INTRODUCTION
As the second leading reason of blindness, glaucoma is a chronic, progressive, and irreversible optic neuropathy,such that the long-term intraocular pressure (IOP) control without complications is greatly significant in glaucoma patients, especially young patients[1-2]. In 1999, Professor Stegmann performed the first operation of viscocanalostomy[3].It is one of the non-penetrating glaucoma surgeries. During the procedure, after dissection of the superficial and deep scleral flaps, Schlemm’s canal (SC) was unroofed. A microcannula was introduced into either side of the surgically created ostium,and viscoelastic substance was repeatedly injected to dilate SC. Viscocanalostomy is intended to restore physiological drainage Three modifications were made for the first time in this study for the purpose of further IOP reduction. The surgeon peeled the inner wall of SC and the juxtacanalicular meshwork in order to decrease the permeation resistance of the aqueous humor from the anterior chamber to the scleral lake.Mitomycin C (MMC) was used to decrease the scar under the superficial scleral flap and under the conjunctiva. Moreover,the superficial flap was closed loosely with 2 sutures instead of being sutured in a watertight manner for the purpose of adding subconjunctival filtration.
Up to now, several studies reported the effect of viscocanalostomy for <5y[3-5]. Also, the long-term results of viscocanalostomy were reported only in African and European patients[1]. To the best of our knowledge, the data of the Asian population was not published yet. Thus, the present retrospective research was aimed at studying the efficacy and safety of modified viscocanalostomy in Chinese population with open angle glaucoma (OAG) over a period of 10y.
SUBJECTS AND METHODS
Ethical Approval The data of patients with OAG, who underwent viscocanalostomy between March 2004 and December 2009 at the First Affiliated Hospital of Nanjing Medical University, were obtained from the medical records.All the patients were Chinese population. The research followed the tenets of the Declaration of Helsinki and was approved by the Ethics Committee of the First Affiliated Hospital of Nanjing Medical University (No.2018-SR-084).Oral informed consent was obtained from all the subjects. The participants didn’t receive a stipend.
Patients Selection Prior to viscocanalostomy, the following examinations were conducted: the best-corrected visual acuity(BCVA) by Snellen chart at 5 meters, slit-lamp examination,fundoscopy, Goldmann applanation tonometry, gonioscopy,and Humphrey perimetry. The indication for surgery was IOP>21 mm Hg with at least 2 kinds of anti-glaucoma eye drops, progressive glaucomatous optic nerve damage and characteristic visual field loss. The patients had open anterior chamber angle. A total of 148 viscocanalostomies were carried out on 148 eyes from 148 patients; those with secondary glaucoma (n=13) and congenital glaucoma (n=17) were excluded. Any eye which undergone glaucoma or cataract surgery before (n=4) were excluded. Moreover, patients with combined surgeries (n=5) with cataract extraction were also excluded. Thus, 109 eyes of 109 patients were included in the study.
Surgical Procedure The surgical procedures were based on Stegmann’s procedure[3]. In order to protect the epi-scleral collector channels, hemostasis cautery was strictly avoided. A gelatin sponge was used to absorb bleeding. The modifications were then performed as described by Yuan et al[6] as follows:MMC was applied followed by peeling the inner wall of SC and the juxtacanalicular trabecular meshwork, finally the superficial scleral flap was loosely sutured.

Figure 1 Surgical details showed the steps of surgical procedures of modified viscocanalostomy A: Demonstration of the superficial and deep scleral flaps; B: Injection of the viscoelastic material into the SC using a microcannula; C: Passing of the viscoelastic material through the epi-scleral veins; D: Removal of the inner wall of SC and the juxta-canalicular trabecular meshwork.
All the surgeries were performed by the same surgeon. Under local anesthesia using 0.75% ropivacaine, 8-0 Vicryl® (Ethilon Inc., Somerville, NJ, USA) was used for corneal traction near the superior limbus. A fornix-based conjunctival flap extending from 11 to 1 o’clock was made. Then, a 5×4 mm2 parabolicshaped, one-third thickness superficial scleral flap was dissected. Cotton pieces with MMC at a dose of 0.3 mg/mL were used under the conjunctiva as well as the superficial scleral flap for 3min. Cotton pieces were removed and the procedure site was washed with 20 mL saline. Next, a two-thirds thickness deep scleral flap, 0.5 mm inside the border of the superficial scleral flap, was fashioned to leave a thin translucent layer of sclera overlying the choroid. And the SC was unroofed (Figure 1A). After the deep flap was cut off, the viscoelastic substance(Healon GV®, AMO, Uppsala, Sweden) was injected into both sides of the surgically created ostia with a microcannula(diameter of 230 μm) repeatedly for 5 times (Figure 1B). The viscoelastic substance was injected into the epi-scleral veins,which in turn became white in color after injection (Figure 1C).Using the self-designed tweezers (flat end with diameter of 250 μm), the inner wall of SC and juxta-canalicular trabecular meshwork were removed (Figure 1D). Anterior chamber paracentesis was performed before SC peeling in order to deal with any possible risk of iris prolapse. Then, the trabeculo-Descemet’s membrane (TDM) was left intact. The superficial scleral flap was closed loosely with 2 sutures of 10-0 nylon.The viscoelastic substance was injected under the superficial scleral flap for the sake of maintaining an adequate scleral lake. Lastly, the conjunctiva flap was sutured with 10-0 nylon sutures. Tobramycin dexamethasone and pilocarpine eye drops were used during the first 3d post-surgery, and pranoprofen eye drop was prescribed for the subsequent 4wk.
Patients’ Follow-up All patients were clinically followed up at day 1, the first week, then after the first, third, sixth and ninth month, and then at one year postoperatively, after which the patients were followed up annually for a 10-year period.The examinations included BCVA, slit-lamp examination,fundoscopy, Goldmann applanation tonometry, and Humphrey perimetry. The surgical site was scanned by ultrasound biomicroscopy (UBM) for some cases 3mo postoperatively.The definition of complete success was an IOP 21, 18, 16 mm Hg or less without anti-glaucoma medications, respectively.Qualified success was defined as an IOP 21, 18, 16 mm Hg or less with or without anti-glaucoma medications, respectively[7].In cases where IOP was above 21 mm Hg, an Nd:YAG laser goniopuncture (LGP; Carl Zeiss Meditec AG, Germany) was performed using a gonioscopy contact lens (Ocular Latina SLT Gonio Laser, Bellevue, Washington, USA). Free running Q-switch mode was selected with energy ranging from 2-4 mJ.Four to ten shots were aimed at the TDM, creating a hole in the TDM and allowing direct passage of aqueous humor from anterior chamber to the scleral lake. The application of LGP was not deemed as a failure. Success of LGP was defined when IOP was equal to or lower than 21 mm Hg without anti-glaucoma medications. Anti-glaucoma eye drops were prescribed if IOP was still above 21 mm Hg after LGP. When the IOP was above 21 mm Hg and could not be controlled by both LGP and anti-glaucoma medications, the surgery was considered a failure.
Statistical Analysis The data were analyzed by statistical analysis system (SAS) version 9.4 (SAS Institute, Cary,NC, USA). Paired-samples t-test was used to determine the significance of any differences in the continuous variables within each group. P<0.05 was defined as statistically significant. Kaplan-Meier survival curve was used to derive the cumulative probability of success. Moreover, Cox regression model was selected to study the association of success rate and demographic factors, including preoperative IOP, age at surgery, gender, and number of anti-glaucoma medications.
RESULTS
In this study, a total of 109 eyes of 109 patients were included.The medical data of 9 patients was lost or incomplete. The data of 100 eyes of 100 patients with mild to severe glaucoma was collected. The preoperative data are summarized in Table 1.The patients were followed up for 104.5±37.0mo (range 96-132mo). The median number was 108mo.
The preoperative and postoperative IOP is shown in Figure 2 and Table 2, which indicates the IOP variation before and after modified viscocanalostomy. Figure 3 shows a scatter plot representation of the postoperative IOP at 5y versus the preoperative IOP. The mean preoperative IOP was 33.5±9.9 mm Hg. At 1, 3 and 6mo postoperatively, the mean IOP was 12.5±4.3, 13.3±3.7 and 14.2±4.2 mm Hg, respectively.And the mean IOP was 15.2±3.6 mm Hg (mean IOP reduction of 51%) and 15.6±2.8 mm Hg (mean IOP reduction of 49.9%)at 5y and 10y after modified viscocanalostomy, respectively(P<0.001). Furthermore, the mean time to start using antiglaucoma eye drops was 51.0±47.5mo postoperatively whenIOP was above 21 mm Hg and could not be controlled by LGP.The complete and qualified success rate of modified viscocanalostomy is listed in Table 3. The number of anti-glaucoma eye medications dropped from 2.39±0.5 preoperatively to 0.47±0.8 and 0.67±0.8 at 5y and 10y postoperatively (Table 2,P<0.001). In addition, 85 eyes (85%) of 85 patients could control IOP with one or less anti-glaucoma eye drop. Figure 4 indicates the Kaplan-Meier survival curves of qualified success rates with an IOP 21, 18 and 16 mm Hg or less, respectively.Figure 5A further illustrates UBM images of the surgical site with adequate IOP control without medications. Figure 5B exhibits the hole in the TDM after LGP, which in turn increased the drainage of aqueous humor into the scleral lake.Figure 5C shows the surgical site of a failed procedure with a collapsed scleral lake.
Table 1 Preoperative data

SD: Standard deviation; IOP: Intraocular pressure; c/d: Cup/disc.
?
Table 2 Preoperative and postoperative IOP and number of medications
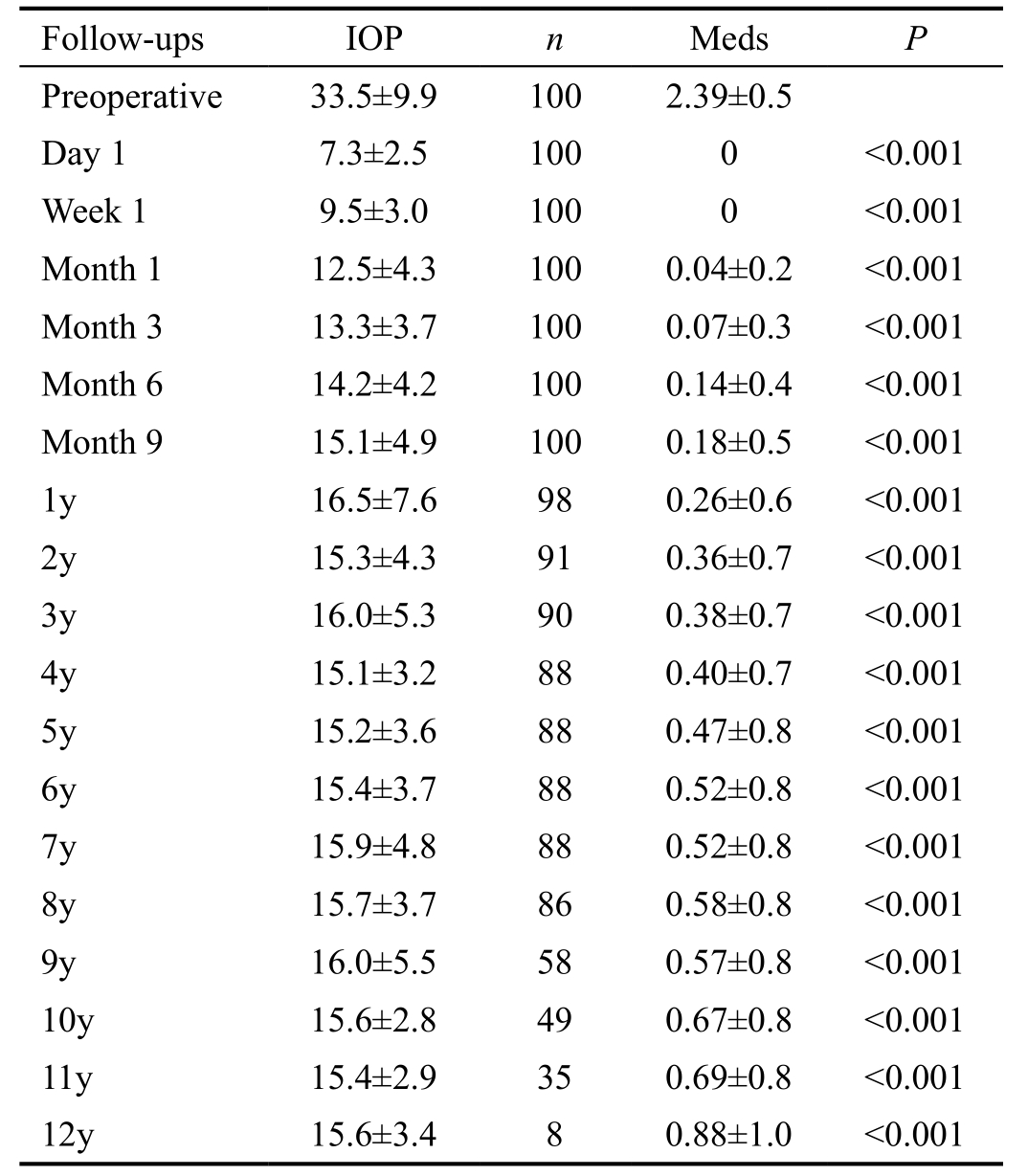
Paired-samples t-test. IOP: Intraocular pressure; Meds: Number of medications; n: Number of patients.
?

Figure 2 Mean preoperative and postoperative IOP; bars indicate the standard error of the mean.

Figure 3 Scatterplot of IOP preoperatively and 5y postoperatively.

Figure 4 Kaplan-Meier analysis of the qualified success.
According to the Cox regression analysis of the complete and qualified success rate (IOP≤21 mm Hg), age and preoperativeIOP were statistically significant. Age had a negative coefficient [hazard ratio 0.97, 95% confidence interval (CI):0.96-0.99, P=0.001], while preoperative IOP had positive beta coefficients (hazard ratio 1, 95%CI: 1-1, P=0.035). Thus, being younger was associated with lower successful rates, whereas higher preoperative IOP was associated with poorer successful rates. For the success rate of IOP≤18 mm Hg, age (hazard ratio 0.98, 95%CI: 0.96-0.99, P=0.007) and preoperative IOP(hazard ratio 1, 95%CI: 1-1.1, P=0.004) affected the complete success rate significantly. Only preoperative IOP affected the qualified success rate significantly (hazard ratio 1, 95%CI:1-1.1, P=0.003). For the success rate of IOP≤16 mm Hg, only age significantly affected the complete success rate (hazard ratio 0.98, 95%CI: 0.96-0.99, P=0.003).
Table 3 Complete and qualified success rate for an IOP of 21, 18 and 16 mm Hg or less (95%CI)

IOP: Intraocular pressure; CI: Confidence interval.
Characteristic 21 mm Hg 18 mm Hg 16 mm Hg 5y Complete 0.59 (0.49-0.69) 0.52 (0.41-0.63) 0.42 (0.31-0.54)Qualified 0.84 (0.80-0.88) 0.73 (0.68-0.78) 0.59 (0.52-0.66)10y Complete 0.43 (0.33-0.53) 0.37 (0.26-0.48) 0.28 (0.17-0.40)Qualified 0.80 (0.76-0.84) 0.69 (0.64-0.74) 0.51 (0.44-0.58)
LGP was performed in 31 eyes (31.3%) of 31 patients,decreasing IOP from 22.9±4.3 mm Hg to 16.3±2.5 mm Hg(P<0.01). The mean time of LGP was 18.0±23.2mo after modified viscocanalostomy. The success rate of LGP was 88%.BCVA decreased from 0.72±0.29 preoperatively to 0.61±0.27 on the first day postoperatively. Visual acuity recovered 1wk postoperatively and remained stable at 5y (0.69±0.30) and 10y(0.65±0.32) postoperatively.
From the perspective of complications, any blebitis, shallow anterior chamber, choroidal detachment or endophthalmitis were not observed. Three eyes (3.1%) of 3 patients had complications, including 2 cases of anterior chamber angle hemorrhage and 1 case of TDM rupture because of trauma,surgical site iris incarceration and eventually raised IOP due to trauma.
DISCUSSION

Figure 5 Postoperative scans of UBM A: UBM image of surgery domain with IOP of 13.7 mm Hg at 10y after viscocanalostomy. The scleral lake and the TDM are clear; B: UMB image of surgery domain after laser goniopuncture treatment. A hole in the TDM was observed; C: UMB image of surgery domain after a failed procedure. The scleral lake collapsed.
Viscocanalostomy effectuated stable IOP reduction in primary open angle glaucoma (POAG) patients. In 1999,Professor Stegmann reported the efficiency and safety of viscocanalostomy for 214 eyes with OAG[3]. The qualified success rate was 89% (IOP≤22 mm Hg with or without medications) while the complete success rate was 82.7%(IOP≤22 mm Hg without medications) with a mean follow-up of 35mo[3]. From that time on, the ophthalmologists initiated many studies on viscocanalostomy; however, the success rate was variable[8-9]. After 16y, based on a multi-center research trial, Stegmann published the long-term results of up to 12y of >700 cases of viscocanalostomy with OAG[10], based on a multi-center research. Up to the present time, it is considered as the most significant research with a large number of patients and with the longest follow-up period. The qualified success rate (IOP≤21 mm Hg with or without anti-glaucoma drops) at 5y was 92% (95%CI: 0.88-0.96) in European patients and 90%(95%CI: 0.87-0.93) in African patients. At 10y, the qualified success rate was 90% (95%CI: 0.88-0.95) and 74% (95%CI:0.69-0.80) in European and African patients, respectively[11]. In the current study, the qualified success rate (IOP≤21 mm Hg with or without anti-glaucoma drops) was 84% (95%CI: 0.80-0.88) at 5y and 80% (95%CI: 0.76-0.84) at 10y in Chinese patients. This is basically in line with Stegmann’s study[10].Although the success rate in the current study was a little bit lower at 5y postoperatively, the patients were much younger(43.7-year-old) than those in Stegmann’s study (57.9-yearold)[10]. Moreover, the present study showed that age affected the qualified success significantly (hazard ratio 0.97, 95%CI 0.96-0.99, P=0.001). Being younger was associated with lower successful rates. Young age is always a challenge for glaucoma management. Young patients had strong repair ability leading to scar in the viscocanalostomy target site, which decreased the drainage of aqueous humor. Thus, this retrospective study showed a little bit lower success rate compared with Professor Stegmann’s study[10]. Another 12-year follow-up study showed a lower overall success rate of 62.5% and lower complete success rate of 12.5% compared with the present study[11]. As far as the number of anti-glaucoma drops was of concern, it dropped from 2.39±0.5 preoperatively to 0.47±0.8 and 0.67±0.8 at 5y and 10y postoperatively (P<0.001). Up to 85 eyes (85%) of 85 patients could control IOP with one or less anti-glaucoma eye drops, which had helped to relieve the burden of the patient.
The surgeon modified viscocanalostomy. According to Stegmann’s procedure, the superficial scleral flap was sutured in a watertight manner[3] and MMC was forbidden to avoid filtering blebs. The aim of this procedure was to facilitate the aqueous humor drainage through the physiological path instead of the subconjunctival route. Nevertheless, in the current procedure, the superficial flap was sutured loosely with only 2 sutures and MMC was used to reduce subconjunctival and scleral lake scars. In this study, the surgeon expected subconjunctival outflow in addition to physiological path induced by the viscocanalostomy. Moreover, the inner wall and the juxtacanalicular trabecular meshwork were peeled to decrease the resistance of the aqueous humor diffusing from the anterior chamber to the scleral lake. This modification was the most sophisticated part of the surgery. The TDM was so thin that it was very liable to perforate into the anterior chamber, leading to the failure of the surgery. In another study, we combined viscocanalostomy with trabeculotomy for the treatment of primary congenital glaucoma[12], because it was easy to locate SC which was the most difficult part of trabeculotomy[13]. The 25 G syringe needle (1 mL syringe, BD,USA) was bended and used to initiate the peeling. Then the self-designed tweezers was applied to strip the inner wall of the SC. After the removal of it, more aqueous humor diffused through the TDM out of the eye ball.
After aqueous humor penetrates through the TDM to the scleral lake, it passages by several ways; some travels into the ostium of SC and the distal outflow system, some is absorbed by the new aqueous humor veins on the sclera, some travels by the subconjunctival path, and the remaining goes through the uveoscleral outflow[14]. At 1, 3 and 6mo after the operation,the mean IOP was 12.5±4.3, 13.3±3.7 and 14.2±4.2 mm Hg,respectively. Compared with Professor Stegmann’s study[10],the current study of modified viscocanalostomy got lower IOP within 6mo. The reason of lower IOP control in the early period after the surgery was due to peeling of the SC inner wall and subconjunctival filtration path.
Furthermore, only a few studies reported the long-term efficacy and safety of viscocanalostomy over a period of 5y[9,11,15-17]. A majority of the data mentioned above were reported in African and European patients. As due to the best of our knowledge, no data was available in the literature regarding a long-term study in the Asian population. The current study applied a 10-year follow-up result of modified viscocanalostomy in the Chinese population. The worldwide prevalence of glaucoma is 3.54%[2]. Africa has the highest prevalence of POAG, while Asia is highest in primary angle closure glaucoma. Males and urban population were likely to have POAG, which was in accordance with the results of the current study[1]. Of 77% of the patients included were male.Furthermore, gender, preoperative IOP, and age were analyzed.Very few studies showed positive results of correlation[10-11,18].While in the current study, the Cox regression model of the complete and qualified success rate (IOP≤21 mm Hg) showed that age and preoperative IOP were statistically significant.Age had a negative coefficient (hazard ratio 0.97, 95%CI:0.96-0.99, P=0.001), while preoperative IOP had positive beta coefficients (hazard ratio 1, 95%CI: 1-1, P=0.035). Thus, being younger was associated with lower successful rates, whereas higher preoperative IOP was associated with poorer successful rates. Scarring was recognized as the primary cause of failure in antiglaucoma surgery. The younger the age, more obvious the failure. Since the mean age was much younger (43.7-yearold vs 57.9-year-old), our study showed a little bit lower success rate than that by Stegmann’s study[10].
LGP is recognized as an effective safe supplemental procedure to viscocanalostomy, increasing the success rate of viscocanalostomy[19]. The aqueous humor penetrates through TDM, which is reduced with the passage of time[20]. If IOP was >21 mm Hg, LGP was performed using the Nd:YAG laser leading to the micro-perforation of TDM. Thus, excessive aqueous humor was drained through TDM and then absorbed by different means. The proportion and success rates of LGP vary from study to study[20-21]. LGP was performed in 31 eyes(31.3%) of 31 patients in the present study, decreasing IOP from 22.9±4.3 mm Hg to 16.3±2.5 mm Hg (P<0.01). The mean time was 18.0±23.2mo after viscocanalostomy.
The data on visual acuity was also recorded. According to the clinical experience, viscocanalostomy did not affect the visual acuity as the non-penetrating procedure could circumvent the sharp IOP drop and brought less astigmatism[22]. BCVA decreased from 0.72±0.29 preoperatively to 0.61±0.27 on the first day postoperatively, and recovered 1wk postoperatively.The transient impaired vision early after the operation was also reported by Shaarawy et al[15]. We didn’t got the exact reason for the vison loss.
Safety is a distinct advantage of viscocanalostomy as compared to trabeculectomy[4]. As a non-penetrating glaucoma surgery,viscocanalostomy procedure does not penetrate into the eye.Thus, it avoids many severe complications such as shallow anterior chamber, choroidal detachment, cataract, blebitis,endophthalmitis and so on. Totally 3.1% patients exhibited complications, including 2 with anterior chamber angle hemorrhage and 1 with TDM perforation and iris prolapse due to trauma as mentioned previously. Microhypema occurred during Healon GV injection and SC expansion. The inner wall of SC was disrupted, and the epi-scleral blood refluxed into the anterior chamber. Microhypema was absorbed in 2d. Viscocanalostomy could avoid complications of shallow anterior chamber, cataract, bleb leakage, and endophthalmitis,which often occurred in trabeculectomy. These complications could impair the visual function. Thus, viscocanalostomy was suitable for OAG patients especially young patients with a long duration of life.
Nevertheless, the present retrospective study had some limitations. First, there was a selection bias, as the study was limited by data availability as well as loss of follow-up.The other was Humphrey perimetry which was not included and analyzed. Perimetry was difficult to follow-up due to the prolonged duration of the study and neglection of visual functions examinations in the past, and particularly, advanced stage and end stage glaucoma patients who could not perform visual field examination, which needed visual acuity and optimal cooperation.
In summary, modified viscocanalostomy effectuated stable IOP reduction in Chinese patients with OAG; age and preoperative IOP affected the success rate significantly; rare complications occurred as compared to trabeculectomy. Despite the learning curve, the technique is promising in developing countries as a cost-effective minimally invasive glaucoma surgery.
ACKNOWLEDGEMENTS
We thank Prof. Jian-Ling Bai from Nanjing Medical University for technical support. We also thank all recruited patients for their participation in this study.
Conflicts of Interest: Liang Y, None; Sun H, None; Shuai J,None; Xu K, None; Ji FF, None; Sucijanti, None; Yuan ZL,None.
1 Chan EW, Li X, Tham YC, Liao J, Wong TY, Aung T, Cheng CY.Glaucoma in Asia: regional prevalence variations and future projections.Br J Ophthalmol 2016;100(1):78-85.
2 Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY.Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology 2014;121(11):2081-2090.
3 Stegmann R, Pienaar A, Miller D. Viscocanalostomy for openangle glaucoma in black African patients. J Cataract Refract Surg 1999;25(3):316-322.
4 Moradian K, Daneshvar R, Saffarian L, Esmaeeli H, Hosseinnezhad H.The efficacy of viscocanalostomy for uncontrollable primary open-angle glaucoma in a developing country. Indian J Ophthalmol 2013;61(2):71-73.
5 Zong Y, Yuan ZL. Recent advances in viscocanalostomy for primary open-angle glaucoma. Zhonghua Yan Ke Za Zhi 2013;49(8):749-751.
6 Yuan ZL, Yang Q, Chen Q, Zhang WZ, Sun H. Modified viscocanalostomy for the surgical treatment with primary open angle glaucoma. Zhonghua Yan Ke Za Zhi 2007;43(5):421-425.
7 Heuer DK, Barton K, Grehn F, Shaarawy T, Sherwood M. Consensus on definition of success. Guidelines on design and reporting of glaucoma surgical trials. Amsterdam: Kluger Publications;2009:15-24.
8 Taubenslag KJ, Kammer JA. Outcomes disparities between black and white populations in the surgical management of glaucoma. Semin Ophthalmol 2016;31(4):385-393.
9 Faulkner W. Seven year follow-up of combined cataract extraction and viscocanalostomy. J Cataract Refract Surg 2007;33(6):940-941.
10 Grieshaber MC, Peckar C, Pienaar A, Koerber N, Stegmann R. Longterm results of up to 12 years of over 700 cases of viscocanalostomy for open-angle glaucoma. Acta Ophthalmol 2015;93(4):362-367.
11 Gunenc U, Ozturk T, Arikan G, Kocak N. Long-term results of viscocanalostomy and phacoviscocanalostomy: a twelve-year follow-up study. Int J Ophthalmol 2015;8(6):1162-1167.
12 Qian CX, Zong Y, Chen Q, Yuan ZL. Viscocanalostomy combined with trabeculotomy and mitomycin C in the treatment of primary congenital glaucoma. Int J Ophthalmol 2017;10(6):919-924.
13 Tan YL, Chua J, Ho CL. Updates on the surgical management of pediatric glaucoma. Asia Pac J Ophthalmol (Phila) 2016;5(1):85-92.
14 Grieshaber MC. Viscocanalostomy and canaloplasty: ab externo schlemm’s canal surgery. Dev Ophthalmol 2017;59:113-126.
15 Shaarawy T, Nguyen C, Schnyder C, Mermoud A. Five year results of viscocanalostomy. Br J Ophthalmol 2003;87(4):441-445.
16 David VP, Kutty KG, Somasundaram N, Varghese AM. Five-year results of viscocanalostomy. Eur J Ophthalmol 2008;18(3):417-422.
17 Wishart PK, Wishart MS, Choudhary A, Grierson I. Long-term results of viscocanalostomy in pseudoexfoliative and primary open angle glaucoma. Clin Exp Ophthalmol 2008;36(2):148-155.
18 Aslan F, Yuce B, Oztas Z, Ates H. Evaluation of the learning curve of non-penetrating glaucoma surgery. Int Ophthalmol 2018;38(5):2005-2012.
19 Mathews D, Shirodkar AL, Ahnood D, Garrick A. Outcomes of Nd:YAG goniopuncture after Viscocanalostomy/Phacoviscocanalostomy.J Glaucoma 2016;25(6):e562-e568.
20 Al Obeidan SA. Incidence, efficacy and safety of YAG laser goniopuncture following nonpenetrating deep sclerectomy at a university hospital in Riyadh, Saudi Arabia. Saudi J Ophthalmol 2015;29(2):95-102.
21 Di Matteo F, Bettin P, Fiori M, Ciampi C, Rabiolo A, Bandello F. Nd:YAG laser goniopuncture for deep sclerectomy: efficacy and outcomes.Graefes Arch Clin Exp Ophthalmol 2016;254(3):535-539.
22 Egrilmez S, Ates H, Nalcaci S, Andac K, Yagci A. Surgically induced corneal refractive change following glaucoma surgery: nonpenetrating trabecular surgeries versus trabeculectomy. J Cataract Refract Surg 2004;30(6):1232-1239.