INTRODUCTION
According to selection criteria for intraocular lens (IOL)use, cataract patients with regular corneal astigmatism<1.0 diopter (D) can choose the multifocal IOL AcrySof IQ ReSTOR IOL (ReSTOR) to correct presbyopia. Cataract patients who have regular corneal astigmatism of 0.5-2.5 D,and wish to correct presbyopia, can choose a toric multifocal IOL, such as Acrysof IQ ReSTOR Toric IOL (ART). ART has different types corresponding to the astigmatism correction range (ART2 to ART5). Patients with regular corneal astigmatism of 0.75-1.0 D with-the-rule or 0.5-0.75 D against-therule can choose ReSTOR or ART2 to correct presbyopia. The choice of ReSTOR or ART2 mainly depends on the patients’financial situation, rather than the reported selection criteria.To our knowledge, no previous studies have been conducted regarding the impact of low corneal astigmatism on the multifocal pseudophakic eye. However, postoperative optical quality is known to be reduced by residual astigmatism, and its impact is aggravated with increased residual astigmatism[1-3].Therefore, this study was designed to compare optical quality in cataract patients with low corneal astigmatism after ART2 and ReSTOR IOL implantation, and to provide a theoretical basis for the selection of multifocal IOL by cataract patients who have low corneal astigmatism.
SUBJECTS AND METHODS
Ethical Approval This retrospective observation study was approved by the Institutional Review Board of Tianjin Medical University Eye Hospital. Informed consent was waived due to the retrospective nature of the study.
Subjects A retrospective patient chart review was performed at Tianjin Medical University Eye Hospital to identify all patients with documented preoperative regular corneal astigmatism of 0.75-1.0 D with-the-rule or 0.5-0.75 D againstthe-rule at the time of surgery. Patients in the department who have this range of cylinder are presented the option of having implantation of an ART2 or ReSTOR. Charts from January 2013 to January 2016 were reviewed.
Eyes were excluded if they had pathology of the cornea,vitreous, macula, or optic nerve; irregular corneal astigmatism;planned extracapsular cataract extraction; a history of ocular surgery or inflammation; patient refusal; and any anticipated difficulties with the examinations, analyses, or follow-ups.
This retrospective review of data included no protected health information. In addition, patients entering the department sign an acknowledgement that their unidentified protected health information data may be used for research purposes. For each eye, preoperative keratometry data and all refractive data available in the chart were recorded. Follow-up was at 1wk, 1,3 and 6mo.
A high percentage of patients chose the ReSTOR (Alcon Laboratories, Fort Worth, TX, USA) option, mainly for economic or other reasons. There were seventeen eyes of seventeen simple age-related cataract patients with preoperative regular corneal astigmatism of 0.75-1.0 D with-the-rule or 0.5-0.75 D against-the-rule underwent the ART2 implantation, whose follow-up data were available and entire for this study.According to age and corneal astigmatism, multistage stratified random sampling were used to choose seventeen eyes of seventeen patients from the charts into the ReSTOR group as control, who had underwent implantation of ReSTOR by the same surgical doctor.
Intraocular Lens The ReSTOR is made of hydrophobic acrylate and shares the biconvex single-piece design, which ensures rotation stability and reduces the incidence rate of posterior capsule opacification[4-5]. The 6.0 mm optic includes an apodized diffractive region in the central portion that measures 3.6 mm and comprises nine concentric steps of gradually decreasing heights. Surrounding the apodized diffractive region in the outer periphery is a refractive area that directs light to a distant focal point. The benefit of these characteristics is satisfactory postoperative distance,intermediate, and near visual acuity[6-7].
Preoperative Evaluation All patients had a comprehensive ophthalmic examination consisting of uncorrected distance visual acuity (UDVA) measurement, corrected distance visual acuity (CDVA) measurement, subjective refraction,keratometry, slit lamp examination, fundoscopy, aberration measurement, Alpha angel measurement, and biometry(LenstarLS900®, iTrace, Haag-StreitAG, Koeniz, Switzerland).
Calculated Formula We considered patients working and reading habits before choosing the lens for implantation. IOL dioptric power was calculated according to accurate biology measurement and formula for IOL design: Hoffer-Q for axial lengths of <22 mm, Holladay between 22 and 25 mm, and Sanders-Retzlaff-Kraff/T for axial lengths of >26 mm. Optical interferometry used the Lenstar LS900 Optical Biometer(Haag-Streit AG) and manual corneal curvature (Haag-Streit AG), which were measured at least three times respectively.
Target Diopter We set the target diopter close to emmetropia:-0.25 to -0.5 D for high myopia patients and -0.25 D for moderate myopia patients; multiple focal IOL implant goal diopter was set at approximately 0.25; 0-0.25 D for emmetropia.
Calculation Online The models of ART2 were calculated on www.acrysoftoriccalculator.com. Additionally, we predicted residual astigmatism.
Operation and Marking Method A single surgeon (Zhang H) performed all surgeries at the same surgical facility in Tianjin Medical University Eye Hospital. Before the implantation of ART2, we marked the dispersion optical axis in two steps: preoperative and intraoperative markings.Preoperative markers were performed on the bedside seat,which were marked on the 0° and 180° of the limbus of the cornea by Ox horn-type marker.
Postoperative Evaluation Evaluations were performed at 1d,1wk, 1, 3, and 6mo postoperatively. All patients underwent a complete ophthalmological evaluation at all visits. Outcome measures were residual astigmatism, UDVA, CDVA. iTrace measurement included aberrations, average modulation transfer function (aMTF), Strehl ratio (SR), and the postoperative axis of ART2. All visual acuity values were calculated according to the logMAR rating scale.
In addition to the above indicators, spectacle independence and patient satisfaction were also evaluated postoperatively as subjective perception index. Postoperative questionnaire survey was conducted after referring to the simplification of the “quality of life questionnaire after multi-focus IOL implantation” in USA. The patients’ satisfaction with postoperative visual state was recorded (very satisfied, basic satisfied, general satisfied, basic dissatisfied, completely dissatisfied); whether glasses should be worn after surgery, the dependence on glasses should be recorded (complete spectacle independence, time<1/2d, time=1/2d, time>1/2d, all day long).
Statistical Analysis Data were analyzed by SPSS 19.0 for Windows. The values are presentedthe mean±standard deviation of the values obtained. Significance was tested using Chi-squared tests and two-sample t-tests by adjusting the level of significance to 5% (P<0.05).
Table 1 Uncorrected visual acuity and overall CDVA mean±SD, logMAR
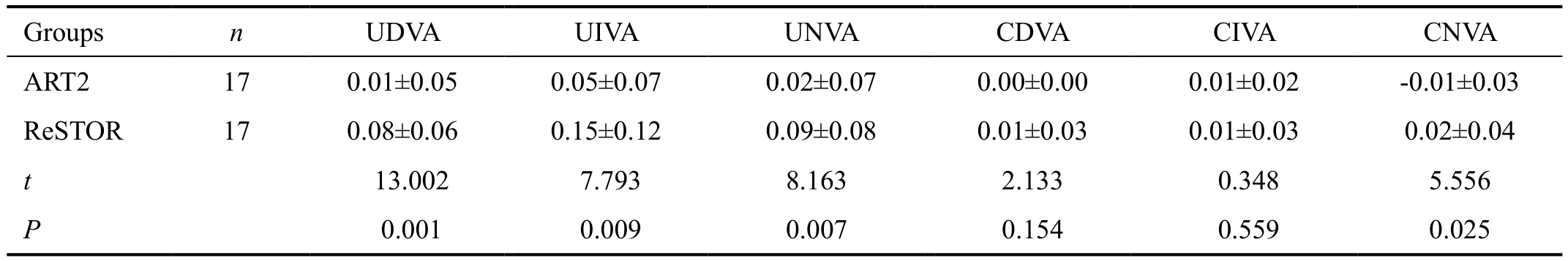
UDVA: Uncorrected distant visual acuity; UIVA: Uncorrected intermediate visual acuity; UNVA: Uncorrected near visual acuity; CDVA:Corrected distance visual acuity; CIVA: Corrected intermediate visual acuity; CNVA: Corrected near visual acuity.
Groups n UDVA UIVA UNVA CDVA CIVA CNVA ART2 17 0.01±0.05 0.05±0.07 0.02±0.07 0.00±0.00 0.01±0.02 -0.01±0.03 ReSTOR 17 0.08±0.06 0.15±0.12 0.09±0.08 0.01±0.03 0.01±0.03 0.02±0.04 t 13.002 7.793 8.163 2.133 0.348 5.556 P 0.001 0.009 0.007 0.154 0.559 0.025
Table 2 Optical quality parameters, spectacle independence and patient satisfaction mean±SD, n (%)
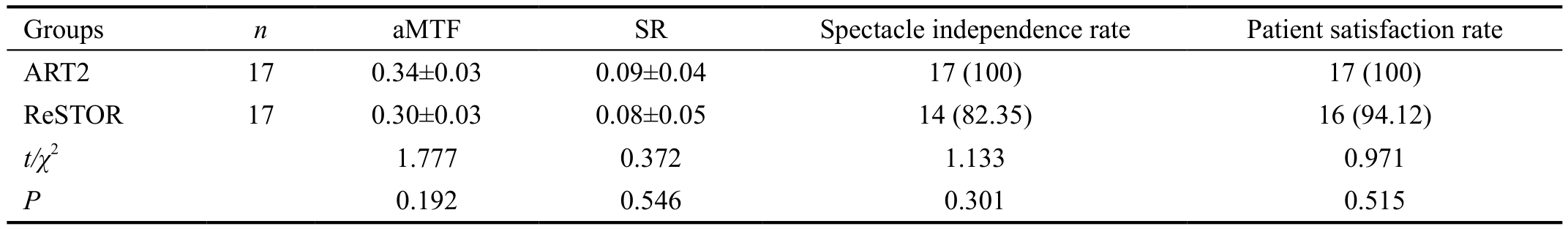
aMTF: Average modulation transfer function; SR: Strehl ratio.
Groups n aMTF SR Spectacle independence rate Patient satisfaction rate ART2 17 0.34±0.03 0.09±0.04 17 (100) 17 (100)ReSTOR 17 0.30±0.03 0.08±0.05 14 (82.35) 16 (94.12)t/χ2 1.777 0.372 1.133 0.971 P 0.192 0.546 0.301 0.515
RESULTS
The study involved 34 patients, 22 men (64.7%) and 12 women (35.3%), and a total of 34 eyes. The average age was 63.82±6.07y. The average corneal astigmatism was 0.68±0.13 D.
Rotational Stability of ART2 Three months after surgery, the average IOL axis rotation of ART2 was 3.12°±0.70°, compared with the preset axis determined by the online calculation.The average rotations at different times (1d, 1wk, 1, 3, 6mo postoperatively) were 1.41°±0.62°, 1.47°±0.62°, 2.71°±0.47°,3.12°±0.70°, and 2.88°±0.68°, respectively; all differences were statistically significant (P<0.05). However, postoperative day 1 rotation in the capsular bag was <1.5°.
Residual Astigmatism The residual astigmatism of group ART2 and group ReSTOR was -0.18±0.07 D and -0.91±0.25 D.There was a statistically significant reduction of residual astigmatism in group ART2 (F=140.42, P<0.01).
Visual Acuity Comparison Table 1 shows the 3mo postoperative UDVA, uncorrected intermediate visual acuity, and uncorrected near visual acuity. All eyes achieved 20/40 (logMAR 0.3) or better. Visual acuity of group ART2 was significantly better than visual acuity of group ReSTOR (P<0.01). The 3mo postoperative CDVA, corrected intermediate visual acuity, and corrected near visual acuity. Overall DCVA of 94.12% eyes in group ART2 achieved 0.8 or better; the corresponding rate in group ReSTOR was 82.35% (P<0.05).
Optical Quality Parameters Table 2 shows the 3mo postoperative objective optical quality parameters in iTrace measurements. The aMTF and SR values of group ART2 were all superior to group ReSTOR, but the differences were not statistically different (P>0.05).
Spectacle Independence and Patient Satisfaction Table 2 shows subjective spectacle independence and patient satisfaction.At 3mo postoperatively, the rates of subjective spectacle independence in groups ART2 and ReSTOR were 100% and 82.35%, respectively. Only three eyes in group R required glasses for less than one-half day. All patients were satisfied with their postoperative results; however, the indexes of the two groups showed no statistical differences (P>0.05).
DISCUSSION
The focus of this study was the necessity of correcting low corneal astigmatism in multifocal pseudophakic eyes. The advent of ART2 has brought surgeons a safe, accurate, and predictable method to manage the cataract patient who has low corneal astigmatism and wants to achieve better entire visual perception. There was roughly a 0.75-D difference(P<0.05) in postoperative astigmatism between groups ART2 and ReSTOR. Recent researches[8-9] regarding the effects of astigmatism on blurred vision suggest that this would equate to a 1-to-2-line difference in high-contrast visual acuity in monofocal pseudophakic eyes, and worse in multifocal pseudophakic eyes. The challenge with low astigmatism in multifocal pseudophakic eyes is the precision and stabilization with which the astigmatism can be corrected postoperatively.As the study shows, though there is no statistical difference regarding preoperative corneal astigmatism, and all operations were performed by the same veteran surgeon using the same measurements, the postoperative residual astigmatism was significantly different (P<0.05). This is the most important finding in this study. The postoperative astigmatisms of group ART2 and ReSTOR were respectively -0.18±0.07 D and-0.91±0.25 D, and their visual outcomes were statistically different (P<0.05), although the veteran surgeon maintained control of surgery-induced astigmatism (SIA) (<0.3 D),and performed every surgery stably. Success in reducing postoperative astigmatism may lie in the preoperative online calculation for AcrySof IQ ReSTOR Multifocal Toric IOL(www.acrysoftoriccalculator.com) and performing “twice precise” orientation, before and during operation. The “twice precise” orientation has successfully avoided axis rotation caused by eyeball rotation. The formula mode of online calculation has incorporated the effect of SIA, and provides the most precise IOL axis for the surgeon. However, the effect of SIA in group ReSTOR cannot be neutralized.
In addition to the precise calculation, the rotation stability of the ART2 is a crucial focus of this study, which not only relies on the material of IOL, but on the skill of the veteran surgeon.This merit of the rotation stability of ART2 has been verified by many surveys. The 3mo postoperative rotations of ART were 4.18°±1.6° and 3.2°±1.55°, respectively, in the studies by Chen et al[10] and Tan et al[11]. The rotation of ART2 in this study was 3.12°±0.70°, which is very similar to the previous studies. On the basis of rotation stability, ART2 provides better visual outcomes than ReSTOR.
Thus, the roughly 0.75-D difference caused ART2 pseudophakic eyes to achieve more satisfactory visual outcomes than ReSTOR eyes at 3mo postoperatively. One-hundred percent of patients UDVA values were 20/25 or better, 88.23% of patients’ uncorrected intermediate visual acuity values were 20/25 or better, 94.12% of patients’ uncorrected near visual acuity values were 20/25 or better. All patients achieved spectacle independence without discomfort, and the improved visual perception satisfied their daily life. These results are comparable to those of the study by Epitropoulos[12]. Other previous studies have shown that Toric IOLs are more reliable for correcting corneal astigmatism. The postoperative residual astigmatism can be reduced to approximately 0.3 D, and lower astigmatism is associated with a better visual outcome[10,13-16].This verifies that the implantation of ART2 is more effectual than ReSTOR in improving the visual acuity of multifocal pseudophakic eyes.
In addition to the subjective evaluation, aMTF and SR are the objective evaluations in this study. Modulation transfer function refers to contrast changes within any specific optical imaging system. This is a function of spatial frequency,and represents contrast differences under different spatial frequencies, which constitute impacts on the quality of the imaging optical system. aMTF and SR are comprehensive evaluation indexes for visual image quality, and can be influenced by many factors, such as age[17], vitreous opacity[18],retinal function[19], and aberrations[20]. The errors of the former three factors were controlled in advance. Regarding aberration,the eccentricity and tilt of the IOL can produce new aberrations such as astigmatism and coma[21], which affect retinal imaging quality and reduce aMTF, especially in the toric pseudophakic eye. Therefore, consummate surgical skill and IOL stability are especially important. In this study, no IOLs showed obvious tilt and eccentricity, and all postoperative aberrations were<0.1 μm, such that they were insufficient for affecting aMTF and SR. Therefore, there were no statistically significant differences between the groups. These results are consistent with the previous study by Ferreira et al[14].
In summary, the ART2 can provide significantly lower postoperative astigmatism than ReSTOR when the preoperative corneal astigmatism is in the range of 0.5-1.0 D (regular corneal astigmatism of 0.75-1.0 D with-the-rule or 0.5-0.75 D against-the-rule). The mean 0.75 D reduction in postoperative astigmatism is likely to produce significant improvements in patients’ visual acuity and objective evaluations, and is likely to contribute to spectacle independence and patient satisfaction.
ACKNOWLEDGEMENTS
Conflicts of Interest: Hao J, Non e; Tan LZ, None; Li L,None; Bu SC, None; Ren XJ, None; Tian F, None; Zhang H,None.
1 Hayashi K, Manabe S, Yoshida M, Hayashi H. Effect of astigmatism on visual acuity in eyes with a diffractive multifocal intraocular lens. J Cataract Refract Surg 2010;36(8):1323-1329.
2 Mimouni M, Nemet A, Pokroy R, Sela T, Munzer G. The effect of astigmatism axis on visual quality. Eur J Ophthalmol 2017;27(3):308-311.
3 Wolffsohn JS, Bhogal G, Shah S. Effect of uncorrected astigmatism on vision. J Cataract Refract Surg 2011;37(3):454-460.
4 Gauthier L, Lafuma A, Laurendeau C, Berdeaux G. Neodymium: YAG laser rates after bilateral implantation of hydrophobic or hydrophilic multifocal intraocular lenses: twenty-four month retrospective comparative study. J Cataract Refract Surg 2010;36(7):1195-1200.
5 Guo T, Gao P, Fang L, Guo L, Fan Y, Liu C. Efficacy of toric intraocular lens implantation in eyes with high myopia: a prospective, case-controlled observational study. Exp Ther Med 2018;15(6):5288-5294.
6 Alfonso JF, Fernandez-Vega L, Puchades C, Montes-Mico R.Intermediate visual function with different multifocal intraocular lens models. J Cataract Refract Surg 2010;36(5):733-739.
7 Hayashi K, Manabe S, Hayashi H. Visual acuity from far to near and contrast sensitivity in eyes with a diffractive multifocal intraocular lens with a low addition power. J Cataract Refract Surg 2009;35(12):2070-2076.
8 Statham M, Apel A, Stephensen D. Comparison of the AcrySof SA60 spherical intraocular lens and the AcrySof Toric SN60T3 intraocular lens outcomes in patients with low amounts of corneal astigmatism. Clin Exp Ophthalmol 2009;37(8):775-779.
9 Ernest P, Potvin R. Effects of preoperative corneal astigmatism orientation on results with a low-cylinder-power toric intraocular lens. J Cataract Refract Surg 2011;37(4):727-732.
10 Chen XF, Lu Y, Duan XY, Shi YH, Yu H, Chen Y, Huang ZP. Effects of AcrySof IQ ReSTOR Toric intraocular lens implantation on visual quality.Rec Adv Ophthalmol 2014;34(4):337-340.
11 Tan LZ, Zhang H, Tian F, Mu JW. Clinical study of optical quality after aspheric multifocal toric intraocular lens implantation. Rec Adv Ophthalmol 2015;35(9):861-865.
12 Epitropoulos AT. Visual and refractive outcomes of a toric presbyopiacorrecting intraocular lens. J Ophthalmol 2016;2016:7458210.
13 Vale C, Menezes C, Firmino-Machado J, Rodrigues P, Lume M,Tenedório P, Menéres P, Brochado Mdo C. Astigmatism management in cataract surgery with Precizon (®) toric intraocular lens: a prospective study. Clin Ophthalmol 2016;10:151-159.
14 Ferreira TB, Marques EF, Rodrigues A, Montes-Mico R. Visual and optical outcomes of a diffractive multifocal toric intraocular lens. J Cataract Refract Surg 2013;39(7):1029-1035.
15 Alfonso JF, Knorz M, Fernandez-Vega L, Rincon JL, Suarez E,Titke C, Kohnen T. Clinical outcomes after bilateral implantation of an apodized +3.0 D toric diffractive multifocal intraocular lens. J Cataract Refract Surg 2014;40(1):51-59.
16 Pesala V, Garg P, Bharadwaj SR. Image quality analysis of pseudophakic eyes with uncorrected astigmatism. Optom Vis Sci 2014;91(4):444-451.
17 Kamiya K, Umeda K, Kobashi H, Shimizu K, Kawamorita T, Uozato H. Effect of aging on optical quality and intraocular scattering using the double-pass instrument. Curr Eye Res 2012;37(10):884-888.
18 Kobayashi K, Shibutani M, Takeuchi G, Ohnuma K, Miyake Y,Negishi K, Ohno K, Noda T. Calculation of ocular single-pass modulation transfer function and retinal image simulation from measurements of the polarized double-pass ocular point spread function. J Biomed Opt 2004;9(1):154-161.
19 Montes-Mico R, Alio JL, Charman WN. Postblink changes in the ocular modulation transfer function measured by a double-pass method.Invest Ophthalmol Vis Sci 2005;46(12):4468-4473.
20 Santhiago MR, Netto MV, Barreto J Jr, Gomes BA, Oliveira CD, Kara-Junior N. Optical quality in eyes implanted with aspheric and spherical intraocular lenses assessed by NIDEK OPD-Scan: a randomized, bilateral,clinical trial. J Refract Surg 2011;27(4):287-292.
21 Pieh S, Fiala W, Malz A, Stork W. In vitro strehl ratios with spherical, aberration-free, average, and customized spherical aberration-correcting intraocular lenses. Invest Ophthalmol Vis Sci 2009;50(3):1264-1270.