INTRODUCTION
M acular hole (MH) is a reversible cause of decreased vision within the elderly population, arises from adhesion in the vitreomacular interface and can theoretically be treated by vitrectomy. MH surgery was first described in 1991 by Kelly and Wendel[1]. Since the advent of microincision vitrectomy, MH surgery has been performed with minimal invasiveness, and significant visual improvement is a common outcome[2].
Visual field defect (VFD) has been a well-recognized complication of pars plana vitrectomy for MH since it was first documented in 1995 by Melberg and Thomas[3]. Since then,many studies have been conducted on this complication and its mechanism. MH surgery can cause either peripheral or central visual field defect (cVFD) in patients. Although the incidence of peripheral VFD after MH surgery has been reduced by developments in surgical techniques and a series of research studies on the underlying pathogenesis of this condition[4],there have been no specific research studies focussing upon cVFD after MH surgery.
As a predictor of functional outcome for doctors, Garweg et al[5] stated that the central visual field might represent a more sensitive indicator than visual acuity (VA) and reading vision. For MH patients, cVFD can cause profound effects upon health-related quality of life, both in terms of professional and personal activities. For example, Desapriya reported that cVFD is potentially harmful to drivers with even a mild condition[6]. Apart from driving, cVFD can impair a person’s perception of their surroundings and also their participation in hobbies such as reading and sports[7]. Over recent years, cVFD has been extensively investigated in relation to glaucoma,optic disc drusen, retinitis pigmentosa and even occipital lobe lesions[8-11]. However, the precise pathogenesis of cVFD after MH surgery still remains unclear[8-11].
In the present study, we investigated 18 full-thickness patients,with or without cVFD, after MH surgery and considered the possible causes.
SUBJECTS AND METHODS
Ethical Approval This study was approved by the institutional review board of Tianjin Medical University General Hospital and was performed according to the tenets of the 1989 Declaration of Helsinki. Informed consents were obtained from all participants.
Patients A total of 47 eyes from 47 consecutive patients undergoing surgery for MH between January 2016 and January 2018 were prospectively evaluated. After follow-up at policlinic, only 18 eyes from 18 full-thickness patients in which MH had been closed after surgery were selected for inclusion in this study. Exclusion criteria were as follows.First, patients with a final VA less than 0.1 were excluded due to the reliability and reproducibility of perimetry results.Second, patients with a follow-up period of less than six months were excluded in order to achieve relatively stable visual performance. Third, after perimetry, patients whose reliability factor value was over 15 were excluded to increase the reliability of our data. Fourth, after optical coherence tomography (OCT) measurements, patients whose OCT image quality score was less than two were excluded. Fifth,patients with post-traumatic holes, optic and visual pathway diseases, glaucoma, vascular occlusion, diabetic retinopathy or retinal detachments were also excluded. We believed that these underlying pathologies would contribute to VFD that would make the interpretation of our results more difficult[12]. Sixth,lamella macular hole (LMH) cases were excluded. Although the presence of preoperative ellipsoid zone disruption could predict poor outcome after LMH surgery[13], the sizes of preoperative and postoperative ellipsoid zone disruption in the eyes of patients with LMH in our study were all zero. This disruption condition does not represent the real disease entity in LMH.
Stage I MH sometimes shows spontaneous closure during physiological posterior vitreous detachment. Hence, such patients can be followed-up by close observation unless distortion or visual impairment is too severe for patients to tolerate. Stage II, or higher full-thickness MH, are good indications for surgical intervention[1]. Prior to surgery, each MH was graded using the classification proposed by Gass[14].
Surgical Procedures Operations were performed by a single surgeon (Yan H) using the following protocol. In brief, a standard 23-gauge 3-port pars plana vitrectomy was performed.Following core vitrectomy, triamcinolone acetonide was injected into the vitreous and the posterior vitreous cortex was removed. The posterior vitreous was then separated from the retina at the optic disc by inhalation if it was still attached; we did use dissection. The internal limiting membrane was then stained by indocyanine green (ICG). For these patients, ICG solution was constituted by dissolving 25 mg ICG in 3.0 mL of sterile water; 0.1 mL of the ICG solution was then injected directly over the posterior pole using a 27-gauge blunt needle.After 90s, the ICG solution was removed by inhalation with a vitreous cutter. Internal limiting membrane was then grasped and peeled off circularly for 1.5 to 2 disc diameters using a microvitreoretinal blade and Tano forceps (Synergetics, St.Charles, MO, USA). A flute needle was then used to clear away dye from other parts of the stained retina. Air-fluid exchange was then carried out under an air pressure of 35-40 mm Hg over 1-2min, followed by an exchange with sterile normal air. The patients were instructed to maintain a facedown position for three days.
Measurements Static perimetry postoperative and OCT were performed preoperatively and postoperatively in all patients.Square root of loss variance (sLV) and mean defect (MD)were used to evaluate cVFD. Macular hole minimum diameter(MHMD) and macular hole base diameter (MHBD) were used to evaluate MH size. The primary outcome measurements were sLV and MD using the OCTOPUS M standard white/white/top program with 1° spacing in the fovea (central 4°; OCTOPUS 900, SN 3425), along with MH size and postoperative ellipsoid zone disruption of the macular cube 512×128 (SD-OCT,CIRRUS 4000, Carl Zeiss Meditec, Germany). MHMD and MHBD, as well as the extent of ellipsoid zone disruption, were determined as a mean of the sizes measured from the horizontal and vertical cuts. Data from the postoperative perimetry and OCT were collected at the 6mo follow-up time point. One technician assessed the performance of measurements in order to prevent errors and maintain reproducibility. Standard postoperative examinations were also performed.
Statistical Analysis Data are presented as means±standard error of the mean. Correlations between VFD and other parameters, including MH stage and MH size, as well as postoperative ellipsoid zone disruption, were estimated by Spearman’s ranked correlation and linear regression.Comparisons of VFD parameters or postoperative ellipsoid zone disruption among different MH stages were performed using the Kruskal-Wallis test. Dunn’s test was used to compare VFD parameters, or postoperative ellipsoid zone disruption,between the different levels of each MH stage. Data were analyzed with the Statistical Package for Social Science(version 21.0; SPSS, Chicago, USA). P values <0.05 were considered to be statistically significant.
RESULTS
A total of 18 patients (18 eyes; nine right eyes and 9 left eyes) were involved in this study: ten females and 8 males.The mean age was 68.17±5.90y. For each patient, the followup appointment took place 6mo after surgery. Ten of these patients had systemic disease; the remainder did not. There were 3 stage II, 7 stage III, and 8 stage IV full-thickness MHs in this retrospective study. Basic patient data is given in Table 1.Typical cases of perimetry and OCT are shown in Figure 1.
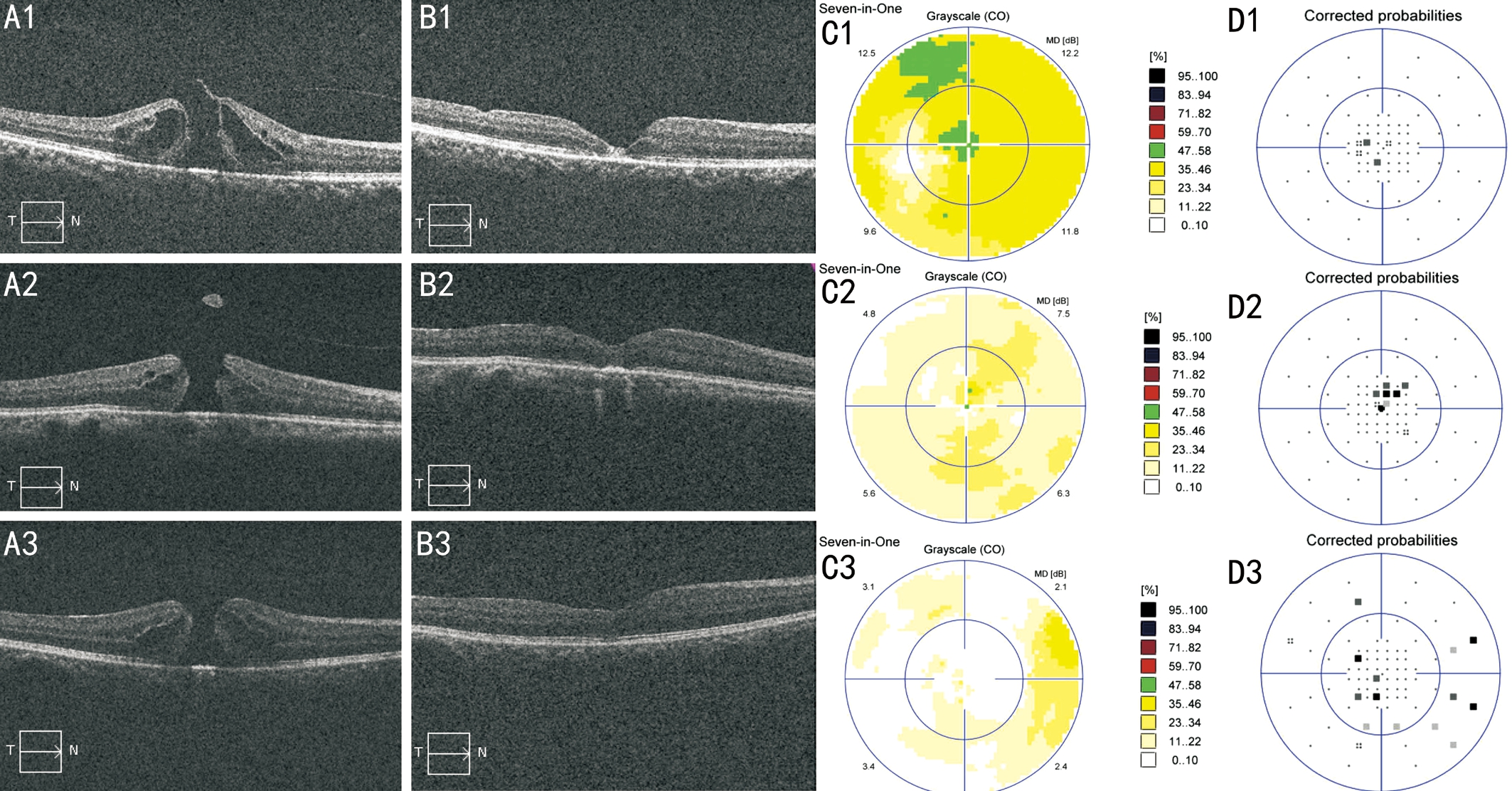
Figure 1 OCT examinations and perimetry of typical cases A: Preoperative OCT examination; B: Postoperative OCT examinations; C:Postoperative grayscale of perimetry; D: Postoperative corrected probabilities of perimetry. A1-D1: Stage II full-thickness MH; A2-D2: Stage III full-thickness MH; A3-D3: Stage IV full-thickness MH.
Table 1 Basic data and the clinical characteristics of the 18 patients involved in this study
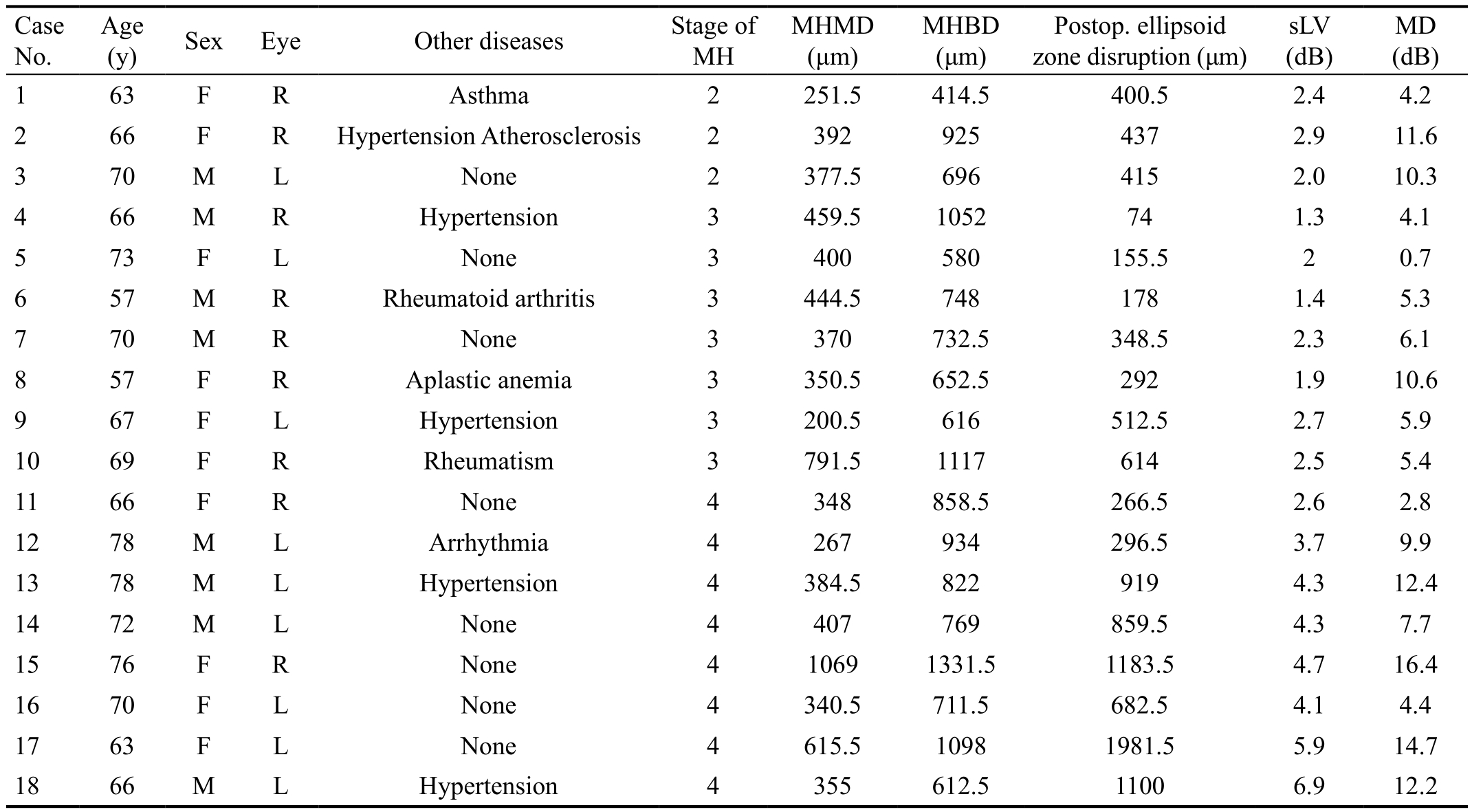
MH: Macular hole; MHMD: Macular hole minimum diameter; MHBD: Macular hole base diameter; sLV: Square root of loss variance; MD:Mean defect.
MD(dB)1 63 F R Asthma 2 251.5 414.5 400.5 2.4 4.2 2 66 F R Hypertension Atherosclerosis 2 392 925 437 2.9 11.6 3 70 M L None 2 377.5 696 415 2.0 10.3 4 66 M R Hypertension 3 459.5 1052 74 1.3 4.1 5 73 F L None 3 400 580 155.5 2 0.7 6 57 M R Rheumatoid arthritis 3 444.5 748 178 1.4 5.3 7 70 M R None 3 370 732.5 348.5 2.3 6.1 8 57 F R Aplastic anemia 3 350.5 652.5 292 1.9 10.6 9 67 F L Hypertension 3 200.5 616 512.5 2.7 5.9 10 69 F R Rheumatism 3 791.5 1117 614 2.5 5.4 11 66 F R None 4 348 858.5 266.5 2.6 2.8 12 78 M L Arrhythmia 4 267 934 296.5 3.7 9.9 13 78 M L Hypertension 4 384.5 822 919 4.3 12.4 14 72 M L None 4 407 769 859.5 4.3 7.7 15 76 F R None 4 1069 1331.5 1183.5 4.7 16.4 16 70 F L None 4 340.5 711.5 682.5 4.1 4.4 17 63 F L None 4 615.5 1098 1981.5 5.9 14.7 18 66 M L Hypertension 4 355 612.5 1100 6.9 12.2 Case No.Age(y) Sex Eye Other diseases Stage of MH MHMD(μm)MHBD(μm)Postop. ellipsoid zone disruption (μm)sLV(dB)
Association Between Central Visual Field Defect and Macular Hole Stage The Spearman coefficient for the correlation between sLV and MH stage was significant (0.705;P<0.01). There was statistically significant difference in terms of sLV among different MH stages (P<0.01). We also found significant differences in sLV between stage III and IV fullthickness MH (P<0.05). Any two residual levels of MH stage in sLV showed no statistically significant difference.Our study found no relationship between MD and MH stage(Table 2).
Table 2 Comparison of VFD parameters or postoperative ellipsoid zone disruption between each two levels of MH stage
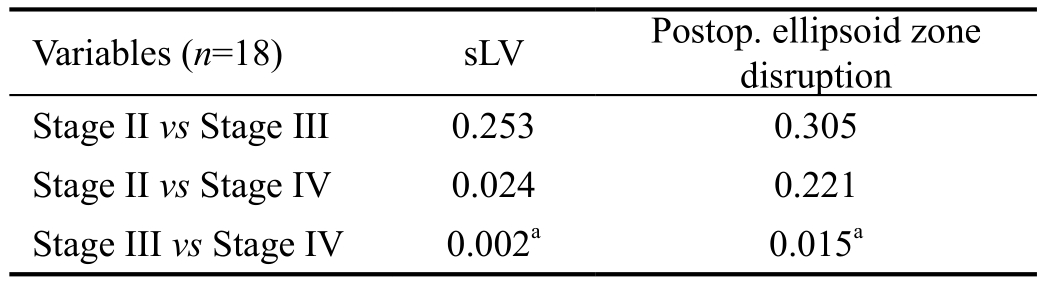
sLV: Square root of loss variance. Values in the table are Spearman coefficient; aP<0.05.
Variables (n=18) sLV Postop. ellipsoid zone disruption Stage II vs Stage III 0.253 0.305 Stage II vs Stage IV 0.024 0.221 Stage III vs Stage IV 0.002a 0.015a
Association Between Central Visual Field Defect and Macular Hole Size The Spearman coefficient for the correlation between sLV and MHMD was 0.026 (P>0.05) and was 0.243(P>0.05) for the correlation between MD and MHMD. The Spearman coefficient for the correlation between sLV and MHBD was 0.246 (P>0.05) and was 0.315 (P>0.05) for the correlation between MD and MHBD. These results showed that neither MHMD nor MHBD showed any statistically significant relationship with sLV or MD in the present study .
Association Between Central Visual Field Defect and Postoperative Ellipsoid Zone Disruption The Spearman coefficient for the correlation between sLV and postoperative ellipsoid zone disruption was 0.877 (P<0.01) and was 0.721(P<0.01) for the correlation between MD and postoperative ellipsoid zone disruption. Both sLV and MD exhibited statistically significant relationships with postoperative ellipsoid zone disruption (R2=0.726, P<0.001; R2=0.483,P<0.001, respectively; Figures 2, 3).
Association Between Postoperative Ellipsoid Zone Disruption and Macular Hole Stage We identified a significant relationship between postoperative ellipsoid zone disruption and MH stage (r=0.470, P<0.05). We also observed a statistically significant difference in postoperative ellipsoid zone disruption among different MH stages (P<0.05). After comparing postoperative ellipsoid zone disruption between any two levels of MH stage, we found that there was a statistically significant difference in postoperative ellipsoid zone disruption between stage III and stage IV full-thickness MH (P<0.05).Any two residual levels of MH stage in postoperative ellipsoid zone disruption showed no statistically significant difference(Table 2).
DISCUSSION
VFD is a common complication after MH surgery. However,with advancements in research, and the evolution of treatment strategies, the incidence of VFD has been decreasing; however,this condition still remains problems and the pathogenesis of this condition is still debated. cVFD causes an impact on the vast majority of daily life activities, so it is essential that we understand the pathogenic mechanisms involved in this condition. This retrospective study was designed to investigate the possible causes of cVFD after MH surgery.
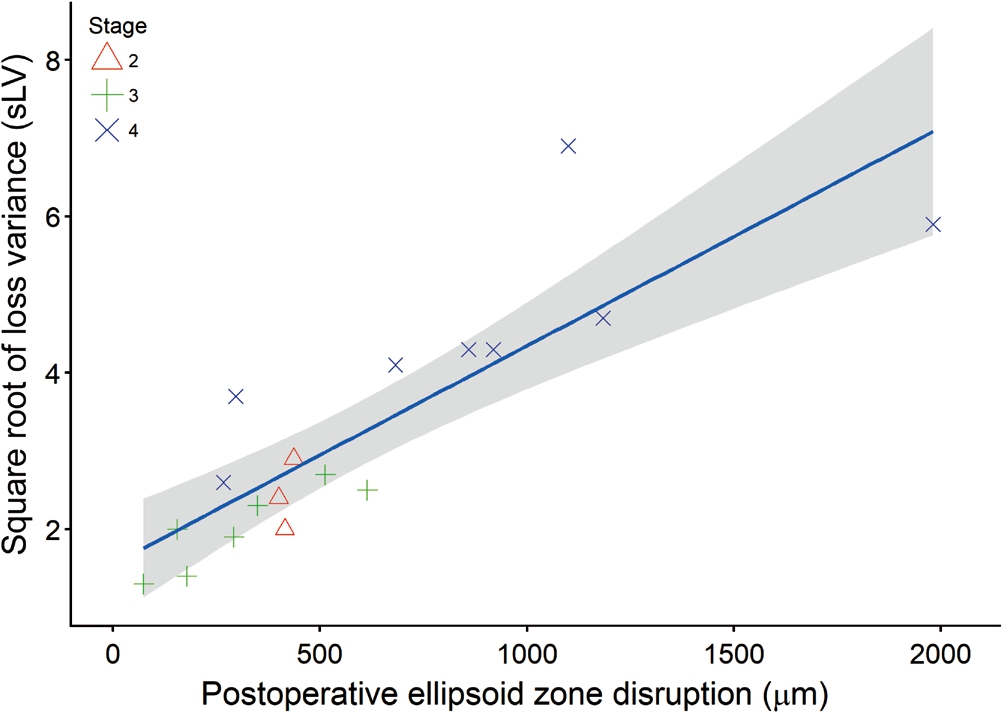
Figure 2 Relationship between sLV and postoperative ellipsoid zone disruption. y=1.555+0.003x (R2=0.726).
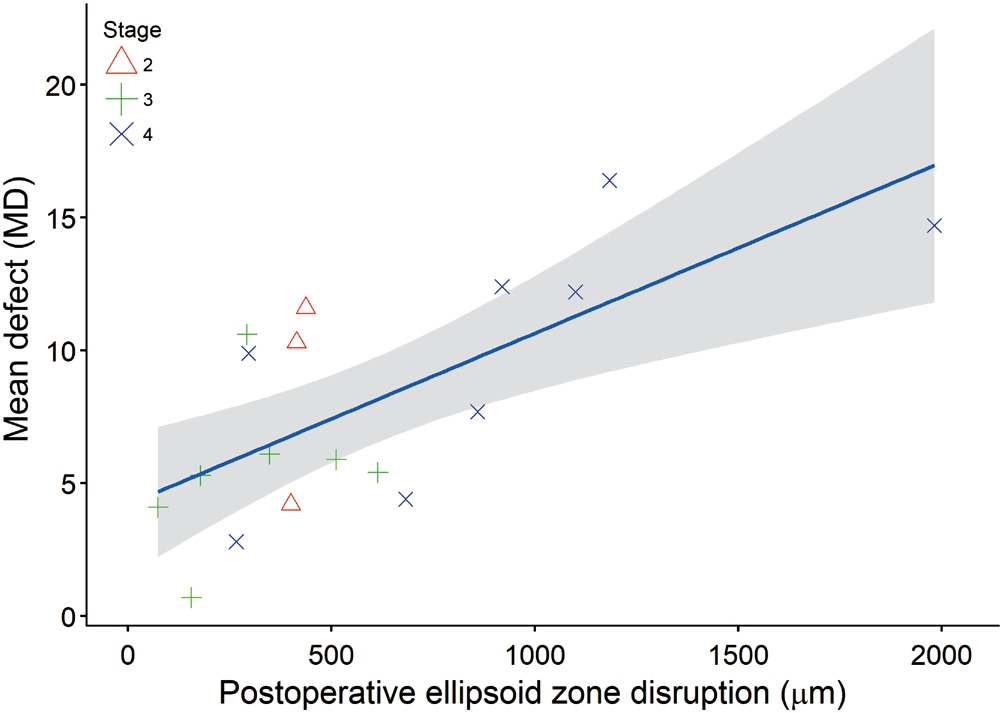
Figure 3 Relationship between MD and postoperative ellipsoid zone disruption. y=4.205+0.006x (R2=0.483).
MD and sLV were selected as qualitative parameters with which to analyze the perimetry. MD represents the arithmetic mean of the sensitivity loss and the mean measure of how depressed a patient’s VF is. MD takes all local defects into account, including even small effects. sLV represents the standard deviation of the individual defects at all visual field locations and provides a measure of variability across the entire visual field. This index is sensitive to irregularity and is an indicator of localized damage[15-16]. Gonzalez et al[17] also reported that sLV in the initial stages of glaucoma appears to be a better predictor of progression from ocular hypertension to glaucoma than MD. In the present study, we found that sLV was a better index for evaluating cVFD after MH surgery than MD.
Prior to MH surgery, MH stage could represent an index of primary damage with which to evaluate the morbidity of cVFD. In the present study, we found that sLV had a strong correlation with MH stage (P<0.01) and there were statistical differences of sLV among different MH stages (P<0.05). After comparing sLV between any two levels of MH stage, we found that sLV was significantly different between stage III and IV full-thickness MH (P<0.05). We can also conclude that cVFD after MH surgery was related to MH stage, although our small sample size limits the rigor of this conclusion. Furthermore,as MH stage increased, so did the sLV. Insufficient evidence prevented us from reaching a conclusion for MD.
MHMD and MHBD were selected to represent MH size in the present study because they could represent prognostic factors before surgery for postoperative visual outcome and the anatomical success rate of MH surgery[18]. In addition,Grigoropoulos et al[19] have previously confirmed that reorganization of the photoreceptor layer was related to MHMD and MHBD[20-21]. Although MH size is of significant importance in the recovery of MH patients, neither MHMD nor MHBD showed a relationship with sLV or MD in the present study; we believe that this due to our small sample size.
The inner and outer segments of photoreceptors are widely accepted as being an essential factor for improvement in VA[22]. Inoue et al[23] found that the postoperative ellipsoid zone junction plays a vital role in visual recovery after MH surgery.Chen et al[24] also found that patients in whom the structure of ellipsoid zone junction was in good condition tended to have a better visual prognosis. Christensen et al[25] further reported that discontinuity of the ellipsoid zone junction with a diameter over 1500 µm 3mo after surgery was associated with poorer VA than less extensive discontinuity. Based on such data, postoperative ellipsoid zone disruption was chosen to conduct correlation analysis with cVFD as the main form of postoperative evaluation in the present study. We found that sLV and MD had a strong relationship with postoperative ellipsoid zone disruption (P<0.01, P<0.01, respectively)and exhibited a statistically significant relationship with postoperative ellipsoid zone disruption (R2=0.726, P<0.01;R2=0.483, P<0.01, respectively). Thus, we can conclude that cVFD after MH surgery was related to postoperative ellipsoid zone disruption, and that patients with less postoperative ellipsoid zone disruption tended to have reduced levels of sLV or MD.
Different types of elements influence postoperative ellipsoid zone disruption. One of the major factors in this disruption is the regeneration of photoreceptors after damage. In a previous study, Horton et al[26] reported that damaged cones are capable, under some circumstances, of generating new outer segments. Moreover, Horton et al[26] reported that peripheral VFD recovered due to the regeneration of cones. Although one patient in this previous study had cVFD after 1y follow-up,it was not possible to conclude that the cones in the macular of this patient did not have sufficient ability to regenerate or restore cVFD.
The regeneration of photoreceptors depends upon an appropriate photoreceptor microenvironment. In a previous study, Fraser et al[27] reported that the microenvironment formed by the remaining retinal cells might be influential in determining the identity of regenerating photoreceptors following the death of cones. The photoreceptor microenvironment includes many types of cells and their cytokines. Developing a better microenvironment around damaged photoreceptors creates more physiological conditions. This environment could be influenced by the degree and period of damage, the size of the MH and whether there was a pseudo-operculum,preoperatively. A previous study of stage I impending MH patients found that restoration of the foveal photoreceptor layer was more likely to occur in eyes with a foveal pseudocyst and a smaller aperture size[21]. In our study, we found a significant relationship between postoperative ellipsoid zone disruption and MH stage (r=0.470, P<0.05), and that postoperative ellipsoid zone disruption among different MH stages showed statistically significance differences (P<0.05).We also found significant differences in postoperative ellipsoid zone disruption between stage III and IV full-thickness MH(P<0.05) which could confirm this hypothesis. Taking this data into consideration, we believe that MH stage could influence postoperative ellipsoid zone disruption by their effects upon the photoreceptor regeneration microenvironment,which represents a significant factor for the regeneration of photoreceptors.
In conclusion, we found that cVFD after MH surgery was related to MH stage and postoperative ellipsoid zone disruption. MH stage influenced photoreceptor regeneration by directly influence its microenviroment which further affected postoperative ellipsoid zone disruption
This study had several limitations which need to be considered.First, this was a retrospective study. Only patients with a VA>0.1 were involved. Patients with a VA<0.1 may have shown improvement of the VFD. Second, with only 18 cases, our sample size was too limited to generate firm conclusions.Third, the sample size of LMH patients with integrity and absence of the ellipsoid zone liner should be increased in future studies in order to generate a more rigorous conclusion.Further studies are now needed to investigate how cVFD recovery changes and how postoperative ellipsoid zone disruption recovers over time.
ACKNOWLEDGEMENTS
Foundations: Supported by National Natural Science Foundation of China (No.81670865; No.81500743); Natural Science Foundation of Tianjin (No.16JCQNJC13000).
Conflicts of Interest: Li JN, None; Wang JX, None; Zhu XL, None; Yan H, None.
1 Kelly NE, Wendel RT. Vitreous surgery for idiopathic macular holes.Results of a pilot study. Arch Ophthalmol 1991;109(5):654-659.
2 Oh H. Idiopathic macular hole. Dev Ophthalmol 2014;54:150-158.
3 Melberg NS, Thomas MA. Visual field loss after pars plana vitrectomy with air/fluid exchange. Am J Ophthalmol 1995;120(3):386-388.
4 Gass CA, Haritoglou C, Messmer EM, Schaumberger M, Kampik A.Peripheral visual field defects after macular hole surgery: a complication with decreasing incidence. Br J Ophthalmol 2001;85(5):549-551.
5 Garweg JG, Bergstein D, Windisch B, Koerner F, Halberstadt M.Recovery of visual field and acuity after removal of epiretinal and inner limiting membranes. Br J Ophthalmol 2008;92(2):220-224.
6 Desapriya E, Hewapathirane DS, Pike I. Central visual field loss and driving. JAMA Ophthalmol 2013;131(6):819-821.
7 Schmeiser B, Daniel M, Kogias E, Bohringer D, Egger K, Yang S, Foit NA, Schulze-Bonhage A, Steinhoff BJ, Zentner J, Lagreze WA, Gross NJ. Visual field defects following different resective procedures for mesiotemporal lobe epilepsy. Epilepsy Behav 2017;76:39-45.
8 de Moraes CG, Furlanetto RL, Ritch R, Liebmann JM. A new index to monitor central visual field progression in glaucoma. Ophthalmology 2014;121(8):1531-1538.
9 Ogawa K, Ishikawa H, Suzuki Y, Oishi M, Kamei S. Clinical study of the visual field defects caused by occipital lobe lesions. Cerebrovasc Dis 2014;37(2):102-108.
10 Abegao Pinto L, Vandewalle E, Marques-Neves C, Stalmans I. Visual field loss in optic disc drusen patients correlates with central retinal artery blood velocity patterns. Acta Ophthalmol 2014;92(4):286-291.
11 Nakazawa M, Suzuki Y, Ito T, Metoki T, Kudo T, Ohguro H. Longterm effects of nilvadipine against progression of the central visual field defect in retinitis pigmentosa: an extended study. Biomed Res Int 2013;2013:585729.
12 Yan H, Dhurjon L, Chow DR, Williams D, Chen JC. Visual field defect after pars plana vitrectomy. Ophthalmology 1998;105(9):1612-1616.
13 Lee CS, Koh HJ, Lim HT, Lee KS, Lee SC. Prognostic factors in vitrectomy for lamellar macular hole assessed by spectral-domain optical coherence tomography. Acta Ophthalmol 2012;90(8):e597-e602.
14 Gass JD. Reappraisal of biomicroscopic classification of stages of development of a macular hole. Am J Ophthalmol 1995;119(6):752-759.
15 Flammer J. The concept of visual field indices. Graefes Arch Clin Exp Ophthalmol 1986;224(5):389-392.
16 Garcia-Medina JJ, Garcia-Medina M, Zanon-Moreno V, Garcia-Maturana C, Cruz-Espinosa FJ, Pinazo-Duran MD. Comparison of global indices and test duration between two visual field analyzers:Octopus 300 and Topcon SBP-3000. Graefes Arch Clin Exp Ophthalmol 2012;250(9):1347-1351.
17 Gonzalez de la Rosa M, Gonzalez-Hernandez M, Diaz Aleman T,Sanchez Mendez M. Stabilization and comparison of TOP and Bracketing perimetric strategies using a threshold spatial filter. Graefes Arch Clin Exp Ophthalmol 2007;245(9):1303-1309.
18 Ullrich S, Haritoglou C, Gass C, Schaumberger M, Ulbig MW, Kampik A. Macular hole size as a prognostic factor in macular hole surgery. Br J Ophthalmol 2002;86(4):390-393.
19 Grigoropoulos VG, Theodossiadis GP, Theodossiadis PG. Association of the preoperative photoreceptor layer defect as assessed by optical coherence tomography with the functional outcome after macular hole closure: a long follow-up study. Ophthalmologica 2011;225(1):47-54.
20 He F, Yu WH, Dai RP, Zhang ZQ, Dong FT. Recovery of photoreceptor inner/outer segment junction in spectral domain optical coherence tomography after surgery in idiopathic macular hole. Zhonghua Yan Ke Za Zhi 2011;47(6):504-507.
21 Lee EK, Heo JW, Yu HG, Chung H. Recovery of foveal photoreceptor integrity after vitrectomy in eyes with an impending macular hole with vitreomacular traction syndrome. Retina 2016;36(8):1454-1462.
22 Morawski K, Jędrychowska-Jamborska J, Kubicka-Trzaska A,Romanowska-Dixon B. The analysis of spontaneous closure mechanisms and regeneration of retinal layers of a full-thickness macular hole:relationship with visual acuity improvement. Retina 2016;36(11):2132-2139.
23 Inoue M, Watanabe Y, Arakawa A, Sato S, Kobayashi S, Kadonosono K. Spectral-domain optical coherence tomography images of inner/outer segment junctions and macular hole surgery outcomes. Graefes Arch Clin Exp Ophthalmol 2009;247(3):325-330.
24 Chen WC, Wang Y, Li XX. Morphologic and functional evaluation before and after successful macular hole surgery using spectral-domain optical coherence tomography combined with microperimetry. Retina 2012;32(9):1733-1742.
25 Christensen UC, Kroyer K, Sander B, Larsen M, la Cour M. Prognostic significance of delayed structural recovery after macular hole surgery.Ophthalmology 2009;116(12):2430-2436.
26 Horton JC, Parker AB, Botelho JV, Duncan JL. Spontaneous regeneration of human photoreceptor outer segments. Sci Rep 2015;5:12364.
27 Fraser B, DuVal MG, Wang H, Allison WT. Regeneration of cone photoreceptors when cell ablation is primarily restricted to a particular cone subtype. PLoS One 2013;8(1):e55410.