibiotic eye drops (moxi fl oxacin 0.5%)and topical steroids eye drops (dexamethazone 0.1%) were given 5 times daily for 2wk with withdrawal of corticosteroid eye drops over another 2wk. Artificial eye drops were given for 3mo. Follow-up of the patient postoperatively was scheduled for 1d and 1wk and subsequently at 3 and 6mo postoperatively.
Two hundred and eighty-two eyes of 141 patients were reviewed in this retrospective interventional consecutive study.All the patients underwent SMILE procedure to correct myopia or myopic astigmatism or both.
The intraoperative complications were reported. The 101 eyes of 52 patients had intraoperative complications(Table 1). The mean operative duration of the SMILE surgery was 13.76±3.71min.
Table 1 Incidence of intraoperative SMILE complications
?
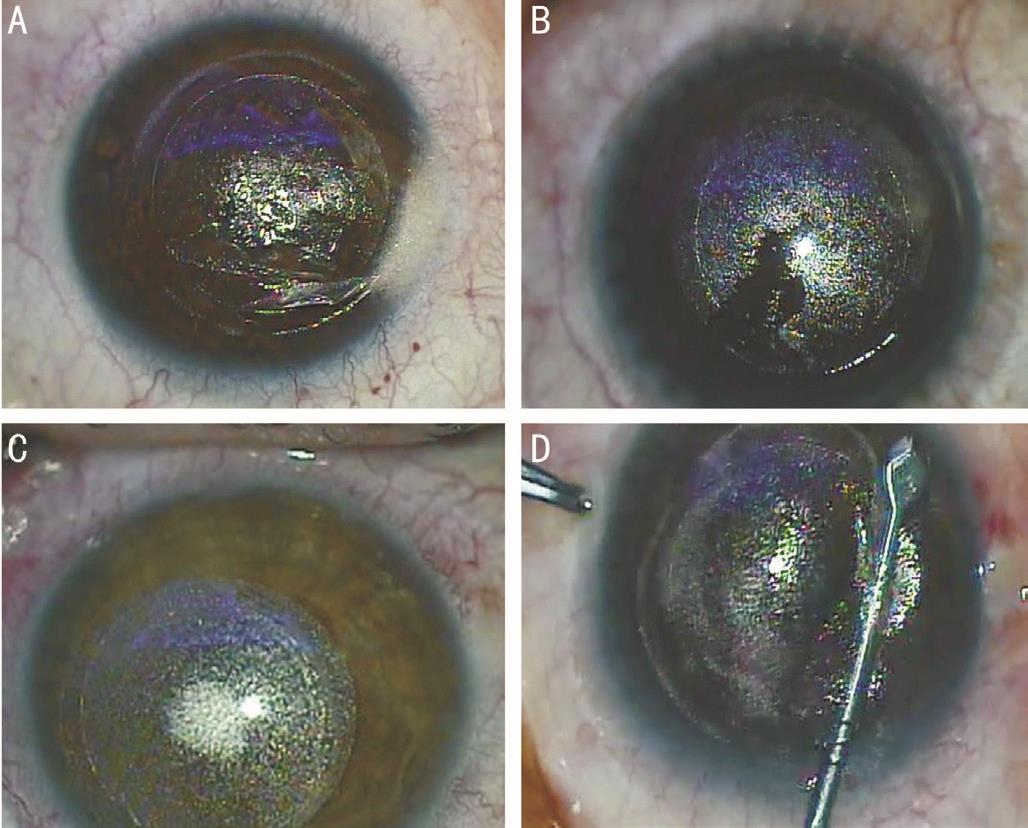
Figure 1 Reported intraoperative complications
A: Incision tear during lenticular extraction; B: Black islands during SMILE operation; C: Treatment decentration; D: Cap perforation.
Eighteen eyes (6.38%) had lost suction. If lost suction occurred before the total creation of the lenticule, the procedure was aborted and rescheduled after the reabsorption of the cavitation bubbles. If the lost suction occurred after the total creation of the lenticule or during the creation of the cap, the eye could be re-docked with a repair license if it was available and the surgeon could restart the cap, side cut and wound creation and dissected it normally.
Incision tear during lenticular extraction was reported in 27 eyes (9.57%) (Figure 1A). We instructed the patients to fixate on the microscope light. If the patients unable to fixate; we used the gimble fixation instrument to decrease eye movements. Twenty-one eyes (7.45%) had intraoperative wound bleeding (due to a vascular pannus).
Black islands (incomplete bubble separation) that reached the pupil was found in 3 eyes (1.06%) which happened due to meibomian secretions that were adherent to the surface of the cone (Figure 1B), the operations were aborted.
Lenticule adherence to the cap was reported in 6 eyes (2.12%).A SMILE lenticule hook (Duckworth & Kent®, England, UK)was used to peel the lenticule out of the pocket.
The epithelial defects occurred in 15 eyes (5.32%). Postoperative contact lens for 1 day was applied.
Treatment decentration was reported in 6 eyes (2.12%), the operations were aborted (Figure 1C). Cap perforation occurred in 2 eyes (0.7%) (Figure 1D).
The lenticular border side cut was not coinciding with the border of the lenticule in 3 eyes (1.06%), the operation was aborted. No eye had lenticule rupture. No significant postoperative complications in these cases were detected.
Femtosecond lasers have advantages over mechanical microkeratomes for creating LASIK flaps. The introduction of a femtosecond laser as a microkeratome is not without disadvantages[13-14]. SMILE is the latest development in a long evolution of keratorefractive procedures[15].
In this study, we reported the intraoperative complications of cases with myopia or myopic astigmatism that underwent refractive correction by SMILE procedure.
We reviewed 282 eyes of 141 patients from our medical records in the period from September 2015 to November 2016.One hundred one eyes of 52 patients had intraoperative complications. The mean operative duration of the SMILE surgery was 13.76±3.71min.
We reported 18 eyes (6.38%) with lost suction. If lost suction occurred before the total creation of the lenticule, the procedure was aborted and rescheduled after the reabsorption of the cavitation bubbles. If the lost suction occurred after the total creation of the lenticule or during the creation of the cap, the eye could be re-docked with a repair license if it was available and the surgeon could restart the cap, side cut and wound creation and dissected it normally. The causes of suction loss are not well known, the suction loss occurs more likely if the patient attempted to move his eye while the suction is active,or it may occur if there is a tiny opening that allows passage of fluid between the patient eye and the cone.
To overcome this complication, we switched from the standard mode of femtosecond laser treatment to the fast mode. We think that it takes shorter time with less incidence of suction loss during the surgery. Also, we decided to use the small size cone on all SMILE cases regardless the white-to-white measurement. As well known, the cone suction applies on the cornea only, and this fact makes the bigger size cone apply suction very close to the limbus that makes the suction loss becomes much easier. Reducing the time of laser procedure from 35s to 25s might lead to reduce the suction time with less incidence of suction loss[16].
Ivarsen et al[17] reported 14 eyes (0.8%) with suction loss. The 13 eyes were retreated successfully immediately, 2wk or 2mo later. One eye retreated with difficult lenticular extraction led to post-operative irregular astigmatism.
Sharma and Vaddavalli[18] reported a case of suction loss in uncooperative patient during cap cut. They tried to re-dock but suction loss occurred again. The procedure was abandoned and converted to femto-LASIK flap. Wong et al[19] reported 11 cases with suction loss during ReLEX procedure. Nine cases were retreated with good suction at the same session while the other 2 cases were aborted.
Small palpebral aperture, loose corneal epithelium, excessive reflex tearing, poor fixation patient anxiety and inability to follow instructions are predisposing factors of suction loss[19-20].
Minor incision tear occurred in 27 eyes (9.57%). The causes of incision tear are either; the patient moves his eye suddenly in any direction while the surgeon is using some instrument inside the SMILE pocket, or due to the surgeon is still in his early learning curve, so he accidentally pushes on SMILE cap causing wound tear. In order to prevent this complication, we fixated the eye with Gimble fixation instrument to prevent inadvertent eye movement. Puch up technique is a new technique that may help to identify the edge of the lenticule.The authors suggested using Y-shaped instrument to identify the edge of the lenticule[21]. Ivarsen et al[17] reported 33 eyes with minor tears at the incision wound and 1 eye with major tear that lead to radial tear dividing the cap in two.
Black islands reaching the visual axis were reported in 3 eyes (1.06%). The operations were aborted. The presence of meibomian gland secretions or debris, while the ocular surface was coupled with the femtosecond laser docking cone, could block the femtosecond laser. The area with no treatment was left either in the lenticule cap interface or in the lenticule stroma interface. The areas with black islands will thus need rougher dissection that may lead to postoperative corneal opacity and irregular astigmatism. Qiu and Yang[20]recommended that if the black spots could influence lenticule separation, measures should be promptly adopted to produce the active suction loss and the surgery should be discontinued immediately.
Treatment decentration was reported in 6 eyes. This complication always happens due to surgeon inexperience and his inability to do proper centration in the middle of the pupil.
Cap perforation was another infrequent complication (2 eyes,0.7%) while dissecting inside the pocket. If the maneuver was rough due to presence of black islands between the femtosecond laser bubbles, the small incision could be enlarged in an uncontrolled manner with sudden resistance release leading to perforation.
Previous study reported 4 cases of cap perforation that not affected the postoperative visual outcome[17]. Lenticule adherence to the cap was reported in 6 eyes (2.12%). We completed the operation successfully without any further complications. This complication always happens when the surgeon is unable to recognize the edge of the lenticule and he dissect all the way underneath, so the lenticule will be adherent to the cap. Ivarsen et al[17] reported impossible lenticular extraction in one patient, the procedure was aborted.They suggested aborting the procedure early in cases with difficult lenticule dissection and reconsidering the patient for an excimer-based treatment.
Insignificant intraoperative epithelial defects occurred in 15 eyes (5.32%). Postoperative contact lens for 1 day was applied.Bleeding from the wound occurred (due to vascular pannus) in 21 eyes (7.45%).
We think that the inexperience of the surgeon at the beginning of learning curve and inability to detect the edge of the lenticule with numerous attempts of dissection above or below the lenticule to find it is the major cause of most of intraoperative complications.
Although SMILE is a new technique for the correction of myopia and myopic astigmatism with efficient, predictable and safe refractive and visual outcomes, complications can occur. However, most of these complications are related to inexperience and are included in the learning curve of the technique. More studies with a bigger number of eyes are required to efficiently evaluate the intraoperative complications and standardize their management strategies.
Conflicts of Interest:Hamed AM, None; Heikal MA, None;Soliman TT, None; Daifalla A, None; Said-Ahmed KE, None.
1 Kymionis GD, Kankariya VP, Plaka AD, Reinstein DZ. Femtosecond laser technology in corneal refractive surgery: a review. J Refract Surg 2012;28(12):912-920.
2 Tanna MS, Schallhorn SC, Hettinger KA. Femtosecond laser versus mechanical microkeratome: a retrospective comparison of visual outcomes at 3mo. J Refract Surg 2009;25(7 Suppl):S668-S671.
3 Sekundo W, Kunert K, Russmann C, Gille A, Bissmann W, Stobrawa G, Sticker M, Bischoff M, Blum M. Fifirst efficacy and safety study of femtosecond lenticule extraction for the correction of myopia: six-month results. J Cataract Refract Surg 2008;34(9):1513-1520.
4 Shah R, Shah S, Sengupta S. Results of small incision lenticule extraction: all-in-one femtosecond laser refractive surgery. J Cataract Refract Surg 2011;37(1):127-137.
5 Wang Y, Wu ZQ, Tang X, Zhang JM, Dou R, Geng WL, Jin Y, Zuo T. Two millimeter micro incision lenticule extraction surgery with minimal invasion: a preliminary clinical report. Zhonghua Yan Ke Za Zhi 2014;50(9):671-680.
6 Liu ML, Chen YL, Wang DY, Zhou YG, Zhang XY, He JX, Zhang T,Sun Y, Liu Q. Clinical outcomes after SMILE and femtosecond laserassisted LASIK for myopia and myopic astigmatism: a prospective randomized comparative study. Cornea 2016;35(2):210-216.
7 Kamiya K, Shimizu K, Igarashi A, Kobashi H. Visual and refractive outcomes of femtosecond lenticule extraction and small-incision lenticule extraction for myopia. Am J Ophthalmol 2014;157(1):128-134.e2.
8 Vestergaard A, Ivarsen AR, Asp S, Hjortdal JØ. Small-incision lenticule extraction for moderate to high myopia: predictability, safety, and patient satisfaction. J Cataract Refract Surg 2012;38(11):2003-2010.
9 Denoyer A, Landman E, Trinh L, Faure JF, Auclin F, Baudouin C.Dry eye disease after refractive surgery: comparative outcomes of small incision lenticule extraction versus LASIK. Ophthalmology 2015;122(4):669-676.
10 Kobashi H, Kamiya K, Shimizu K. Dry eye after small incision lenticule extraction and femtosecond laser-assisted LASIK: meta-analysis.Cornea 2017;36(1):85-91.
11 Sekundo W, Kunert KS, Blum M. Small incision corneal refractive surgery using the small incision lenticule extraction (SMILE) procedure for the correction of myopia and myopic astigmatism: results of a 6 month prospective study. Br J Ophthalmol 2011;95(3):335-339.
12 Moshirfar M, McCaughey MV, Reinstein DZ, Shah R, Santiago-Caban L, Fenzl CR. Small-incision lenticule extraction. J Cataract Refract Surg 2015;41(3):652-665.
13 Yu Y, Zhang W, Cheng X, Cai J, Chen H. Impact of treatment decentration on higher-order aberrations after SMILE. J Ophthalmol 2017;2017:9575723.
14 Durrie DS, Kezirian GM. Femtosecond laser versus mechanical keratome flaps in wavefront-guided laser in situ keratomileusis:prospective contralateral eye study. J Cataract Refract Surg 2005;31(1):120-126.
15 Kezirian GM, Stonecipher KG. Comparison of the IntraLase femtosecond laser and mechanical keratomes for laser in situ keratomileusis. J Cataract Refract Surg 2004;30(4):804-811.
16 Ang M, Chaurasia SS, Angunawela RI, Poh R, Riau A, Tan D, Mehta JS. Femtosecond lenticule extraction (FLEx): clinical results, interface evaluation, and intraocular pressure variation. Invest Ophthalmol Vis Sci 2012;53(3):1414-1421.
17 Ivarsen A, Asp S, Hjortdal J. Safety and complications of more than 1500 small-incision lenticule extraction procedures. Ophthalmology 2014;121(4):822-828.
18 Sharma R, Vaddavalli PK. Implications and management of suction loss during refractive lenticule extraction (ReLEx). J Refract Surg 2013;29(7):502-503.
19 Wong CW, Chan C, Tan D, Mehta JS. Incidence and management of suction loss in refractive lenticule extraction. J Cataract Refract Surg 2014;40(12):2002-2010.
20 Qiu PJ, Yang YB. Analysis and management of intraoperative complications during small-incision lenticule extraction. Int J Ophthalmol 2016;9(11):1697-1700.
21 Hamed A, Fekry A. Refractive small-incision lenticule extraction:Push-up and push-down techniques. J Cataract Refract Surg 2016;42(12):1713-1715.