INTRODUCTION
Retinal vein occlusion (RVO) is a common retinal vascular disorder, and its estimated 15-year cumulative incidence is 2.3% in the population, with a majority of cases being branch retinal vein occlusion (BRVO)[1-2]. BRVO mostly occurs at arteriovenous crossings where a retinal artery crosses over a retinal vein within a common adventitial sheath[3]. Systemic vascular diseases such as hypertension and arteriosclerosis, which are associated with thickening of the retinal artery, are risk factors for BRVO[3-12]. Other risk factors include diabetes mellitus, smoking, hyperlipidemia, glaucoma,and ocular inflammatory diseases[3-12].
Several investigations support the pathophysiological correlation between BRVO and glaucoma. One study showed that ocular blood flow was significantly lower in both BRVO-affected eyes and non-affected contralateral eyes, suggesting that significant vascular pathogenesis exists in patients with BRVO, like central retinal vein occlusion (CRVO) and hemi-CRVO[13]. It has been reported that the laminar and prelaminar thicknesses in BRVO-affected eyes and contralateral eyes were significantly thinner than those of normal control groups[14].Our study group also investigated changes in peripapillary choroidal thickness (PCT) in patients with unilateral BRVO[15].The mean PCT value was significantly reduced over a 12-month period in both BRVO-affected eyes and nonaffected contralateral eyes, and the reduction was significantly greater in BRVO-affected eyes[15]. Along with structural changes of the optic nerve in patients with BRVO, one study investigated glaucoma progression in patients with glaucoma who developed unilateral BRVO in the contralateral eyes[16].They showed that BRVO occurred in eyes with more advanced stages of glaucoma, and the patients who developed BRVO showed more rapid glaucoma progression in the contralateral eyes without BRVO compared with glaucoma patients who did not develop BRVO. These studies suggest that there may be a pathophysiological correlation of BRVO and glaucoma.
One study evaluated regional changes of choroidal thickness in BRVO with macular edema[17]. They showed that the mean choroidal thickness of the occlusive area was significantly thicker than that of the non-occlusive, subfoveal, and corresponding areas in the contralateral eyes and normal control eyes[17]. Because BRVO is a sectoral disease, there can also be regional differences in the mean PCTs. However, our previous study lacked sectoral analyses of PCTs in BRVO patients.
Thus, in this study, we investigated sectoral changes in mean PCT values in patients with unilateral BRVO. In addition, we investigated the possible effect of the occluded location on the changes of sectoral PCT changes.
SUBJECTS AND METHODS
Ethical Approval The Institutional Review Board of International St. Mary’s Hospital, Catholic Kwandong University College of Medicine approved the study. The study design and protocols adhered to the tenets of the Declaration of Helsinki. We obtained written informed consent from each patient at the time of fluorescein angiography (FA).
Enrollment of Study Subjects For this retrospective,interventional study, we reviewed the medical records of treatment-naïve patients who were diagnosed with acute unilateral BRVO from January 2015 to September 2016 in the Vitreoretinal Clinic at Catholic Kwandong University College of Medicine, Incheon, Republic of Korea.
Inclusion criteria for this current study were as follows: 1)treatment-naïve acute, unilateral BRVO diagnosed using FA, and 2) follow-up for at least 6mo after being diagnosed with BRVO. We excluded patients with one or more of the following: 1) long-standing BRVO for greater than 3mo;2) high intraocular pressure (≥22 mm Hg) as measured using a Goldmann contact tonometer; 3) increased cupdisc ratio (≥0.5); 4) any history of glaucoma before being diagnosed with BRVO; 5) axial length ≥26.5 mm and any signs of pathological myopia (e.g. a lacquer crack or posterior staphyloma); 6) concomitant ocular disease (e.g. central serous chorioretinopathy, diabetic retinopathy, or epiretinal membrane); or 7) treatment for macular edema combined with BRVO because intravitreal agents could affect choroidal thickness[18-20].
The primary outcome measurement was the sectoral change in mean PCT over 6mo in patients with unilateral BRVO.
Ocular Examination During the initial visit, we performed a thorough baseline examination for each patient that included a slit lamp examination, measurement of intraocular pressure using a Goldmann tonometer, and a fundus examination after dilation. We used an autorefractor to measure refractive error and converted the results to spherical equivalents [diopters(D)]. We used partial coherence interferometry (IOL Master;Carl Zeiss, Dublin, CA, USA) to measure the axial length of each eye. We used a confocal scanning laser ophthalmoscope and the Heidelberg Retina Angiograph system (HRA-2;Heidelberg Engineering, Dossenheim, Germany) to perform FA. In our clinical setting, we closely monitor patients with BRVO in the first 6mo after the diagnosis. We ask patients with newly developed BRVO to visit the ophthalmology clinic monthly during the first 6mo, and then adjusted the subsequent follow-up intervals according to each patient’s status. Thus, we could investigate the patients’ data at baseline and at 1-, 3-, and 6-month follow-up visits in this study.
Measurement of Peripapillary Choroidal Thickness We measured the PCT using spectral domain optical coherence tomography (OCT) with the enhanced depth imaging (EDI)modality (Spectralis; Heidelberg Engineering). A retinal nerve fiber layer (RNFL) circle scan centered on the optic nerve head (3.40 mm diameter) was used to measure the PCT.The scans consisted of 1024 A-scans with high definition frame enhancement software. The instrument’s light source emitted light at an 810-nm wavelength. To improve choroidal visualization, each image was created from 100 averaged B-scans in a single raster line scan. We defined the PCT as the perpendicular distance from the outer border of the hyperreflective line representing the retinal pigment epithelium to the chorioscleral interface. Two independent observers(Kang HM and Lee NE) who were blinded to the clinical data of each patient measured the PCT using digital calipers provided by the Heidelberg Spectralis OCT software, and the values were averaged. We used the mean PCT values measured by Kang HM (senior retinal specialist) if the difference between the measured values were less than 10 μm. If the difference of the measured PCT values were different more than 10 μm, the senior investigators (Koh HJ and Lee SC)made the final judgement.
We measured PCT at eight locations (i.e. superior, superonasal,nasal, inferonasal, inferior, inferotemporal, temporal, and superotemporal) and then averaged the measurements to obtain the mean PCT value (Figure 1). We also calculated the difference in PCT between baseline and 6mo (delta PCT; ΔPCT)and the ratio of the change in PCT (percent PCT; %PCT) as follows: absolute value of ΔPCT/baseline PCT×100%.
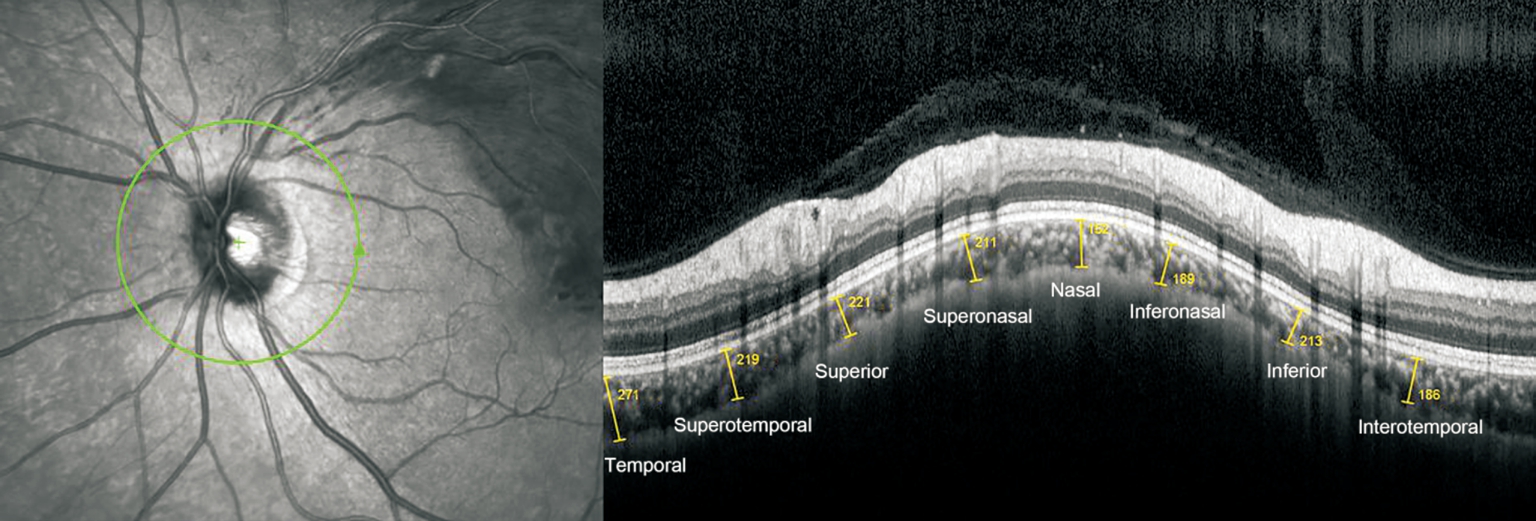
Figure 1 Representative image of PCT measurement in a 53-year-old male patient with unilateral BRVO in the left eye PCT was measured using spectral domain OCT with EDI. A circular scan centered on the optic nerve head (3.40-mm diameter, “RNFL circle scan”) in the peripapillary area. Choroidal thickness was defined as the perpendicular distance from the outer border of the hyperreflective line representing the retinal pigment epithelium to the chorioscleral interface. PCT was measured at eight locations (yellow lines from left to right: temporal,superotemporal, superior, superonasal, nasal, inferonasal, inferior, and inferotemporal), and then averaged for each eye. BRVO: Branch retinal vein occlusion; PCT: Peripapillary choroidal thickness; OCT: Optical coherence tomography; EDI: Enhanced depth imaging.
For sectoral analysis of PCT, we divided the peripapillary area into four sectors [i.e. superior (SPCT), temporal (TPCT),inferior (IPCT), and nasal (NPCT)]. We calculated the mean SPCT by averaging the PCT measurements obtained at the superonasal, superior, and superotemporal locations. We averaged the PCT measurements obtained at the inferonasal,inferior, and inferotemporal locations to calculate the mean IPCT. We also calculated the difference between baseline and 6mo (ΔSPCT, ΔTPCT, ΔIPCT, and ΔNPCT) and the ratio of the change (%SPCT, %TPCT, %IPCT, and %NPCT) for each sector. After the sectoral analysis was completed, we performed a subgroup analysis between the superior BRVO eyes (superotemporal and superonasal BRVO) and the inferior BRVO eyes (inferotemporal and inferonasal BRVO) to determine whether there were any differences in PCT changes according to the affected location.
To measure the subfoveal choroidal thickness (SFCT), at least two good-quality horizontal and vertical scans across the fovea for each eye were analyzed. Using digital calipers provided by the Heidelberg Spectralis software, the SFCT was measured at the subfovea, and was trans-sectionally imaged horizontally and vertically, and then averaged.
Statistical Analysis We summarized the data as the mean±standard deviation (SD) (range) values, unless otherwise indicated. We used the IBM SPSS Statistics 21.0 for Windows software (IBM Corporation, Somers, NY, USA) for the statistical analyses. We used repeated-measures analysis of variance to assess the significance between repeatedly measured variables. We used the Student’s t-test for continuous variables and the Chi-square test for categorical variables to compare BRVO-affected and non-affected eyes. We also performed subgroup analysis between the superior BRVO and inferior BRVO groups using the Mann-Whitney U test for continuous variables and the chi-square test for categorical variables. We used Mauchly’s test of sphericity and Kolmogorov-Smirnov analyses to confirm statistical validity. Results with P<0.05 were considered statistically significant.
Table 1 Comparison of baseline characteristics between the BRVO-affected eyes and non-affected contralateral eyes
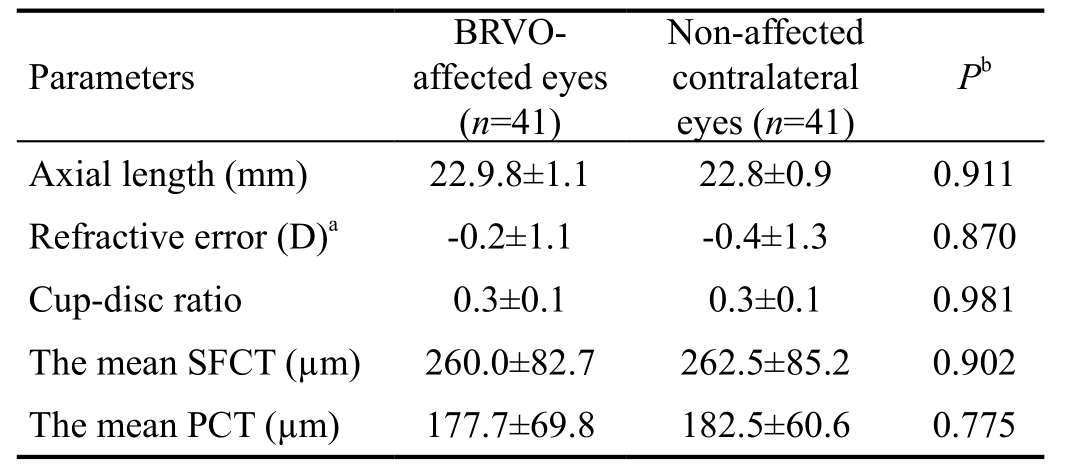
BRVO: Branch retinal vein occlusion; SFCT: Subfoveal choroidal thickness; PCT: Peripapillary choroidal thickness. aSpherical equivalent; bStudent’s t-test was used for comparison between the BRVO-affected eyes and non-affected contralateral eyes. P<0.05 was set as statistically significant.
?
RESULTS
Baseline Characteristics of the Study Population Forty-one patients met the study criteria. In total, 18 patients (43.9%) were male, and the mean age at the time of BRVO diagnosis was 61.2±11.3y (range, 40-82y). The mean duration of symptoms was 14.5±5.1d (range, 1-30d). The affected sites were: superior in 28 (68.3%) patients [26 (63.4%) at superotemporal and 2 (4.9%) at superonasal] and inferior in 13 (31.7%) patients(all inferotemporal).
We compared baseline characteristics between the BRVO-affected eyes and the non-affected contralateral eyes.There was no statistically significant difference in baseline characteristics between the BRVO-affected eyes and the nonaffected contralateral eyes (Table 1).
Changes in the Peripapillary Choroidal Thickness over 6mo In the BRVO-affected eyes, the mean PCT was 177.7±69.8 μm(range, 70.1-396.0 μm) at baseline and 127.8±54.8 μm (range,56.4-312.1 μm) at 6mo. In the non-affected contralateral eyes,the mean PCT was 192.5±60.6 μm (range, 61.4-365.0 μm) at baseline and 165.9±61.1 μm (range, 56.8-326.8 μm) at 6mo.The mean PCT decreased significantly over 6mo in both BRVO-affected and non-affected eyes (both P<0.001; Figure 2).Comparison of the mean PCT values revealed that there were no statistically significant differences between BRVO-affected eyes and non-affected contralateral eyes at baseline, 1, and 3mo (P=0.775, P=0.127, and P=0.076, respectively). However,the mean PCT was significantly lower in the BRVO-affected eyes than in the non-affected eyes at 6mo (P=0.010).
In the BRVO-affected eyes, the mean ΔPCT was -46.9±32.9 μm(range, -112.7 to -9.8 μm); the mean %PCT was 32.2%±14.4%(range, 0.5%-65.1%). In the non-affected contralateral eyes,the mean ΔPCT was -19.7±21.0 μm (range, -53.9-10.1 μm),and the mean %PCT was 16.2%±11.5% (range, 2.4%-39.8%).The mean ΔPCT and %PCT were significantly greater in the BRVO-affected eyes compared with the non-affected eyes(P<0.001 for both).
Changes in Subfoveal Choroidal Thickness over 6mo in Unilateral Branch Retinal Vein Occlusion At baseline, the mean SFCT was 260.0±82.7 µm (range, 145.5-364.5 µm) in the BRVO-affected eyes, and 262.5±85.2 µm (range, 157.5-372.5 µm) in the non-affected contralateral eyes (P=0.816).At 6mo, the mean SFCT was 246.0±92.7 µm (range, 137.5-335.5 µm) in the BRVO-affected eyes, and 257.1±80.8 µm(range, 154.5-357.5 µm) in the non-affected contralateral eyes (P=0.436). During the 6-month follow-up period, the mean SFCT was not significantly changed in both the BRVO-affected eyes (P=0.450) and the non-affected contralateral eyes(P=0.910).
Changes in Peripapillary Choroidal Thickness of Four Sectors over 6mo in the Branch Retinal Vein Occlusion Affected Eyes and Non-affected Contralateral Eyes After we assessed mean the PCT, we performed additional sectoral analyses of the BRVO-affected eyes and the non-affected contralateral eyes. In the BRVO-affected eyes, the mean PCT was significantly reduced in all sectors over 6mo (P<0.001 for all sectors). In the non-affected contralateral eyes, the mean PCT did not significantly change for any sector over the 6-month follow-up (P=0.143, P=0.825, P=0.192, and P=0.599 for the superior, temporal, inferior, and nasal sectors,respectively).
We then compared the mean PCT at each sector between the BRVO-affected eyes and non-affected contralateral eyes.There were no significant differences at baseline in any sectors(P=0.390 for SPCT, P=0.532 for TPCT, P=0.420 for IPCT,and P=0.374 for NPCT). However, the mean sectoral PCT values were significantly lower in the BRVO-affected eyes than in the non-affected contralateral eyes in all sectors at 6mo(P=0.030 for SPCT, P=0.016 for TPCT, P=0.003 for IPCT, and P=0.026 for NPCT). We also compared ΔPCT and %PCT for each sector between the BRVO-affected eyes and non-affected contralateral eyes. The mean ΔPCT and %PCT for each sector was significantly larger in the BRVO-affected eyes than the non-affected contralateral eyes as shown in Table 2.
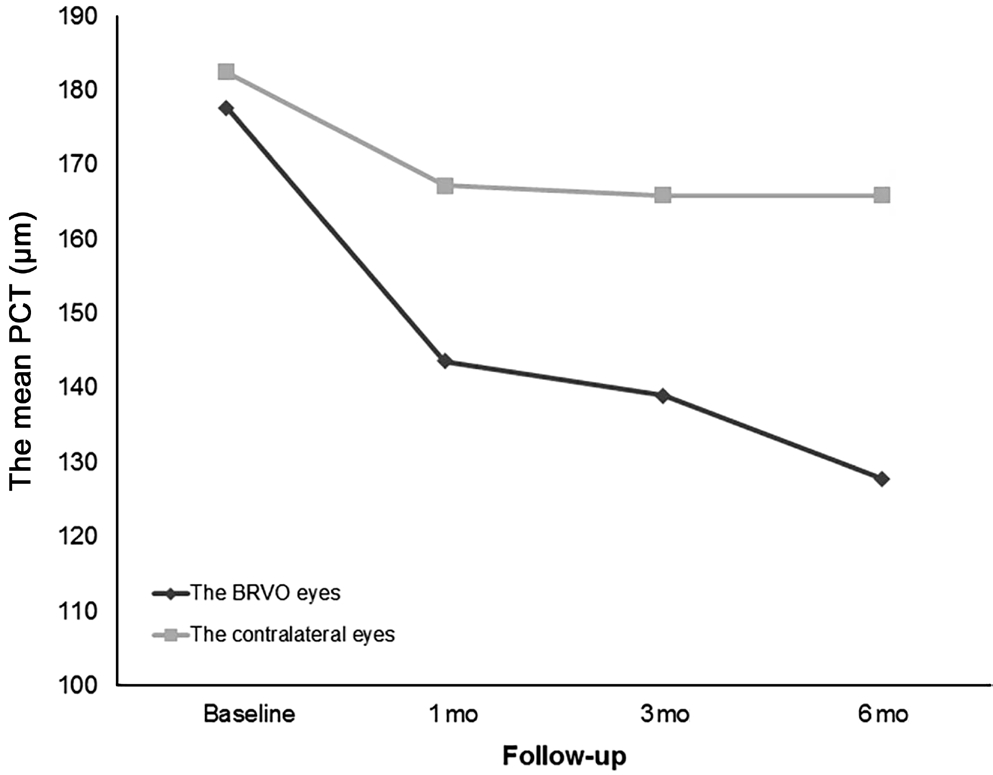
Figure 2 Changes in mean PCT over 6mo in BRVO-affected eyes and non-affected contralateral eyes in patients with unilateral BRVO The mean PCT decreased significantly over 6mo in BRVO-affected and non-affected eyes (both P<0.001). ΔSPCT and %SPCT were significantly greater in the BRVO-affected eyes compared with the non-affected contralateral eyes (P=0.009 for both). BRVO: Branch retinal vein occlusion; SFCT: Subfoveal choroidal thickness; PCT:Peripapillary choroidal thickness.
Comparisons of Peripapillary Choroidal Thickness Between Eyes with Superior Branch Retinal Vein Occlusion and Those with Inferior Branch Retinal Vein Occlusion Twenty-eight patients in the study population had superior BRVO (the superior group). Twenty-six of these patients had superotemporal BRVO and two patients had superonasal BRVO. Thirteen patients had inferior BRVO (the inferior group, all interotemporal BRVO).
In the superior group, the mean values for PCT, SPCT,TPCT, IPCT, and NPCT were significantly reduced over 6mo (P=0.001, P=0.002, P<0.001, P<0.001, and P=0.005,respectively). There was a similar trend for the inferior group(P<0.004 for the mean PCT, P<0.001 for the mean SPCT and the mean IPCT, P=0.049 for the TPCT, and P=0.002 for the NPCT). The mean ΔPCT value was -49.6±34.6 μm in the superior group and -39.5±28.4 μm in the inferior group(P=0.218). The mean %PCT was 32.4%±12.1% in the superior group and 31.9%±20.0% in the inferior group (P=0.929). The mean ΔPCT and %PCT for each sector were not significantly different between the superior group and the inferior group.The results are shown in Table 3.
DISCUSSION
This was the first attempt to investigate sectoral changes of mean PCT in patients with unilateral BRVO. The mean PCTwas significantly reduced in both BRVO-affected eyes and non-affected contralateral eyes, which was consistent with a previous investigation[17]. We also divided the peripapillary area into four sectors: superior, temporal, inferior, and nasal.Further sectoral analyses showed significant thinning of each sector in the BRVO-affected eyes, but not in the non-affected contralateral eyes. After sectoral analyses, we compared the mean PCT of each sector between the patients with superiorBRVO and inferior BRVO. The mean PCT of each sector was significantly reduced regardless of the occlusion site in the
patients with BRVO. The amount and ratio of PCT change were not significantly different between the patients with superior BRVO and those with inferior BRVO. The reduction of the mean SPCT was not significantly greater in the patients with superior BRVO than those with inferior BRVO, and similar results were observed in the mean IPCT. Regardless of the occlusion site, the mean PCT in each sector also retained the thickness pattern of the normal population[21-22]; that is,thickest in the superior and thinnest in the inferior, regardless of the occlusion site.
Table 2 Sectoral comparison of the mean PCT over 6mo between eyes with BRVO and non-affected contralateral eyes mean±SD, µm

BRVO: Branch retinal vein occlusion; PCT: Peripapillary choroidal thickness. aStudent’s t-test was used for comparison between the BRVO-affected eyes and non-affected contralateral eyes. P<0.05 was set as statistically significant. Sectoral analyses [(superior(SPCT), temporal (TPCT), inferior (IPCT), and nasal (NPCT)] were performed. The difference in PCT between baseline and 6mo (ΔPCT)was obtained. In addition, the ratio of the change in PCT (%PCT) was calculated using the following equation: (absolute value of ΔPCT/baseline PCT)×100%.
Parameters BRVO-affected eyes (n=41)Pa Non-affected contralateral eyes(n=41)Mean SPCT Baseline 178.6±74.4 194.1±68.2 0.390 1mo 161.8±69.4 192.0±73.5 0.100 3mo 155.0±71.4 188.7±71.1 0.067 6mo 148.5±65.7 187.4±75.2 0.030 ΔSPCT -31.1±34.5 -10.2±23.7 0.009%SPCT 19.0±12.2 11.5±9.3 0.009 Mean TPCT Baseline 148.7±66.2 158.8±62.6 0.532 1mo 137.8±68.3 160.7±73.5 0.205 3mo 129.1±57.8 161.0±66.1 0.045 6mo 120.8±61.5 148.5±59.4 0.016 ΔTPCT -27.0±28.1 -10.5±14.3 0.001%TPCT 23.8±24.8 13.3±13.5 0.023 Mean IPCT Baseline 136.9±58.1 147.9±48.1 0.420 1mo 124.6±52.1 142.0±51.7 0.193 3mo 117.6±51.8 141.0±50.0 0.065 6mo 105.9±44.5 132.4±50.1 0.003 ΔIPCT -30.8±24.9 -11.1±24.5 <0.001%IPCT 23.8±24.9 13.1±10.8 0.005 Mean NPCT Baseline 163.4±64.0 179.1±78.8 0.374 1mo 152.1±65.7 174.8±91.9 0.249 3mo 141.7±63.8 177.1±81.9 0.057 6mo 137.9±65.3 169.2±81.3 0.026 ΔNPCT -24.3±39.5 -10.2±26.2 0.018%NPCT 21.4±15.5 12.3±12.9 0.015
Table 3 In eyes with BRVO, the mean PCT over 6mo was compared between those with superior BRVO and inferior BRVO mean±SD, µm
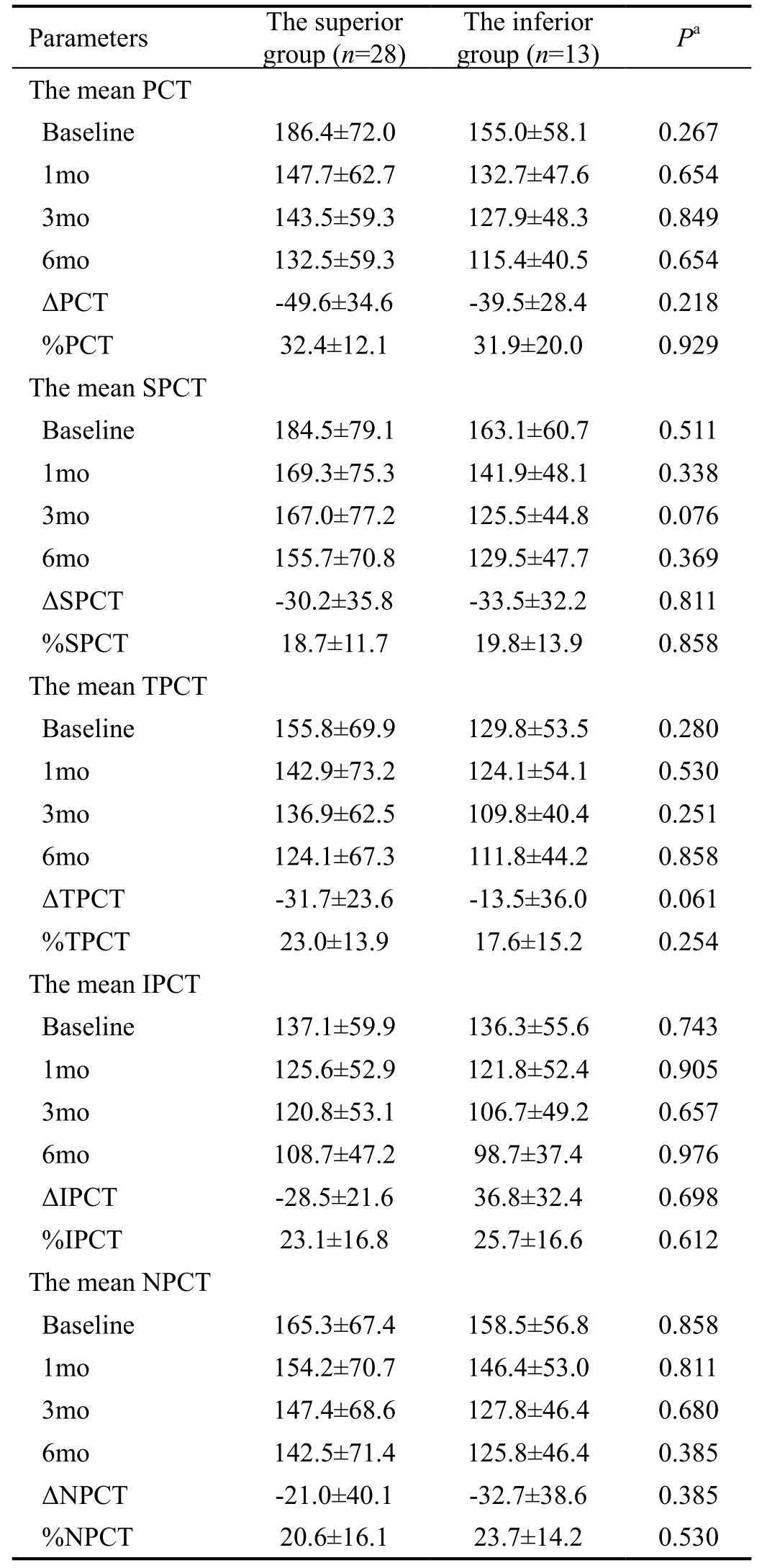
BRVO: Branch retinal vein occlusion; PCT: Peripapillary choroidal thickness. aMann-Whitney U test was used for comparison between the eyes with superior BRVO and those with inferior BRVO. P<0.05 was set statistically significant. Sectoral analyses [(superior (SPCT),temporal (TPCT), inferior (IPCT), and nasal (NPCT)] were also performed. The difference in PCT between baseline and 6mo (ΔPCT)was obtained. In addition, the ratio of the change in PCT (%PCT) was calculated using the following equation: (absolute value of ΔPCT/baseline PCT)×100%.
?
The results of the current study suggested that the choroidal blood flow in the peripapillary area may be impaired when BRVO occurs. We speculate that systemic factors predisposing patients to BRVO may also affect the peripapillary choroid.As previously mentioned, systemic vascular diseases such as hypertension and arteriosclerosis, which are associated with thickening of the retinal artery, are risk factors for BRVO[3-12] as well as for glaucoma[23-27]. These systemic conditions can also lead to increased resistance to flow, reduced perfusion pressure,or increased blood viscosity, leading to vascular insufficiency of the optic disc and predisposing to glaucoma. Several studies also support the vascular theory for both glaucoma and RVO,showing associations between disc hemorrhage, glaucoma,and RVO[28-30]. We speculate that when BRVO occurs, vascular insufficiency also affects the peripapillary choroidal blood flow, leading to generalized reduction of the mean PCT in both BRVO-affected eyes and non-affected contralateral eyes during follow-up periods. In BRVO-affected eyes, more ischemic injury associated with BRVO itself may lead to a significantly larger reduction of the mean PCT than that of non-affected contralateral eyes. In addition, vascular insufficiency of the peripapillary choroid may lead to generalized reduction of the mean PCT in each sector regardless of the location of occlusion site in our study. Further prospective studies,including investigation of peripapillary choroidal blood flow is warranted to clarify the pathophysiological correlation of the mean PCT and BRVO.
In our study, the mean SFCT and the mean PCT showed different tendencies in BRVO patients. In patients with diabetic retinopathy, another common retinal vascular disorder, it seems that macular choroidal thickness and mean PCT show similar tendencies[31-32]. Both peripapillary and macular choroidal thickness are significantly correlated with the severity of diabetic retinopathy[31-32], and are significantly reduced after panretinal photocoagulation[32]. In our study, the mean SFCT was not significantly different over 6mo, whereas the mean PCT in each sector was significantly reduced in the patients with BRVO. This discrepancy between the SFCT and PCT may be due to different mechanisms in the patients with BRVO;macular choroidal thickness changes may be the secondary effect due to BRVO, and the PCT changes are associated with the underlying vascular insufficiency in conjunction with BRVO. In the macular area, damaged vascular endothelial cells and hypoxic damage around the obstructed retinal vessels may lead to increased vascular endothelial growth factor (VEGF)release[33-37]. Increased VEGF secretion in the occluded area can lead to vascular hyperpermeability and subsequent macular choroidal thickening in the patients with BRVO[33-36]. Breakdown of the outer blood-retinal barrier can be another conduit of extravasated fluid to the choroidal space. Thus, different mechanisms could contribute to the discrepancy between the macular choroidal thickness and PCT in the patients with BRVO.
Significant reduction of the mean PCT in both BRVO-affected eyes and non-affected contralateral eyes may predispose these patients to glaucomatous optic neuropathy. The vascular theory for glaucomatous optic neuropathy states that insufficient blood supply associated with various conditions such as elevated intraocular pressure or systemic diseases affecting ocular blood flow may lead to the development of glaucoma[38-41]. Reduction of ocular blood flow was found in all ocular tissues, especially in the choroid, optic nerve head, and peripapillary area[42-43].Several studies showed associations between glaucomatous optic neuropathy, impaired choroidal circulation, and decreased blood flow to the optic nerve head[44-46]. Recent studies using EDI OCT showed that the mean PCT was significantly reduced in the patients with normotensive glaucoma, further providing evidence for the vascular theory[47-49]. Based on our results, the peripapillary choroidal circulation seems to be significantly impaired in the patients with BRVO during the followup period, especially in the BRVO-affected eyes. Impaired peripapillary choroidal blood flow and resultant peripapillary choroidal thinning may increase the risk for glaucomatous optic neuropathy in patients with BRVO, leading to further visual deterioration. Thus, close monitoring for glaucomatous optic neuropathy as well as retinal complications of BRVO may be needed to prevent further visual loss in these patients.This study had several limitations. It was a retrospective study with a relatively small study population. Due to the small study population, the occlusion areas were only classified into two groups: superior and inferior. Because of the retrospective design of the study, we lacked the visual field test results. The clinical impact of the mean PCT change on the visual field change could be more helpful in real practice.Further prospective studies with longer follow-up periods,which would include a control group and visual field tests is warranted to support the clinical impact of our findings.
In conclusion, the mean PCT was significantly reduced in both BRVO-affected eyes and non-affected contralateral eyes over 6mo in patients with unilateral BRVO. The mean PCT in each area was reduced significantly over 6mo in the BRVO-affected eyes, but not in the non-affected contralateral eyes. Sectoral changes in mean PCT values were not affected by BRVO location.
ACKNOWLEDGEMENTS
Authors’ contributions: Designed and performed the study:Lee NE, Kang HM and Choi JH; collected the data: Kang HM; managed, analyzed, and interpreted data: Lee NE, Kang HM, Choi JH, Koh HJ, and Lee SC; prepared, reviewed, and approved the manuscript: Lee NE, Kang HM, Choi JH, Koh HJ, and Lee SC.
Foundation: Supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government(MSIT) (NRF-2018R1C1B5085620).
Conflicts of Interest: Lee NE, None; Kang HM, None; Choi JH, None; Koh HJ, None; Lee SC, None.
1 Argon laser scatter photocoagulation for prevention of neovascularization and vitreous hemorrhage in branch vein occlusion. A randomized clinical trial. Branch Vein Occlusion Study Group. Arch Ophthalmol 1986;104(1):34-41.
2 Klein R, Moss SE, Meuer SM, Klein BE. The 15-year cumulative incidence of retinal vein occlusion: the Beaver Dam Eye Study. Arch Ophthalmol 2008;126(4):513-518.
3 Bowers DK, Finkelstein D, Wolff SM, Green WR. Branch retinal vein occlusion. A clinicopathologic case report. Retina 1987;7(4):252-259.
4 Frangieh GT, Green WR, Barraquer-Somers E, Finkelstein D.Histopathologic study of nine branch retinal vein occlusions. Arch Ophthalmol 1982;100(7):1132-1140.
5 Sperduto RD, Hiller R, Chew E, Seigel D, Blair N, Burton TC, Farber MD, Gragoudas ES, Haller J, Seddon JM, Yannuzzi LA. Risk factors for hemiretinal vein occlusion: comparison with risk factors for central and branch retinal vein occlusion: the eye disease case-control study.Ophthalmology 1998;105(5):765-771.
6 Rath EZ, Frank RN, Shin DH, Kim C. Risk factors for retinal vein occlusions. A case-control study. Ophthalmology 1992;99(4):509-514.
7 Jaulim A, Ahmed B, Khanam T, Chatziralli IP. Branch retinal vein occlusion: epidemiology, pathogenesis, risk factors, clinical features,diagnosis, and complications. An update of the literature. Retina 2013;33(5):901-910.
8 The Eye Disease Case-control Study Group. Risk factors for branch retinal vein occlusion. Am J Ophthalmol1993;116(3):286-296.
9 Vannas S, Tarkkanen A. Retinal vein occlusion and glaucoma.Tonographic study of the incidence of glaucoma and of its prognostic significance. Br J Ophthalmol 1960;44:583-589.
10 Beaumont PE, Kang HK. Cup-to-disc ratio, intraocular pressure, and primary open-angle glaucoma in retinal venous occlusion. Ophthalmology 2002;109(2):282-286.
11 Bucciarelli P, Passamonti SM, Gianniello F, Artoni A, Martinelli I.Thrombophilic and cardiovascular risk factors for retinal vein occlusion.Eur J Intern Med 2017;44:44-48.
12 Frucht J, Shapiro A, Merin S. Intraocular pressure in retinal vein occlusion. Br J Ophthalmol 1984;68(1):26-28.
13 Wang Y, Fawzi AA, Varma R, Sadun AA, Zhang X, Tan O, Izatt JA,Huang D. Pilot study of optical coherence tomography measurement of retinal blood flow in retinal and optic nerve diseases. Invest Ophthalmol Vis Sci 2011;52(2):840-845.
14 Son Y, Lee S, Park J. Measurement of lamina and prelaminar thicknesses of both eyes in patients with unilateral branch retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol 2017;255(3):503-508.
15 Kang HM, Choi JH, Koh HJ, Lee CS, Lee SC. Significant reduction of peripapillary choroidal thickness in patients with unilateral branch retinal vein occlusion. Retina 2018;38(1):72-78.
16 Lopilly Park HY, Jeon S, Lee MY, Park CK. Glaucoma progression in the unaffected fellow eye of glaucoma patients who developed unilateral branch retinal vein occlusion. Am J Ophthalmol 2017;175:194-200.
17 Kim KH, Lee DH, Lee JJ, Park SW, Byon IS, Lee JE. Regional choroidal thickness changes in branch retinal vein occlusion with macular edema. Ophthalmologica 2015;234(2):109-118.
18 Forte R, Cennamo G, Breve MA, Vecchio EC, de Crecchio G. Functional and anatomic response of the retina and the choroid to intravitreal bevacizumab for macular edema. J Ocul Pharmacol Ther 2012;28(1):69-75.
19 Lee EK, Han JM, Hyon JY, Yu HG. Changes in choroidal thickness after intravitreal dexamethasone implant injection in retinal vein occlusion. Br J Ophthalmol 2015;99(11):1543-1549.
20 Yumusak E, Ornek K, Dikel NH. Comparison of choroidal thickness changes following intravitreal dexamethasone, ranibizumab, and triamcinolone in eyes with retinal vein occlusion. Eur J Ophthalmol 2016;26(6):627-632.
21 Jiang R, Wang YX, Wei WB, Xu L, Jonas JB. Peripapillary choroidal thickness in adult Chinese: the Beijing Eye Study. Invest Ophthalmol Vis Sci 2015;56(6):4045-4052.
22 Gupta P, Cheung CY, Baskaran M, Tian J, Marziliano P, Lamoureux EL, Cheung CM, Aung T, Wong TY, Cheng CY. Relationship between peripapillary choroid and retinal nerve fiber layer thickness in a population-based sample of nonglaucomatous eyes. Am J Ophthalmol 2016;161:4-11.e1-2.
23 Zhao D, Cho J, Kim MH, Friedman DS, Guallar E. Diabetes, fasting glucose, and the risk of glaucoma: a meta-analysis. Ophthalmology 2015;122(1):72-78.
24 Zhou M, Wang W, Huang W, Zhang X. Diabetes mellitus as a risk factor for open-angle glaucoma: a systematic review and meta-analysis.PLoS One 2014;9(8):e102972.
25 Lockwood A, Clearkin LG. Insulin resistance in retinal vein occlusion and glaucoma. Lancet 1992;340(8827):1100-1101.
26 Bae HW, Lee N, Lee HS, Hong S, Seong GJ, Kim CY. Systemic hypertension as a risk factor for open-angle glaucoma: a meta-analysis of population-based studies. PLoS One 2014;9(9):e108226.
27 Bonomi L, Marchini G, Marraffa M, Bernardi P, Morbio R, Varotto A. Vascular risk factors for primary open angle glaucoma: the Egna-Neumarkt Study. Ophthalmology 2000;107(7):1287-1293.
28 Krakau CE. Disk hemorrhages and retinal vein occlusions in glaucoma.Surv Ophthalmol 1994;38(Suppl):S18-S21; discussion S22.
29 Sonnsjö B. Similarities between disc haemorrhages and thromboses of the retinal veins. Int Ophthalmol 1992;16(4-5):235-238.
30 Sonnsjö B, Dokmo Y, Krakau T. Disc haemorrhages, precursors of open angle glaucoma. Prog Retin Eye Res 2002;21(1):35-56.
31 Vujosevic S, Martini F, Cavarzeran F, Pilotto E, Midena E. Macular and peripapillary choroidal thickness in diabetic patients. Retina 2012;32(9):1781-1790.
32 Kang HM, Lee NE, Choi JH, Koh HJ, Lee SC. Significant reduction of both peripapillary and subfoveal choroidal thickness after panretinal photocoagulation in patients with type 2 diabetes. Retina 2018;38(10):1905-1912.
33 Tilton RG, Chang KC, LeJeune WS, Stephan CC, Brock TA,Williamson JR. Role for nitric oxide in the hyperpermeability and hemodynamic changes induced by intravenous VEGF. Invest Ophthalmol Vis Sci 1999;40(3):689-696.
34 Ferrara N. Vascular endothelial growth factor: molecular and biological aspects. Curr Top Microbiol Immunol 1999;237:1-30.
35 Noma H, Minamoto A, Funatsu H, Tsukamoto H, Nakano K,Yamashita H, Mishima HK. Intravitreal levels of vascular endothelial growth factor and interleukin-6 are correlated with macular edema in branch retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol 2006;244(3):309-315.
36 Aiello LP, Northrup JM, Keyt BA, Takagi H, Iwamoto MA. Hypoxic regulation of vascular endothelial growth factor in retinal cells. Arch Ophthalmol 1995;113(12):1538-1544.
37 Ebneter A, Kokona D, Schneider N, Zinkernagel MS. Microglia activation and recruitment of circulating macrophages during ischemic experimental branch retinal vein occlusion. Invest Ophthalmol Vis Sci 2017;58(2):944-953.
38 Flammer J, Orgül S, Costa VP, Orzalesi N, Krieglstein GK, Serra LM,Renard JP, Stefánsson E. The impact of ocular blood flow in glaucoma.Prog Retin Eye Res 2002;21(4):359-393.
39 Blumenthal M, Best M, Galin MA, Toyofuku H. Peripapillary choroidal circulation in glaucoma. Arch Ophthalmol 1971;86(1):31-38.
40 Banitt M. The choroid in glaucoma. Curr Opin Ophthalmol 2013;24(2):125-129.
41 Geijssen HC, Greve EL. Vascular concepts in glaucoma. Curr Opin Ophthalmol 1995;6(2):71-77.
42 Duijm HF, van den Berg TJ, Greve EL. Choroidal haemodynamics in glaucoma. Br J Ophthalmol 1997;81(9):735-742.
43 Wolf S, Arend O, Sponsel WE, Schulte K, Cantor LB, Reim M. Retinal hemodynamics using scanning laser ophthalmoscopy and hemorheology in chronic open-angle glaucoma. Ophthalmology 1993;100(10):1561-1566.
44 Grunwald JE, Piltz J, Hariprasad SM, DuPont J. Optic nerve and choroidal circulation in glaucoma. Invest Ophthalmol Vis Sci 1998;39(12):2329-2336.
45 Galassi F, Sodi A, Ucci F, Renieri G, Pieri B, Baccini M. Ocular hemodynamics and glaucoma prognosis: a color Doppler imaging study.Arch Ophthalmol 2003;121(12):1711-1715.
46 Nicolela MT, Hnik P, Drance SM. Scanning laser Doppler flowmeter study of retinal and optic disk blood flow in glaucomatous patients. Am J Ophthalmol 1996;122(6):775-783.
47 Park HY, Lee NY, Shin HY, Park CK. Analysis of macular and peripapillary choroidal thickness in glaucoma patients by enhanced depth imaging optical coherence tomography. J Glaucoma 2014;23(4):225-231.
48 Hirooka K, Tenkumo K, Fujiwara A, Baba T, Sato S, Shiraga F.Evaluation of peripapillary choroidal thickness in patients with normaltension glaucoma. BMC Ophthalmol 2012;12:29.
49 Usui S, Ikuno Y, Miki A, Matsushita K, Yasuno Y, Nishida K.Evaluation of the choroidal thickness using high-penetration optical coherence tomography with long wavelength in highly myopic normaltension glaucoma. Am J Ophthalmol 2012;153(1):10-16.e1.