
Figure 1 Artiflex/Veriflex phakic intraocular lens (Simões and Ferreira[6], 2014).
P hakic intraocular lens implantation is an approach used to correct myopia especially high myopia which can not be corrected with laser corneal refractive surgery[1].
These lenses are classified according to their site of implantation into three types: anterior chamber angle-supported, iris-fixated phakic intraocular lens, and posterior chamber. Although there are many designs of angle-supported phakic intraocular lenses, most have been withdrawn from the market due to complications related to corneal endothelial cell loss[2]. On the other hand iris-fixated phakic intraocular lenses and implantable collamer lenses (ICLs) are approved by Food and Drug Administration and have conformity with European status[3].
Artiflex lens is an example for foldable iris fixed anterior chamber phakic intraocular lenses which can be implanted through a 3.2 mm corneal incision. It has a big advantage of being “one sizefits all eyes”[4]. It is made of a silicone optic which is 6 mm in diameter and polymethylmethacrylate haptic.For safe implantation of Artiflex phakic intraocular lenses, the anterior chamber depth should be at least larger than 3.0 mm[5](Figure 1).

Figure 1 Artiflex/Veriflex phakic intraocular lens (Simões and Ferreira[6], 2014).
Visian V4c ICL with centraFLOW (ICL V4c) is a posterior chamber sulcus fixed phakic intraocular lens which was made of a biocompatible material called collamer, the design of this model characterized by central hole measured 360 μm in the optic of the lens, this central port allows a more natural fl ow of aqueous humor and eliminates the need for peripheral iridectomy leading to shortening of the time of surgery[4] with preservation of stable intraocular pressure[7]. In addition, this model handles vaulting issues as it provides a high vault which prevent contact between the ICLs and crystalline lens and allows aqueous flow with delivery of nutrients to crystalline lens leading to decrease risk of cataract formation[7]. The fourth generation received approval in December 2005[8] (Figure 2).Multiple studies from different parts of the world compared the visual outcomes of the old model of ICL (V4) to the unfoldable model of iris fixed phakic intraocular lens (Artisan/Verisyse)but there is no available studies that compare the visual outcomes including contrast sensitivity of the new model of ICL (V4c) which contain central pore and the foldable model of iris fixed phakic intraocular lens (Artiflex/Veriflex), the importance of focusing on contrast sensitivity testing is that contrast sensitivity represents indicator for a level of visual functionality or quality, that can be impaired in presence of a normal visual acuity, also its loss is more prominent and disturbing than loss of visual acuity[10-13].
In this study, we used prospective design to assess visual performance and compare the qualitative and quantitative visual outcomes of two types of foldable intraocular lenses [Visian ICL(V4c) and Artiflex] that are used for correction of high myopia.
Ethical Approval The study protocol was approved by the Committee of Institution Review Board and Medical Research Ethics Committee, Faculty of Medicine, Mansoura University(ms/1003) and followed the principles outlined in the Declaration of Helsinki. Written consent was obtained from every patient and they were informed about risks of surgery and consequences of the study.
Figure 2 ICL V4c CentraFLOW technology (Pineda and Chauhan[9], 2016).
Patient Enrollment This is a comparative prospective case study on patients with high myopia attended outpatients clinic of Mansoura Ophthalmic Center, Mansoura University in the period from January 2014 to January 2016. The inclusion criteria where high myopia (higher than 6 D), stable refractive error (<0.5 D change over one year), normal central corneal thickness with no history of ocular pathology or surgery. The exclusion criteria were patient age younger than 20y to ensure stable refraction, abnormal cornea such as keratoconus or corneal epithelial pathology, ocular surface disease, abnormal or large mesopic pupil, history of ocular inflammation,cataract, glaucoma, posterior segment pathology such as macular degeneration and retinopathy.
Selection of the type of phakic intraocular lens for patients was based on surgeon's preferences, there was no specific selection criteria.
Study Protocol Power calculation of the phakic intraocular lenses was provided by the manufacturer after giving them the following biometric data: refractive power, axial length,anterior chamber depth, keratometry, and white to white diameter.
Preoperatively Every patient had a complete ophthalmic examination which included uncorrected distant visual acuity (UDVA) and corrected distant visual acuity (CDVA),manifest and cycloplegic refractions using Nidek AR-800 autorefractometer, slit lamp biomicroscopic examination,endothelial cell count using non-contact specular microscopy(Tomey EM 3000), anterior segment analysis using Oculus scheimpflug pentacam, tonometry using Reichert Tonopen,axial length, anterior chamber depth and white to white measurement using Carl Zeiss intraocular lens Master V. 7.5,fundus examination using binocular Indirect ophthalmoscopy and examination of contrast sensitivity with a sine-wave grating at spatial frequencies of 1.5, 3, 6, 12 and 18 cpd using a computer software (chart 2020, Konan medical), the chart viewed from 3 m under photopic condition with mean luminance of 85 cd/m2. Sensitivity values were transformed into a logarithmic scale.
The study sample were classified into two groups: ICLV4c group (underwent Visian ICL V4c implantation); Artiflex group (underwent Artiflex lens implantation).
Surgical Techniques
Visian ICL V4c implantation operative technique The pupil was dilated using mydriatic eye drops, the operation was done under general anesthesia due to young age of patients and in some patients both eyes were operated at same session, the eye was sterilized with Betadine, two side ports was created using 19 gauge micro-vitreoretinal blade (MVR), viscoelastic(hydroxypropylmethylcellulose) was injected tofill the anterior chamber, 3.2 mm corneal incision was created by keratome.The ICL (V4c) was injected into the anterior chamber parallel to the iris plane and allowed to unfold, then the footplate at each corner of phakic intraocular lens was positioned gently under the iris. viscoelastic was removed and the corneal incisions were hydrated. Vigamox (moxi fl oxacinhydrochloride ophthalmic solution 0.5%, Alcon Laboratories Inc.)was subsequently instilled in the eye.
Artiflex lens implantation operative technique The pupil was constricted using miotic eye drops (pilocarpine hydrochloride ophthalmic solution 1%, Alcon Laboratories,Inc.). Operation was done under general anesthesia due to young age of patients and in some patients both eyes were operated at same session. The eye was sterilized with Betadine.Two side port incisions were done vertically at 2 and 10 o'clock positions aiming the sites of enclavation at 3 and 9 o'clock then a corneal tunnel incision was created by 3.2 mm keratome. Viscoelastic (hydroxypropyl methylcellulose) was injected inside anterior chamber then the Artiflex lens was implanted into the anterior chamber using a special holder which allows folding of the lens while passing through the main tunnel. Viscoelastic was re-injected between the corneal endothelium and the lens pushing it towards the iris then the lens was rotated to be placed in its proper position between 3 and 9 o'clock a little bit above the horizontal meridian using a manipulator. Enclavation was done using an enclavation needle and special forceps which holds the lens from the solid part.Peripheral iridectomy was performed using vitrectomy probe.Viscoelastic material was removed then the anterior chamber was filled with balanced saline solution. Stromal hydration of the main and side port incisions was performed. Vigamox(moxi fl oxacinhydro-chloride ophthalmic solution 0.5%, Alcon Laboratories Inc.) was subsequently instilled in the eye.
Postoperatively Examination visits were scheduled at 1d,1wk and 1, 3, 6 and 12mo using the same preoperative clinical parameters and investigation tools.
Assessment of outcome measures was based on a comparison of preoperative and postoperative visual acuity values to calculate safety index and efficacy index of each type of phackic intraocular lens as follow: safety index=mean postoperative CDVA/mean preoperative (CDVA) “using decimals for visual acuity”, efficacy index=mean postoperative UDVA/mean preoperative (CDVA) “using decimals for visual acuity”. Outcomes assessment also included comparison of the achieved versus the expected refractive outcomes postoperatively (predictability), assessment of changes in themean spherical equivalent (SEQ) over the time (stability),assessment of quality of vision by examination of contrast sensitivity using computer software (Chart 2020, Konan medical) and analysis of complications.
Table 1 Patient demographic and clinical characteristics n (%)
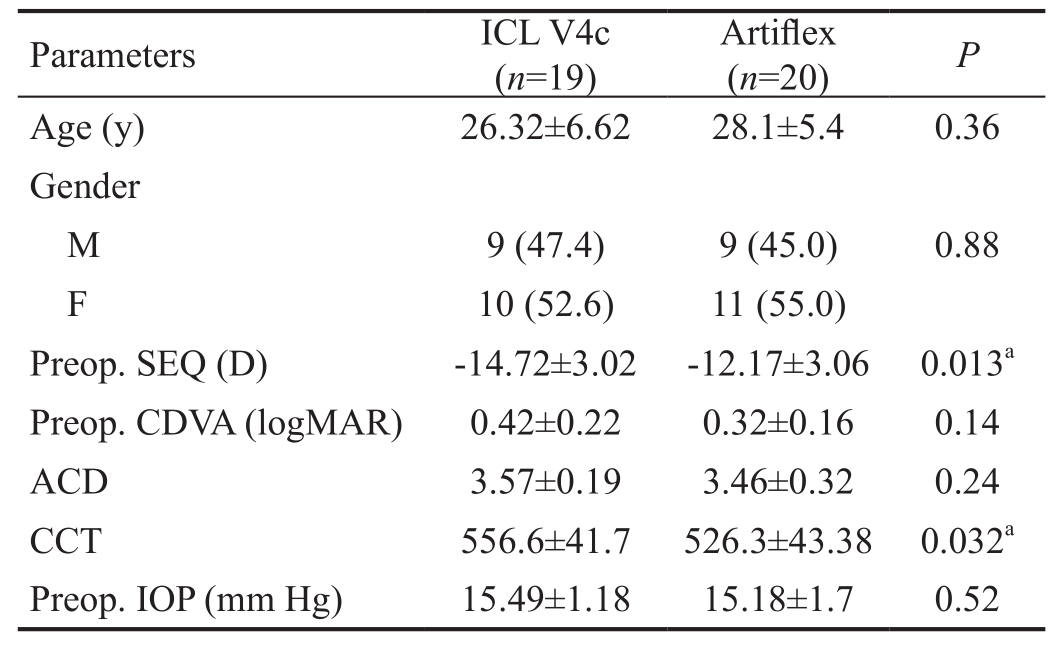
ACD: Anterior chamber depth; CDVA: Corrected distant visual acuity; ICL: Implantable collamer lens; IOP: Intraocular pressure;SEQ: Spherical equivalent; CCT: Central corneal thikness.aStatistically significant.
?
Statistical Analysis Data were fed to the computer and analyzed using IBM SPSS software package version 20.0(SPSS, Inc., Chicago, IL, USA and Microsoft Excel 2007“Microsoft Corporation, New York, NY, USA”). Visual acuity was changed to logMAR measuring unit for the purpose of precise statistical analysis. Significance of the obtained results was judged at the 5% level. P-values less than 0.05 was considered statistically significant. The Chi-square test,Student's t test, paired t-test and linear regression analysis were used.
Patient's Characteristics The data were collected and recorded from January 2014 to January 2016. The study included 39 eyes of 23 patients, 18 (46.2%) males and 21 (53.8%) females. Of 19 eyes underwent Visian ICL (model V4c) implantation (ICL V4c group) and 20 eyes underwent Artiflex lens implantation (Artiflex group). All patients completed the follow up duration (Table 1).
Comparison between both groups revealed statistically insignificant difference as regard age (26.32±6.62y for ICL V4c and 28.1±5.4y for Artiflex, P=0.36), preoperative CDVA(0.42±0.22 logMAR for ICL V4c and 0.32±0.16 logMAR for Artiflex, P=0.14) and preoperative intraocular pressure(15.49±1.18 mm Hg for ICL V4c and 15.18±1.7 mm Hg for Artiflex, P=0.52). While a statistically significant difference was found in preoperative SEQ (-14.72±3.02 D for ICL V4c and -12.17±3.06 D for Artiflex, P=0.013). There was statistically insignificant difference between both groups regarding postoperative SEQ (-0.78±0.7 D for ICL V4c and-0.719±0.6 D for Artiflex, P=0.8), CDVA (0.155±0.1 logMAR for ICL V4c and 0.147±0.1 logMAR for Artiflex, P=0.87),UDVA (0.33±0.2 logMAR for ICL V4c and 0.37±0.2 logMAR for Artiflex, P=0.59) and intraocular pressure (15.64±1.13 mm Hg for ICL V4c and 15.32±1.6 mm Hg for Artiflex, P=0.48) at 12th month (Table 2).
In Visian V4C group, manifest SEQ and mean UDVA and CDVA were changed significantly from preoperative values-14.72±3.02 D, 0.421±0.22 logMAR, 1.62±0.23 logMAR to postoperative 12th month values -0.78±0.7 D, 0.155±0.1 logMAR,0.33±0.2 logMAR respectively while in Artiflex group-12.17±3.06 D, 0.324±0.16 logMAR, 1.46±0.21 logMAR to postoperative 12th month values -0.719±0.6 D, 0.147±0.1 logMAR,0.37±0.2 logMAR respectively (Table 2).
Safety Index In ICL V4c group, 2 eyes (10.5%) had unchanged CDVA, 7 eyes (36.8%) gained one line, 6 eyes(31.5%) gained two lines and 4 eyes (21%) gained more than two lines while in Artiflex group 4 eyes (20%) had unchanged CDVA, 11 eyes (55%) gained one line and 3 eyes (15%)gained two lines and 2 eyes (10%) gained more than two lines.No eyes lost lines of CDVA in either group.
The safety indices for ICL V4c group at 1wk, 1, 3, 6 and 12mo were 1.57, 1.67, 1.70, 1.67 and 1.67.
The safety indices for Artiflex group at 1wk, 1, 3, 6 and 12mo were 1.26, 1.26, 1.34, 1.60 and 1.34.
Efficacy Index The manifest SEQ changed significantly from -14.72±3.02 D preoperatively to -0.78±0.7 D 12mo postoperatively in ICL V4c group. Also, mean CDVA changed significantly from 0.421±0.22 logMAR preoperatively to 0.155±0.1 logMAR 12mo postoperatively, postoperative astigmatism after 12mo was -1.15±0.73 D.
For Artiflex group, manifest SEQ changed significantly from -12.17±3.06 D preoperatively to -0.719±0.6 D 12mo postoperatively. Also, mean CDVA changed significantly from 0.324±0.16 logMAR preoperatively to 0.147±0.1 logMAR 12mo postoperatively. Postoperative astigmatism after 12mo was -0.87±1.17 D.
The efficacy indices for ICL V4c group at 1wk, 1, 3, 6 and 12mo were 1.0, 1.25, 1.25, 1.25 and 1.25.
The efficacy indices for Artiflex group at 1wk, 1, 3, 6 and 12mo were 0.8, 1.0, 0.8, 0.8 and 0.8.
Predictability After 12mo postoperativefifteen eyes (78.9%)were within one diopter SEQ in ICL V4c group compared to fourteen eyes (70%) in Artiflex group. R2 was 0.934 for ICL V4c group and 0.958 for Artiflex group (Figure 3).
Stability Postoperative mean SEQ was stable in both ICL V4c and Artiflex groups (Figure 4).
Contrast Sensitivity The differences at five spatial frequencies between both groups was statistically insignificant at 12th postoperative month (Table 3).
Table 2 Preoperative and 12th postoperative month data in both groups

ICL: Implantable collamer lens; CDVA: Corrected distant visual acuity; UDVA: Uncorrected visual acuity; IOP: Intraocular pressure;SEQ: Spherical equivalent; CCT: Central corneal thickness.
aStatistically significant.
 Age (y) 26.32±6.62 28.1±5.4 0.36 Preop.SEQ (D) -14.72±3.02 -12.17±3.06 0.013a CDVA (logMAR) 0.421±0.22 0.324±0.16 0.14 UDVA (logMAR) 1.62±0.23 1.46±0.21 0.12 IOP (mm Hg) 15.49±1.18 15.18±1.7 0.52 CCT (μm) 556.6±41.7 526.3±43.38 0.032a Q value -0.40±0.06 -0.35±0.09 0.24 Postop. 12mo SEQ (D) -0.78±0.7 -0.719±0.6 0.8 CDVA (logMAR) 0.155±0.1 0.147±0.1 0.87 UDVA (logMAR) 0.33±0.2 0.37±0.2 0.59 IOP (mm Hg) 15.64±1.13 15.32±1.6 0.48
Age (y) 26.32±6.62 28.1±5.4 0.36 Preop.SEQ (D) -14.72±3.02 -12.17±3.06 0.013a CDVA (logMAR) 0.421±0.22 0.324±0.16 0.14 UDVA (logMAR) 1.62±0.23 1.46±0.21 0.12 IOP (mm Hg) 15.49±1.18 15.18±1.7 0.52 CCT (μm) 556.6±41.7 526.3±43.38 0.032a Q value -0.40±0.06 -0.35±0.09 0.24 Postop. 12mo SEQ (D) -0.78±0.7 -0.719±0.6 0.8 CDVA (logMAR) 0.155±0.1 0.147±0.1 0.87 UDVA (logMAR) 0.33±0.2 0.37±0.2 0.59 IOP (mm Hg) 15.64±1.13 15.32±1.6 0.48
Table 3 Contrast sensitivity at 12th postoperative month in both groups
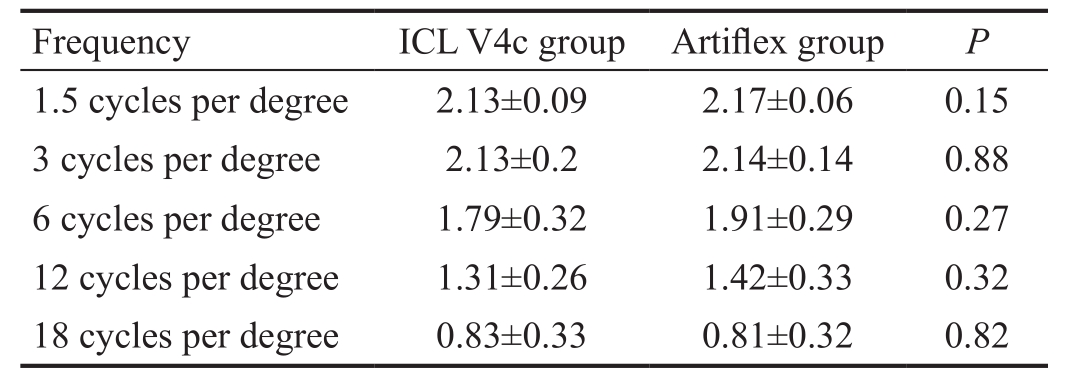
 1.5 cycles per degree 2.13±0.09 2.17±0.06 0.15 3 cycles per degree 2.13±0.2 2.14±0.14 0.88 6 cycles per degree 1.79±0.32 1.91±0.29 0.27 12 cycles per degree 1.31±0.26 1.42±0.33 0.32 18 cycles per degree 0.83±0.33 0.81±0.32 0.82
1.5 cycles per degree 2.13±0.09 2.17±0.06 0.15 3 cycles per degree 2.13±0.2 2.14±0.14 0.88 6 cycles per degree 1.79±0.32 1.91±0.29 0.27 12 cycles per degree 1.31±0.26 1.42±0.33 0.32 18 cycles per degree 0.83±0.33 0.81±0.32 0.82
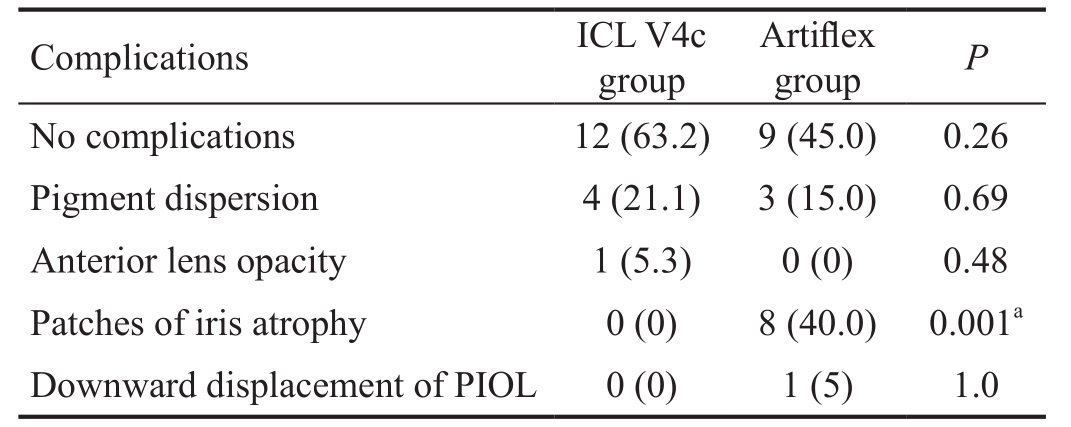
Complications Few low risk complications have been found throughout the follow up period with insignificant difference between both groups (Table 4).
Our results agree with the study conducted by Awadein and Habib[11] that was done on 24 patients with myopia in both eyes, one eye had ICLs implantation and the other eye had Artiflex phakic intraocular lens implantation. They reported that there was a significant improve in CDVA in both groups.The difference in postoperative UDVA or CDVA between the two groups was statistically insignificant (P=0.41 and 0.36 respectively) and no eye lost lines of CDVA in either group[11].A study compared between ICLs and the unfoldable model of iris fixed phakic intraocular lenses (Artisan) was conducted by Hassaballa and Macky[12] on 68 highly myopic eyes of 34 patients: 42 eyes had Artisan phakic intraocular lenses implantation and 26 eyes had Vasian ICLs implantation. The study reported statistically insignificant difference between the two groups concerning postoperative UDVA (P=0.268), CDVA(P=0.128), and SEQ (P=0.67)[12].
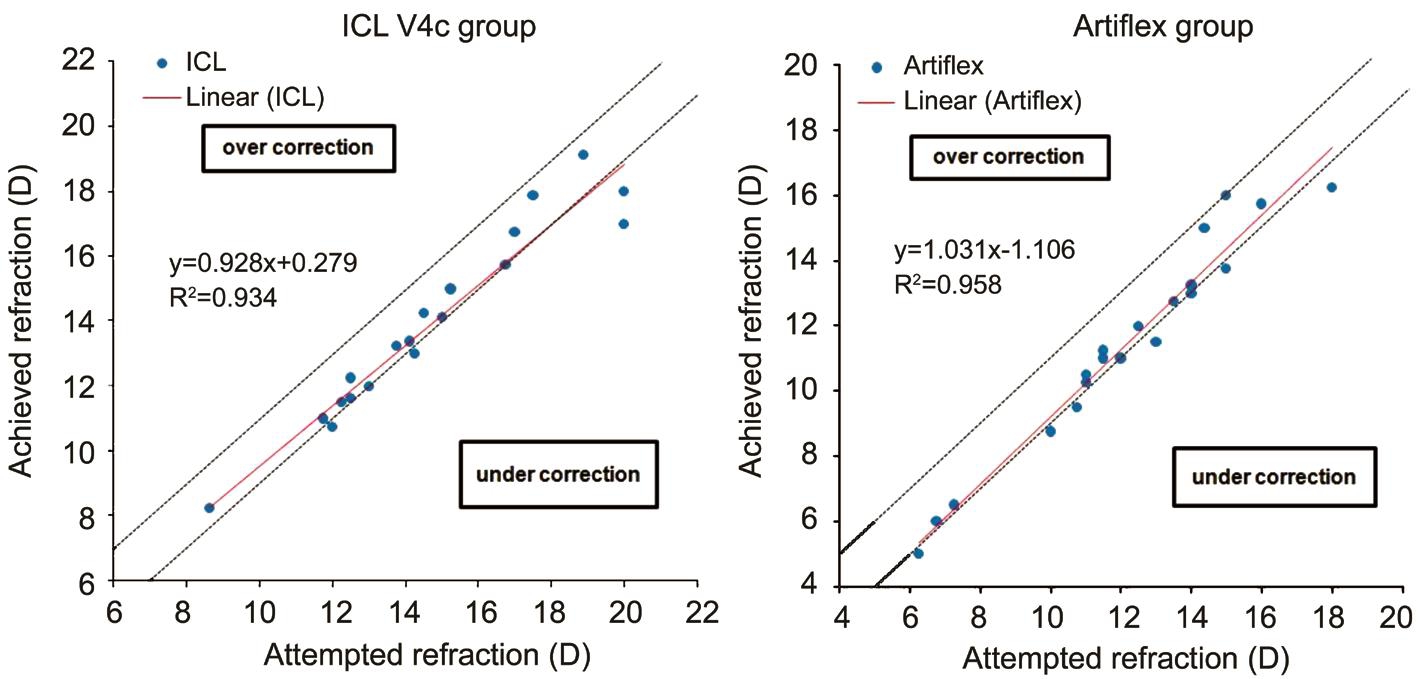
Figure 3 Attempted versus achieved correction in both groups.
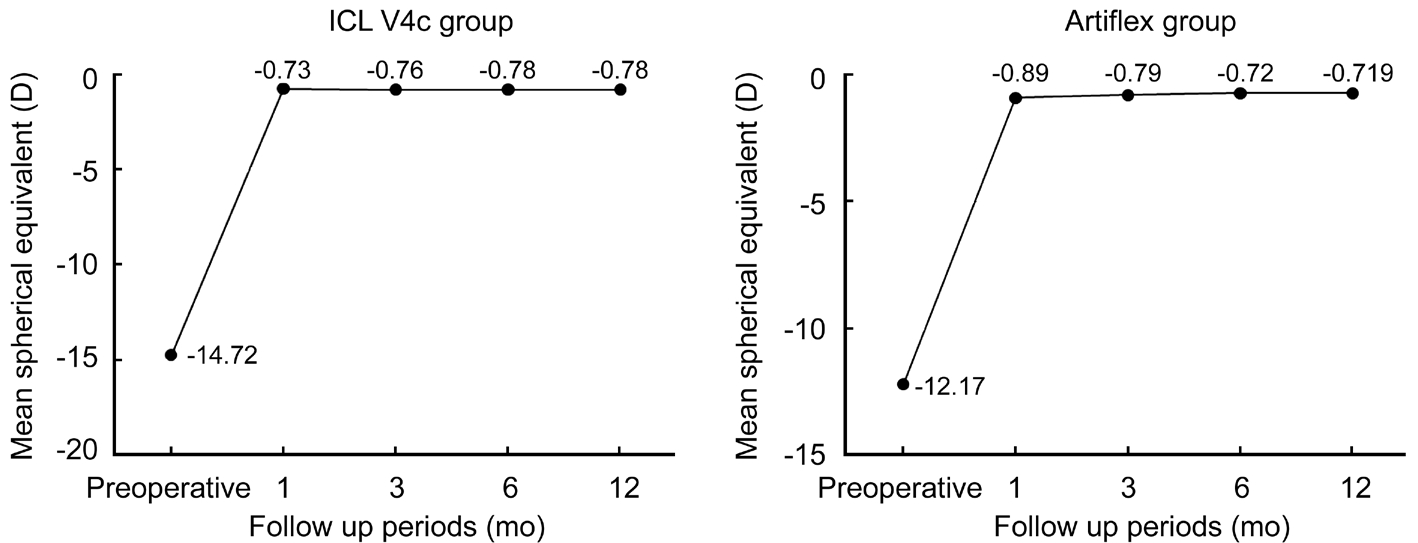
Figure 4 Stability of spherical equivalent (SEQ) in both groups along follow up period.
Table 4 Postoperative complications in both groups n (%)
PIOL: Phakic intraocular lens.aStatistically significant.
?
Boxer Wachler et al[13] conducted a study on 61 high myopic eyes to compare refractive and visual results between the Visian ICL and Verisyse phakic intraocular lens. They concluded that both groups had comparable monocular UDVA as in this study. However unlike this study, they reported that refractive outcomes were more accurate in the ICLs group than the Verisyse lens group. They referred that to the postoperative dynamic movement of the iris claw phakic intraocular lens,which may affect predictability of refractive outcomes and deviation from the target refraction. Their interpretation was based on Sekundo et al[14] study that revealed forward movement of the iris-claw phakic intraocular lens which occurs during the process of accommodation using optical coherence biometry[13-14].
As regards contrast sensitivity, the results of our study was parallel to Awadein and Habib's study[12] as they reported statistically insignificant difference in postoperative contrast sensitivity.
In this study, one eye (5.3%) in ICL V4c group had fine anterior subcapsular lens opacity which was caused by inadvertent iatrogenic touch of crystalline lens during implantation. It was presented during early follow up sessions and remained stable throughout the whole follow up period without effect on CDVA. This rate is similar to that of Sanders's study[15] where subcapsular opacity rate was (5.9%).Lackner et al[16] reported an increased probability of cataract formation in patients aged over 45y underwent Visian lens implantation which couldn't be investigated in current study due to younger age range of the study[15-16].
No cataract formation noticed in Artiflex group during the twelve months postoperative follow up period in this study.This may be due to the relatively short follow-up duration.Menezo et al[17] study included 137 eyes. They mentioned that, nuclear cataract was developed in two eyes of two patients (1.46%) after Artisan (unfoldable version of Artiflex)intraocular lens implantation. The mean time of development of nuclear cataract after Artisan phakic intraocular lens implantation was 54.83±22.12mo (range 35-99mo). They suggested that, high axial myopia and age of patient at the time of operation are relevant to early development of nuclear cataract after implantation of Artisan phakic intraocular lens.Pigment dispersion occurred in four eyes of ICL V4c group(21.1%) and three eyes (15.0%) of Artiflex groups. These results were similar to that of Menezo et al[17] study in which incidence of pigment deposits was (38.1%) in ICLs group with lower incidence (6.57%) in Artisan (unfoldable version of Artiflex) group. Contact between posterior chamber intraocular lens and the iris increases the probability of pigment dispersion and explains the higher incidence of pigment dispersion in ICLs than Artiflex. However, Hassaballa and Macky's study[12]showed different results as they found pigment dispersion in two eyes (15.38%) in the Visian ICL group and in twelve eyes(28.6%) in the Artisan phakic intraocular lens group.
A frequent cause for high intraocular pressure in previous models of ICL was pupillary block, so preoperative neodymium: Yttrium aluminum garnet (YAG) laser iridotomy or intraoperative peripheral iridectomy was mandatory to prevent such a complication. Fortunately introduction of central hole in the new model V4c used in this study offers surgical advantages over earlier models by insuring better aqueous fl ow and so, eliminating the need for laser iridotomy or peripheral iridectomy as these procedure may induce discomfort for patient or intraoperative surgical difficulties in some cases[18-19].
There was no incidence of endophthalmitis or retinal detachment after implantation of either ICL V4c or Artiflex lens in this study. Arne reported that, the risk of retinal detachment was lower in patients had phakic intraocular lens implantation than in patients had clear lens extraction. In this study, the number of subjects was too low to adequately detect endophthalmitis or retinal detachment[20].
Advantage of this study (based on its results) is to facilitate making the decision about the type of phakic intraocular lense to be implanted to correct high myopia because comparison between both types of phakic intraocular lenses (ICL V4c and Artiflex) showed that both are effective, safe, stable and predictable with equal visual performance and acceptable low risk short time complications and so considerations may be directed to other concerns like availability or price of those phakic intraocular lenses.
Disadvantages and limitations of this study were related to a relatively short follow up period and small study sample because longer postoperative follow up period. And larger study sample are needed for e precise assessment of longterm complications and safety of phakic intraocular lens implantation. In this study we focused on refractive outcomes rather than endothelial cell count which is considered as a shortcoming, lack of assessment of high order aberrations is another shortcoming.
Future studies should include the toric models of ICL V4c and Artiflex with long term postoperative evaluation to assess efficacy, safety and stability of these models in correction of high myopia with accompanying high astigmatism.
Based on the study results, we recommend the use of ICL V4c and Artiflex lens for correction of high myopia as both of these phakic intraocular lenses showed equal qualitative and quantitative visual performance.
In conclusion, both ICL V4c and Artiflex lense showed equal and comparable safety and efficacy with stable and predictable refractive outcomes with no vision threatening complications.
Conflicts of Interest: Rizk IM, None; Al-hessy AA, None;El-Khouly SE, None; Sewelam AM, None.
1 Alió JL, Ortiz D, Muftuoglu O, Garcia MJ. Ten years after photorefractive keratectomy (PRK) and laser in situ keratomileusis (LASIK) for moderate to high myopia (control-matched study). Br J Ophthalmol 2009;93(10):1313-1318.
2 Liang GL, Wu J, Shi JT, Liu J, He FY, Xu W. Implantable collamer lens versus iris- fixed phakic intraocular lens implantation to correct myopia: a meta-analysis. PLoS One 2014;9(8):e104649.
3 Huang D, Schallhorn SC, Sugar A, Farjo AA, Majmudar PA, Trattler WB, Tanzer DJ. Phakic intraocular lens implantation for the correction of myopia: a report by the American Academy of Ophthalmology.Ophthalmology 2009;116(11):2244-2258.
4 Pineda R 2nd, Chauhan T. Phakic intraocular lenses and their special indications. J Ophthalmic Vis Res 2016;11(4):422-428.
5 Stulting RD, John ME, Maloney RK, Assil KK, Arrowsmith PN,Thompson VM, U.S. Verisyse Study Group. Three-year results of Artisan/Verisyse phakic intraocular lens implantation. Results of the United States Food And Drug Administration clinical trial. Ophthalmology 2008;115(3):464-472.e1.
6 Simões PS, Ferreira TB. Iris-fixated intraocular lenses for ametropia and aphakia. Med Hypothesis Discov Innov Ophthalmol 2014;3(4):116-122.
7 Alfonso JF, Lisa C, Abdelhamid A, Fernandes P, Jorge J, Montés-Micó R. Three-year follow-up of subjective vault following myopic implantable collamer lens implantation. Graefes Arch Clin Exp Ophthalmol 2010;248(12):1827-1835.
8 Dougherty PJ, Priver T. Refractive outcomes and safety of the implantable collamer lens in young low-to-moderate myopes. Clin Ophthalmol 2017;11:273-277.
9 Pineda R 2nd, Chauhan T. Phakic intraocular lenses and their special indications. J Ophthalmic Vis Res 2016;11(4):422-428.
10 Milling AF, O'connor AR, Newsham D. The importance of contrast sensitivity testing in children. British and Irish Orthoptic Journal 2014;11:9.
11 Awadein A, Habib AE. ICL versus Veri fl ex phakic IOL for treatment of moderately high myopia: randomized paired-eye comparison. J Refract Surg 2013;29(7):445-452.
12 Hassaballa MA, Macky TA. Phakic intraocular lenses outcomes and complications: Artisan vs Visian ICL. Eye (Lond) 2011;25(10):1365-1370.
13 Boxer Wachler BS, Scruggs RT, Yuen LH, Jalali S. Comparison of the Visian ICL and Verisyse phakic intraocular lenses for myopia from 6.00 to 20.00 diopters. J Refract Surg 2009;25(9):765-770.
14 Sekundo W, Bissmann W, Tietjen A. Behaviour of the phakic iris-claw intraocular lens (Artisan /Verisyse) during accommodation: an optical coherence biometry study. Eur J Ophthalmol 2007;17(6):904-908.
15 Sanders DR. Anterior subcapsular opacities and cataracts 5 years after surgery in the visian implantable collamer lens FDA trial. J Refract Surg 2008;24(6):566-570.
16 Lackner B, Pieh S, Schmidinger G, Hanselmayer G, Dejaco-Ruhswurm I, Funovics MA, Skorpik C. Outcome after treatment of ametropia with implantable contact lenses. Ophthalmology 2003;110(11):2153-2161.
17 Menezo JL, Peris-Martínez C, Cisneros AL, Martínez-Costa R. Phakic intraocular lenses to correct high myopia: Adatomed, Staar, and Artisan. J Cataract Refract Surg 2004;30(1):33-44.
18 Smallman DS, Probst L, Rafuse PE. Pupillary block glaucoma secondary to posterior chamber phakic intraocular lens implantation for high myopia. J Cataract Refract Surg 2004;30(4):905-907.
19 Lisa C, Naveiras M, Alfonso-Bartolozzi B, Belda-Salmerón L, Montés-Micó R, Alfonso JF. Posterior chamber collagen copolymer phakic intraocular lens with a central hole to correct myopia: one-year follow-up.J Cataract Refract Surg 2015;41(6):1153-1159.
20 Arne JL. Phakic intraocular lens implantation versus clear lens extraction in highly myopic eyes of 30- to 50-year-old patients. J Cataract Refract Surg 2004;30(10):2092-2096.