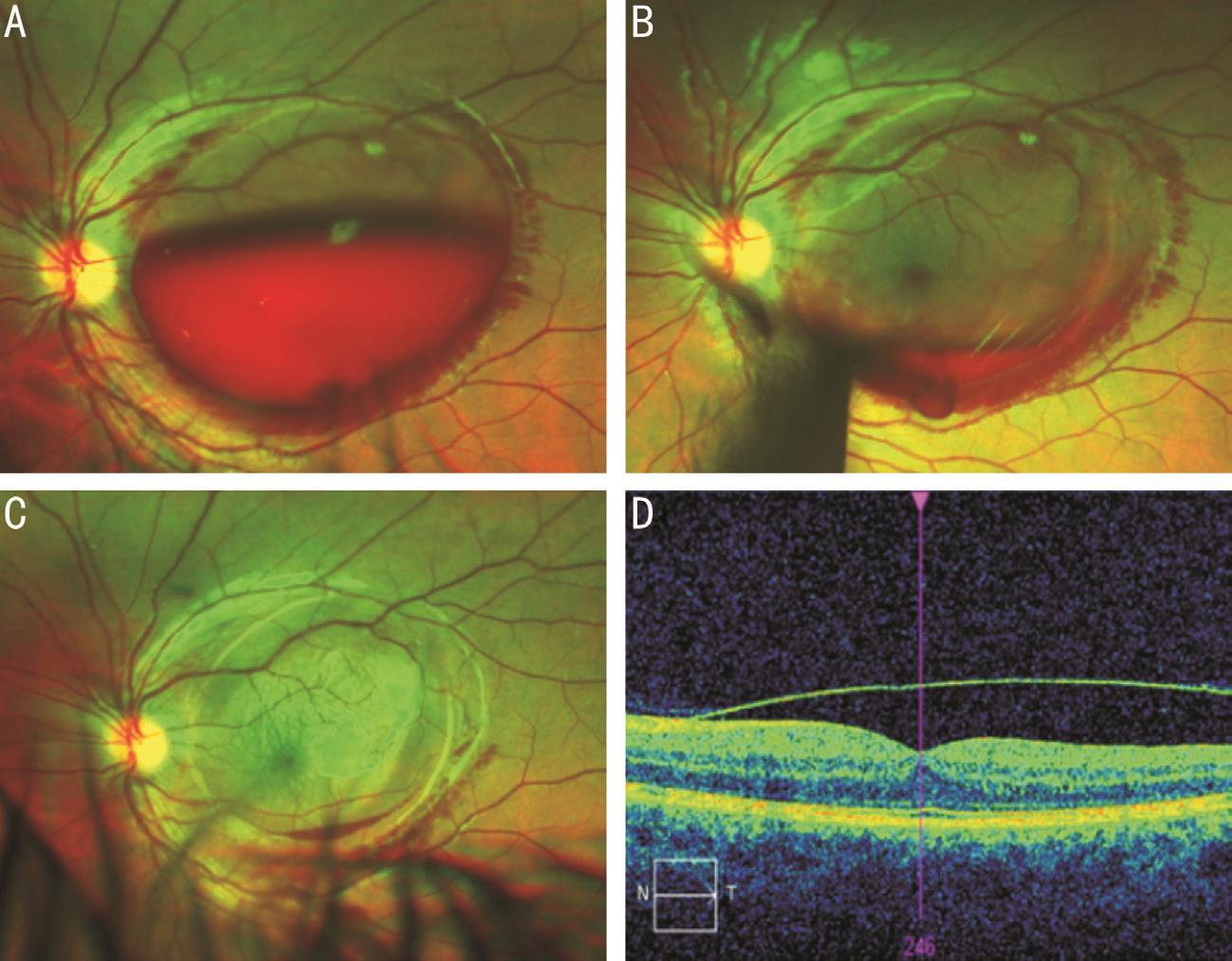
Figure 1 Serial wide-angle fundus photography
A: Day of presentation; B: 1-week review; C: 6-week review; D: 6-week OCT.
Dear Editor,
O ur authors present a three-case series review of subhyaloid haemorrhage presentations in a Tasmanian centre during 2017. Same-day Nd:YAG laser hyaloidotomy was performed in each case with rapid improvement of visual acuity. All cases reported were presented with informed consent; this study was performed according to principles of Good Clinical Practice(GCP) and ethical considerations outlined in the Declaration of Helsinki.
Premacular subhyaloid haemorrhage often presents as sudden,painless vision loss[1]. Common causes include Valsalva retinopathy, acute intracranial conditions (subarachnoid haemorrhage or direct trauma) or as a complication of retinal vascular disorders including retinal vein occlusion, diabetic retinopathy, macroaneurysm and macular degeneration[1-2].
Nd:YAG laser hyaloidotomy can drain the haemorrhage into the vitreous, facilitating reabsorption and potentially offering rapid restoration of vision[3]. Other management options include observation, intravitreal pneumatic displacement after tissue plasminogen activator (tPA) and pars plana vitrectomy(PPV)[1-2,4-7]. All patients within this series were treated using the Ellex Ultra Q Re fl exTM YAG laser and Ocular Instruments®OJK-3S vitreolysis contact lens.
Patient 1 A 16-year-old male presented with overnight onset loss of vision in his left eye after an episode of respiratory distress secondary to severe asthma. Best corrected visual acuity (BCVA) was 6/6 in the unaffected right eye and hand movements (HM) in the left eye. Intraocular pressures were 21 mm Hg bilaterally. Ocular coherence tomography (OCT)and fundus photography demonstrated a large subhyaloid haemorrhage (Figure 1). Maximal diameter was equal to 5.5 disc diameters.
The patient was treated with Nd:YAG laser hyaloidotomy,achieving immediate drainage with 16 shots at 4 mJ. Review at one-week demonstrated improved BCVA to 6/7.5. Complete resolution occurred by eight weeks.
Patient 2 A 50-year-old male presented with a four-day history of vision loss in his left eye. His past medical history included hypertension and type 2 diabetes. Presenting BCVA was 6/6 in the unaffected right eye and light perception in the left. Intraocular pressures were 12 and 8 mm Hg respectively.
Examination revealed a large subhyaloid haemorrhage(Figure 2), 4 disc diameters on the horizontal axis, with no evidence of diabetic retinopathy; it was presumed that the haemorrhage occurred from an arterial macroaneurysm along the inferior vascular arcade. Initial Nd:YAG laser hyaloidotomy of 13 shots of 4 mJ resulted in minimal drainage,raising the suspicion of organised clot formation. The patient returned the following day, with vision is his left eye improved to count fingers and underwent a further 12 shots at 4 mJ of Nd:YAG laser in a more inferior position, which achieved visible drainage. BCVA at one week post-drainiange was 6/30.At 8wk there was complete haematoma resolution while the patient's vision continued to improve and was 6/6 at 20wk.
Patient 3 A 90-year old female presented with a 24-hour deteriorating vision in her left eye, describing ‘clusters of stripes and spots' in her central vision. The patient's ocular history included a choroidal neovascular membrane (CNVM)in the same eye, diagnosed in 2010 and treated with monthly intravitreal ranibizumab. Prior to presentation she maintained a BCVA at 6/30.
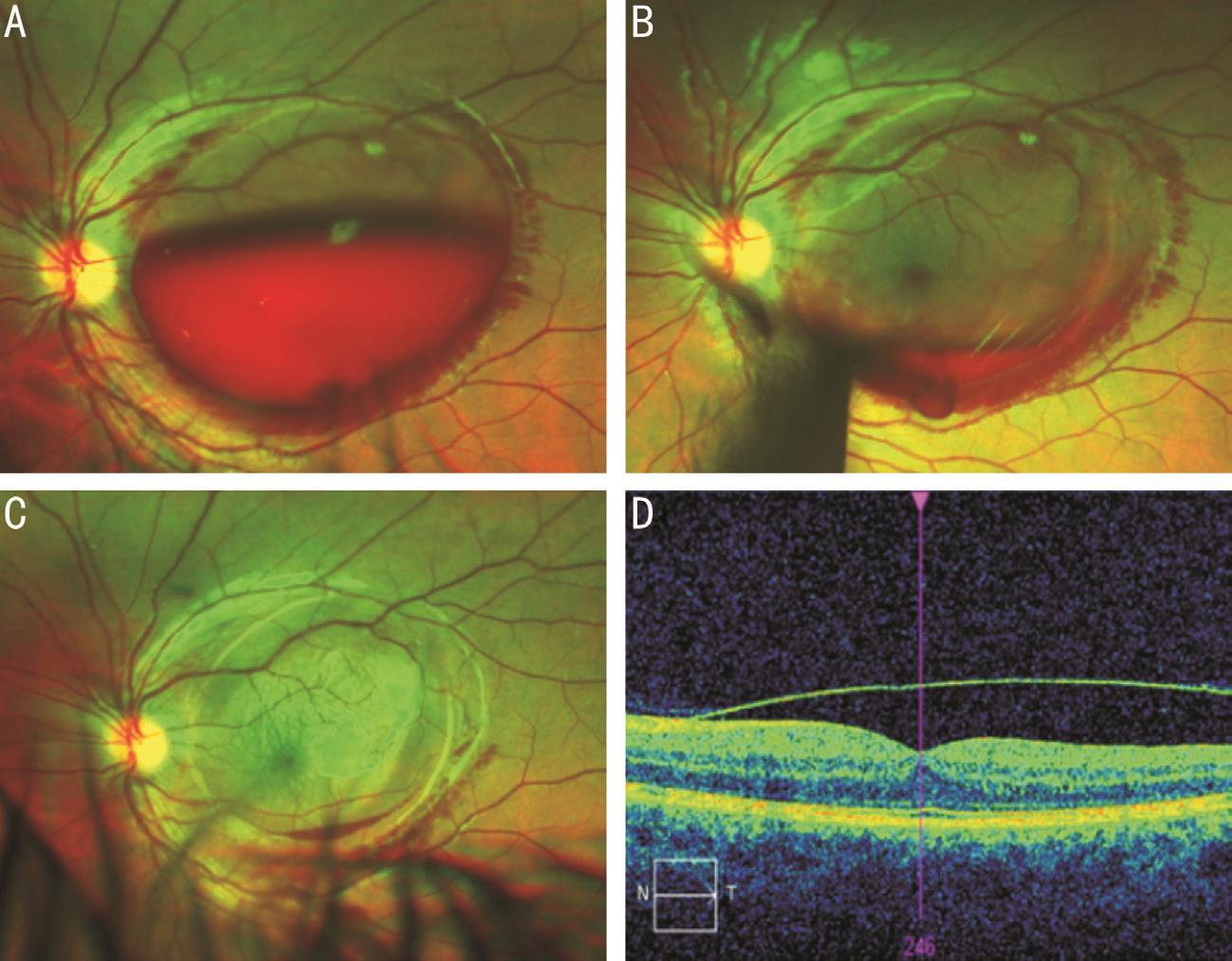
Figure 1 Serial wide-angle fundus photography
A: Day of presentation; B: 1-week review; C: 6-week review; D: 6-week OCT.

Figure 2 Fundus photography of patient 2
A: At presentation; B: 24-hour review.
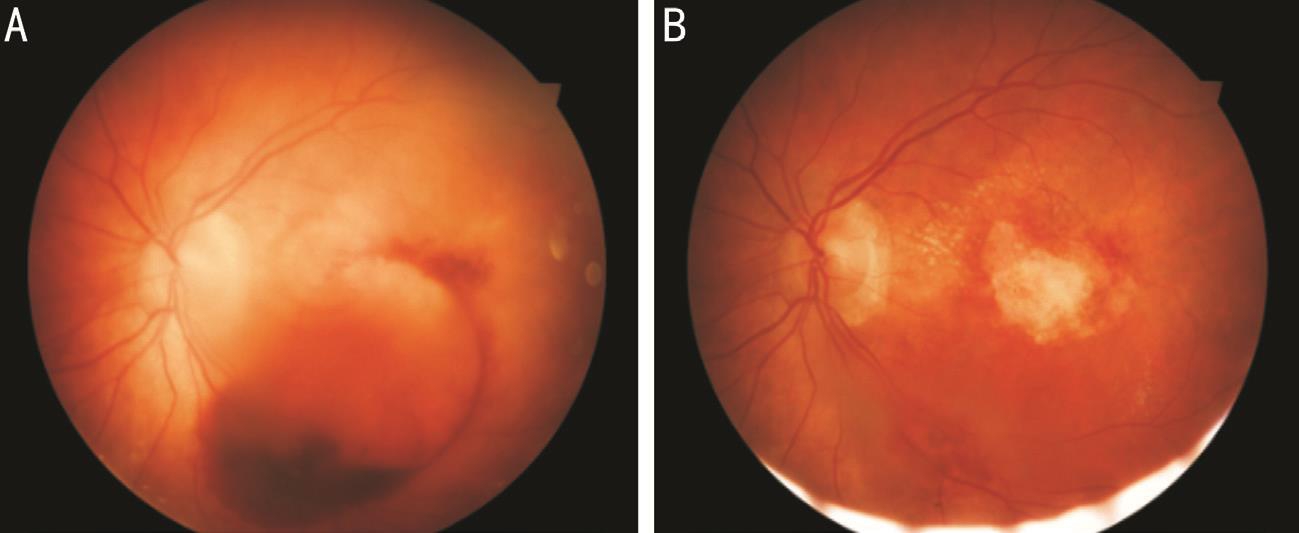
Figure 3 Fundoscopy of patient 3
A: Day of presentation; B: 8wk post-laser therapy. Note changes from previous photodynamic therapy.
At presentation, the patient's vision had deteriorated to a BCVA of 6/60. Fundoscopy demonstrated a subhyaloid haemorrhage,with maximal dimensions of 3 disc diameters. This was effectively drained with Nd:YAG hyaloidotomy, using 12 shots at 4 mJ (Figure 3). One-week review demonstrated dispersion of haemoglobin throughout the vitreous, though this resolved within one week with BCVA returning to 6/30. The patient has continued regular ranibizumab treatment with stable visual acuities since and without any further complications.
Our presented case series offers insight into the variable aetiologies of subhyaloid haemorrhages[1-4,6,8] in addition to the age range patients who may present with this pathology.Regardless of cause, many subhyaloid haemorrhages are amenable to laser therapy.
Keys to effective delivery of treatment have been previously reported[1,3,8]. Directing therapy away from major vessels and the fovea to prevent unwanted photomechanical damage is prudent, though the haemorrhage acts as an effective safeguard for the underlying retina reducing the risk of retinal hole formation or new choroidal haemorrhages[7-8]. Previous studies have recommended laser therapy for haemorrhages of at least 3-disc diameters to ensure a sizeable barrier, which was observed in this cohort[4]. An inferior puncture allows for gravity-assisted drainage, though lateral breach and headtilting is possible if an inferior breach is undesirable[2,4].
As demonstrated in patient 2, prompt treatment ensures minimal clot organisation to allow outflow. We note that within our case series, in order to achieve effective drainage more shots were required than several other series; given similar laser techniques reported, no discernible reason has been identified,though it may be attributed to minor offset of repeated shots,to avoid prolonged and repeated exposure to a single point of underlying retina. Other barriers to effective treatment include difficulty in Nd:YAG delivery due to abnormal corneal curvature or cataracts[1]. In these cases, or those where clot organisation prevents drainage, alternate therapeutic options are available.Intravitreal injection and pneumatic displacement has been used for haemorrhages associated with age-related macular degeneration[4]. tPA facilitates clot breakdown and subsequent gas injection (air, octafluoropropane or sulfur hexafluoride)displaces the haematoma from the macula[4,8]. PPV, while definitive,requires surgical intervention with attendant risks[2-3,8].
A conservative approach: awaiting reabsorption and resolution is possible, though this process may take 1-2mo[2-4]. Permanent vision loss remains a risk throughout this time due to pigmentary macular changes, formation of a reactive epiretinal membrane, or toxic retinal damage secondary to prolonged haemoglobin exposure[1].
In conclusion, timely use of Nd:YAG laser treatment in subhyaloid haemorrhages offers an immediate, effective ambulatory treatment choice. If initially unsuccessful due to clot organisation the procedure may be repeated, however keys to effective intervention include a short duration from initial symptoms to treatment and an inferiorly position puncture to allow effective drainage.
Conflicts of Interest: McCartney M, None; Verma N, None;Traill A, None.
1 Khadka D, Bhandari S, Bajimaya S, Thapa R, Paudyal G, Pradhan E.Nd:YAG laser hyaloidotomy in the management of premacular subhyaloid hemorrhage. BMC Ophthalmol 2016;16:41.
2 Kuruvilla O, Munie M, Shah M, Desai U, Miller JA, Ober MD. Nd:YAG membranotomy for preretinal hemorrhage secondary to valsalva retinopathy. Saudi J Ophthalmol 2014;28(2):145-151.
3 Murtaza F, Rizvi SF, Bokhari SA, Kamil Z. Management of macular pre-retinal subhyaloid hemorrhage by Nd:YAG laser hyaloidotomy. Pak J Med Sci 2014;30(2):339-342.
4 Hillenkamp J, Surguch V, Framme C, Gabel VP, Sachs HG. Management of submacular hemorrhage with intravitreal versus subretinal injection of recombinant tissue plasminogen activator. Graefe's Arch Clin Exp Ophthalmol 2010;248(1):5-11.
5 Heichel J, Kuehn E, Eichhofirst A, Hammer T, Winter I. Nd:YAG laser hyaloidotomy for the treatment of acute subhyaloid hemorrhage: a comparison of two cases. Ophthalmol Ther 2016;5(1):111-120.
6 Rennie CA, Newman DK, Snead MP, Flanagan DW. Nd:YAG laser treatment for premacular subhyaloid haemorrhage. Eye (Lond) 2001;15(Pt 4):519-524.
7 Karagiannis D, Kontadakis GA, Flanagan D. ND:YAG laser for preretinal hemorrhage in diabetic retinopathy. Am J Ophthalmol Case Rep 2018;10:8-9.
8 Alarfaj MA, Hasen AA, Al-Yami SS. Traumatic subhyaloid macular hemorrhage with complete resolution following neodymium-doped yttrium aluminium garnet laser. Am J Ophthalmol Case Rep 2018;9:85-87.