INTRODUCTION
Laser in situ keratomileusis (LASIK) obtained with a mechanical microkeratome (MM) is an effective,safe, and predictable procedure to correct different amounts of myopia[1]. The femtosecond (FS) laser and the MM both provide fast visual rehabilitation, an almost painless postoperative period, and a low risk of development of haze. Nevertheless, the FS laser creates a more predictable thin and planar corneal flap[2-3] that is thought to have lower biomechanical impact on the cornea than the thicker, meniscusshaped flap usually obtained with an MM[3]. Nevertheless,the use of a FS laser to create a flap induces greater stromal inflammation compared to the MM flap[4-5].
Patient age is an important variable that affects the visual results of corneal refractive surgical procedures[6-7]. Some studies have shown suboptimal results with mechanical LASIK associated with increasing age[7-13], perhaps as a result of a decreased wound-healing response[7]. However, it is unknown whether the differences between the characteristics of the flaps created using an MM or an FS laser might affect the visual outcomes in different patient age groups.For this reason, we decided to evaluate the visual and refractive outcomes after LASIK performed with an MM or an FS laser to correct myopia in young and older patients.
SUBJECTS AND METHODS
Ethical Approval All patients provided informed consent,and the Institutional Review Board approval was obtained.The study was performed in accordance with the tenets of the Declaration of Helsinki.
Methods We retrospectively studied consecutive patients who underwent LASIK performed with an MM or an FS laser to correct myopia with or without astigmatism. In presbyopic patients, when conventional monovision was planned, only the dominant eye (targeted for emmetropia) was included in the study. All the surgeries were performed at the same clinic and by two experienced surgeons during the period from January 2014 to January 2017.
A masked observer performed the same complete preoperative examination that included measurement of the uncorrected distance visual acuity (UDVA), corrected distance visual acuity(CDVA) including the manifest and cycloplegic refractions,corneal keratometry and topography (CSO, Compagnia Instrumenti Oftalmici, Florence, Italy), ultrasound corneal pachymetry (DHG 5100 contact pachymeter; DHG Technology Inc., Exton, PA, USA), mesopic infrared pupillometry (Colvard Pupillometer, Oasis Medical Inc., Glendora, CA, USA), slitlamp biomicroscopy, Goldmann tonometry (CT-80, Topcon,Tokyo, Japan), and fundus examination.
When evaluated for refractive surgery, we excluded patients with unstable refractions; patients who had underwent a previous ocular surgery (refractive or other surgical procedure);keratoconus suspects (defined as any even mild localized steepening seen with Placido corneal topography or slight bowing of the posterior corneal surface detected by corneal tomography); and patients with ocular or systemic diseases,such as diabetes mellitus or connective tissue disorders, that could interfere with the wound-healing process. The decision to use an FS laser instead of an MM to create the flap was based on the preoperative keratometry (when the keratometric values were lower than 41 D or higher than 46 D, the flap was created with the FS laser) and the mesopic pupillary size (i.e. when the pupil diameter was ≥7 mm, the flap was obtained with FS laser in order to obtain a greater and more predictable flap diameter,irrespective of the preoperative corneal curvature).
In addition, when the patient was a good candidate for both procedures, the decision to perform MM or FS laser was based on patient preference after the advantages and disadvantages of both techniques were fully disclosed.
Surgical Technique Two experienced surgeons (Garcia-Gonzalez M and Teus MA) performed all the surgeries. A povidone-iodine solution was applied to the skin and the conjunctiva, and a sterile surgical drape and a rigid eyelid speculum were placed. All the procedures were performed using topical anesthesia with lidocaine 2%.
In the mechanical LASIK group, the Moria M2 MM (Moria SA, Antony, France) was used to obtain the flap. The suction rings (+2, +1, 0, or -1) and the cutting heads (90, 110, or 130 µm) were selected based on the preoperative corneal keratometry and the manufacturer’s nomogram.
In the FS LASIK group, the 60-kHz IntraLase FS laser(IntraLase Corp., Irvine, CA, USA) was used to obtain the flap,using the following parameters: a raster pattern; bed energy level, 0.9 µJ; side-cut energy, 0.90 µJ; spot separation, 7 µm;side cut angle, 70 degrees; hinge angle, 50 degrees; attempted flap depth, 100 µm; and flap diameter, 9 mm.
In both groups, once the flap was obtained, it was raised with a spatula, the stromal bed was dried with a sponge, and the ablation was applied using the Esiris Schwind Excimer Laser(Schwind Eye Tech Solutions, Kleinostheim, Germany), with an optical zone larger than or equal to the mesopic pupil size.The same age-based nomogram (provided by the manufacturer)was applied for both groups, and all treatments were conducted using conventional (non-wavefront) technology.
Once the excimer laser ablation was performed, the stromal bed was rinsed with balanced salt solution (Alcon Laboratories Inc., Ft. Worth, TX, USA) and the flap was gently put back in place with a cannula. Finally, antibiotic drops (ciprofloxacin 3 mg/mL, Oftacilox®, Alcon Cusí, Barcelona, Spain) and nonsteroidal anti-inflammatory drops (ketorolac trometamol 5 mg/mL, Acular®, Allergan, Madrid, Spain) were instilled.
Postoperative Follow-up All patients used postoperatively preservative-free artificial tears as needed and were instructed to apply topical antibiotic drops (ciprofloxacin 3 mg/mL) four times daily after both procedures during the first postoperative week. Steroid drops (dexamethasone alcohol 1 mg/mL,Maxidex®, Alcon Cusí, Spain) were instilled four times daily in the MM group and six times daily in the FS group during the first postoperative week because of the reported expected higher risk of diffuse lamellar keratitis after femto-LASIK[5].
Examinations were scheduled at 1d, 1wk, and 3mo postoperatively.At each postoperative visit two experienced optometrists,masked to the preoperative refraction and type of surgery,refracted the patients in the same room with the same light adjusted to mesopic conditions. Three months postoperatively,a complete ocular examination including corneal topography was performed in all patients.
Statistical Analysis The Statview+Graphics software (Abacus Concept Inc., Cupertino, CA, USA) was used for the statistical analyses, using a two-tailed unpaired Student’s t-test and linear regression analysis when appropriate. A P value <0.05 was considered significant. The data are expressed as the mean±standard deviation (SD). Although the minimum angle of resolution values of all visual acuity (VA) tests were used for the statistical analyses, we converted them to Snellen quotation(decimal scale) throughout the text using a visual acuity conversion chart.
In order to evaluate the effect of age on the visual and refractive results, the patients were divided into two groups, in accordance to the age-based nomogram applied. One group included allParameters Mechanical LASIK group Femtosecond LASIK group Ppatients 18 to 40y, and the other group included all patients over 40y.
Table 1 Preoperative refractive data of 3071 eyes of patients aged 18 to 40y who had undergone LASIK for the correction of myopia mean±SD (range)
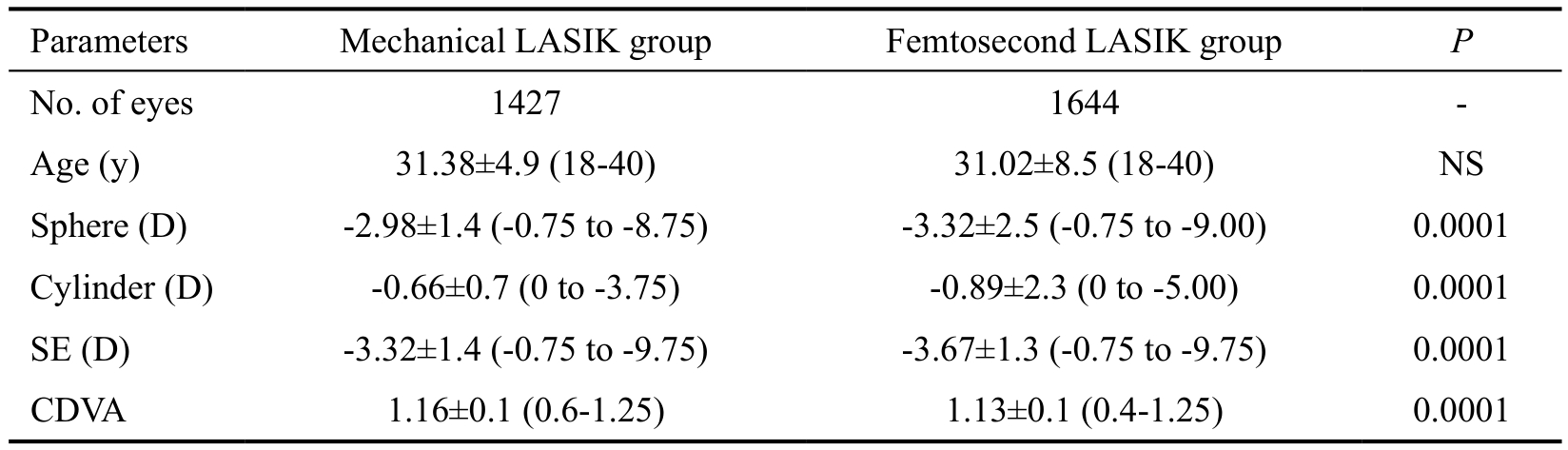
NS: Not significant; SE: Spherical equivalent; CDVA: Corrected distance visual acuity.
Parameters Mechanical LASIK group Femtosecond LASIK group P No. of eyes 1427 1644 -Age (y) 31.38±4.9 (18-40) 31.02±8.5 (18-40) NS Sphere (D) -2.98±1.4 (-0.75 to -8.75) -3.32±2.5 (-0.75 to -9.00) 0.0001 Cylinder (D) -0.66±0.7 (0 to -3.75) -0.89±2.3 (0 to -5.00) 0.0001 SE (D) -3.32±1.4 (-0.75 to -9.75) -3.67±1.3 (-0.75 to -9.75) 0.0001 CDVA 1.16±0.1 (0.6-1.25) 1.13±0.1 (0.4-1.25) 0.0001
Table 2 Preoperative refractive data of 755 eyes of patients over 40y who had undergone LASIK for the correction of myopia mean±SD (range)

NS: Not significant; SE: Spherical equivalent; CDVA: Corrected distance visual acuity.
No. of eyes 298 457 -Age (y) 46.26±4.7 (41-61) 46.09±5.1 (41-66) NS Sphere (D) -3.06±1.4 (-0.75 to -8.25) -3.29±2.3 (-0.75 to -9.25) NS Cylinder (D) -0.75±0.7 (0 to -4.00) -1.11±1.1 (0 to -5.00) 0.001 SE (D) -3.41±1.5 (-0.75 to -9.25) -3.83±2.3 (-0.75 to -9.75) 0.001 CDVA 1.13±0.1 (0.6-1.25) 1.08±0.2 (0.4-1.25) 0.02
RESULTS
A total of 3826 myopic eyes were included in the study (1725 eyes treated with mechanical LASIK and 2101 eyes treated with FS-LASIK).
The preoperative data from the two age groups are shown in Tables 1 and 2. Because of the large number of eyes included in the group of patients aged 18 to 40y, the statistical analyses identified as statistically significant differences in some of the preoperative data between groups (CDVA, and preoperative refractive error) even if these differences were minute and subsequently, not clinically relevant. The same argument should be applied to the group of patients aged over 40y. Due to large number of eyes included in the study(755 eyes), the statistical analyses identified as statistically significant differences in some of the preoperative data between groups (CDVA, cylinder and spherical equivalent) even if these differences were minute and subsequently, not clinically relevant.
Three months postoperatively, linear regression analysis showed a significant correlation between age and postoperative spherical equivalent (SE) after mechanical LASIK (P=0.006,r2=0.004) and after FS-LASIK (P=0.0001, r2=0.02); i.e.LASIK performed with an MM or an FS laser tended to undercorrect myopia with aging (Figure 1).

Figure 1 Scatterplot of the regression analysis between age and the 3-month postoperative spherical equivalent refraction in 1725 eyes treated with mechanical LASIK (A) and 2101 eyes treated with femtosecond LASIK (B) to correct myopia.
Table 3 Refractive outcomes 3-month postoperative of patients aged 18 to 40y that underwent LASIK for the correction of myopia mean±SD (range)
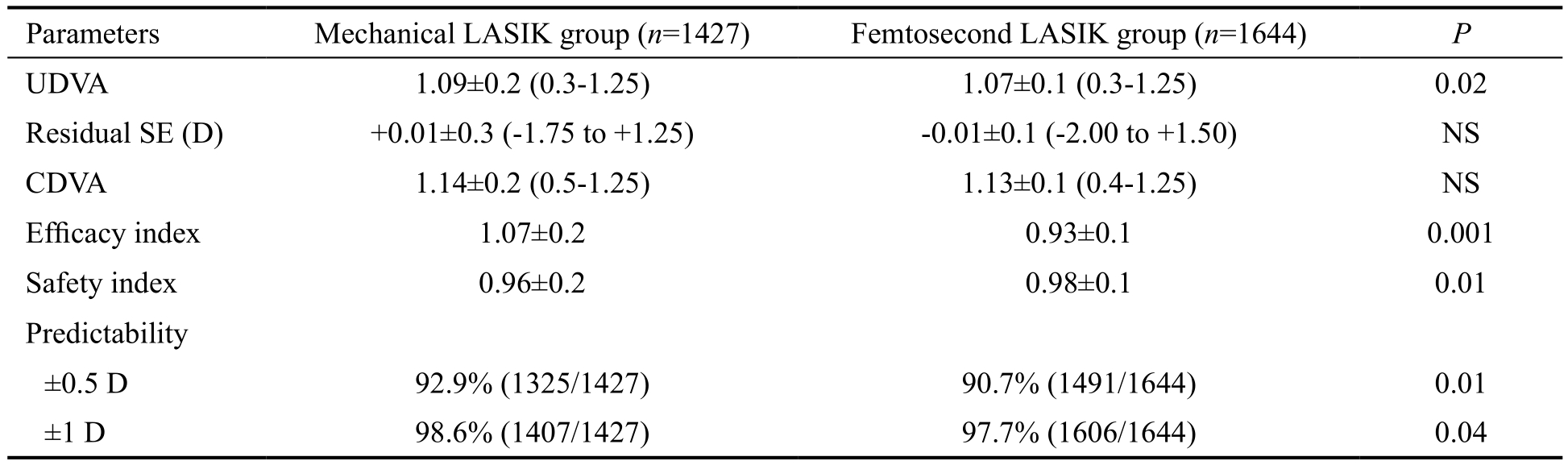
NS: Not significant; UDVA: Uncorrected distance visual acuity; SE: Spherical equivalent; CDVA: Corrected distance visual acuity.
Parameters Mechanical LASIK group (n=1427) Femtosecond LASIK group (n=1644) P UDVA 1.09±0.2 (0.3-1.25) 1.07±0.1 (0.3-1.25) 0.02 Residual SE (D) +0.01±0.3 (-1.75 to +1.25) -0.01±0.1 (-2.00 to +1.50) NS CDVA 1.14±0.2 (0.5-1.25) 1.13±0.1 (0.4-1.25) NS Efficacy index 1.07±0.2 0.93±0.1 0.001 Safety index 0.96±0.2 0.98±0.1 0.01 Predictability±0.5 D 92.9% (1325/1427) 90.7% (1491/1644) 0.01±1 D 98.6% (1407/1427) 97.7% (1606/1644) 0.04
Regarding accuracy, linear regression analysis showed a significant correlation between age and efficacy index after mechanical LASIK (P=0.001, r2=0.006) and FS-LASIK(P=0.0001, r2=0.01); i.e. LASIK tended to provide less efficacy with aging, independently of the technique used to create the flap (Figure 2).
Regarding safety, linear regression analysis showed a significant correlation between age and safety index after mechanical LASIK (P=0.0001, r2=0.05); i.e. mechanical LASIK tended to provide less safety with aging. No significant correlation was found between age and the safety index in the FS-LASIK group.
We also found that the predictability of LASIK was significantly higher in the group of younger patients, independently of the technique used to create the flap. Therefore, 92.9% of eyes of patients aged 18 to 40y versus 81.9% of eyes of patients older than 40y were within ±0.5 D of emmetropia in the mechanical LASIK group (P=0.001); and 90.7% of eyes of patients 18-40y versus 83.1% of eyes of patients >40y were within ±0.5 D of emmetropia in the FS-LASIK group (P=0.001).
Table 3 shows the visual and refractive results 3mo postoperatively after mechanical and FS-LASIK in patients aged 18 to 40y. No significant differences were found in the residual refractive error or CDVA between techniques. The postoperative UDVA and the efficacy index were significantly better in the mechanical LASIK group 3mo postoperatively,although the differences between the groups were very small,and probably not clinically relevant. The safety indexes were high with both techniques but significantly (P=0.01) better in the FS-LASIK group. Change in lines of CDVA after 3mo of follow-up is shown in Figure 3.
More eyes in the mechanical LASIK group (92.9%) than in the FS-LASIK group (90.7%) were within 0.5 D of emmetropia(P=0.01), and more eyes in the mechanical LASIK group(98.6%) than in the FS-LASIK group (97.7%), were within 1.00 D of emmetropia (P=0.04) 3mo postoperatively; i.e.mechanical LASIK provided slightly better predictability than FS laser when correcting myopia in young patients.Predictability after 3mo of follow-up is shown in Figure 4.
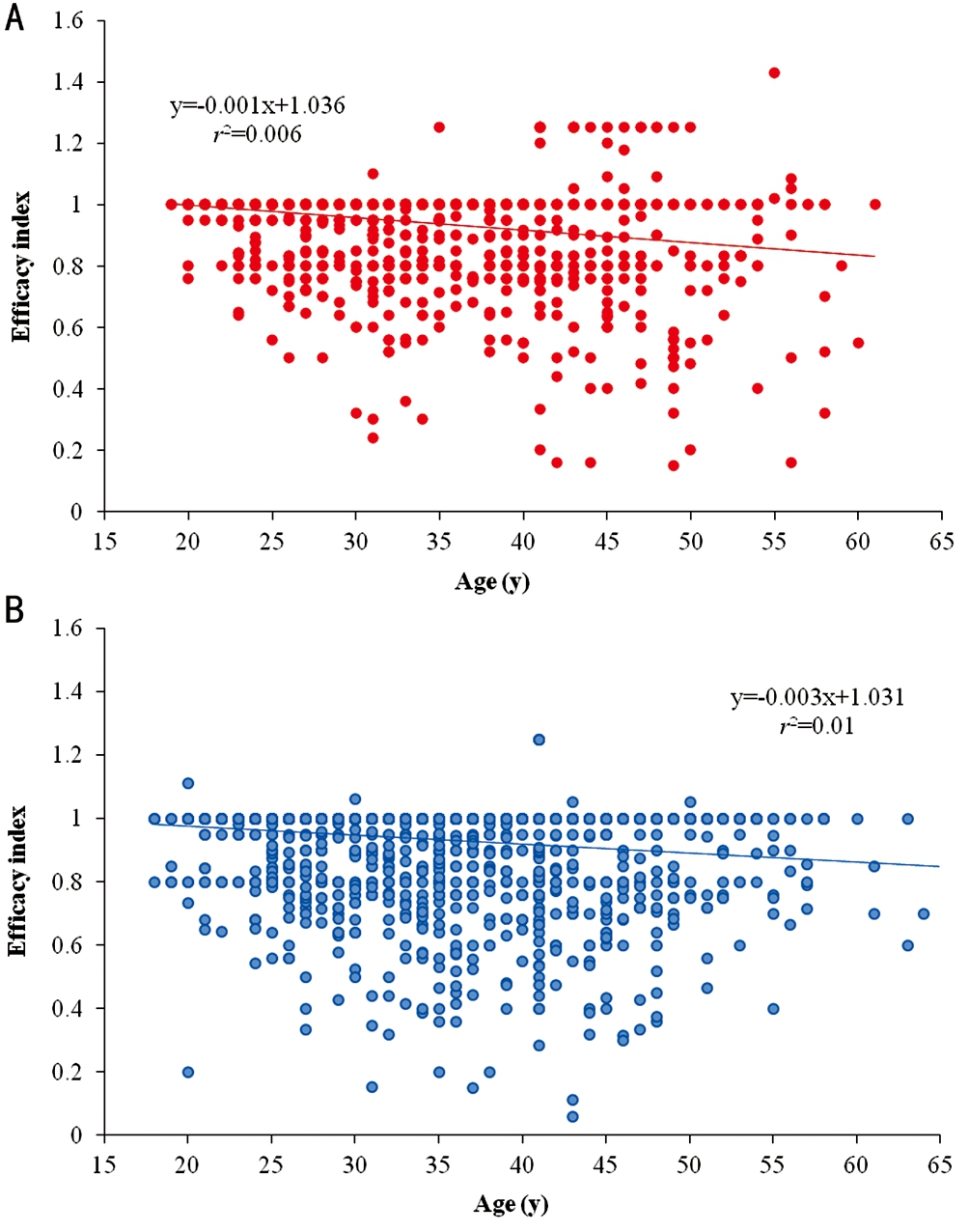
Figure 2 Scatterplot of the regression analysis between age and the efficacy index of LASIK performed with a mechanical microkeratome(A) or a femtosecond laser (B) for the correction of myopia.
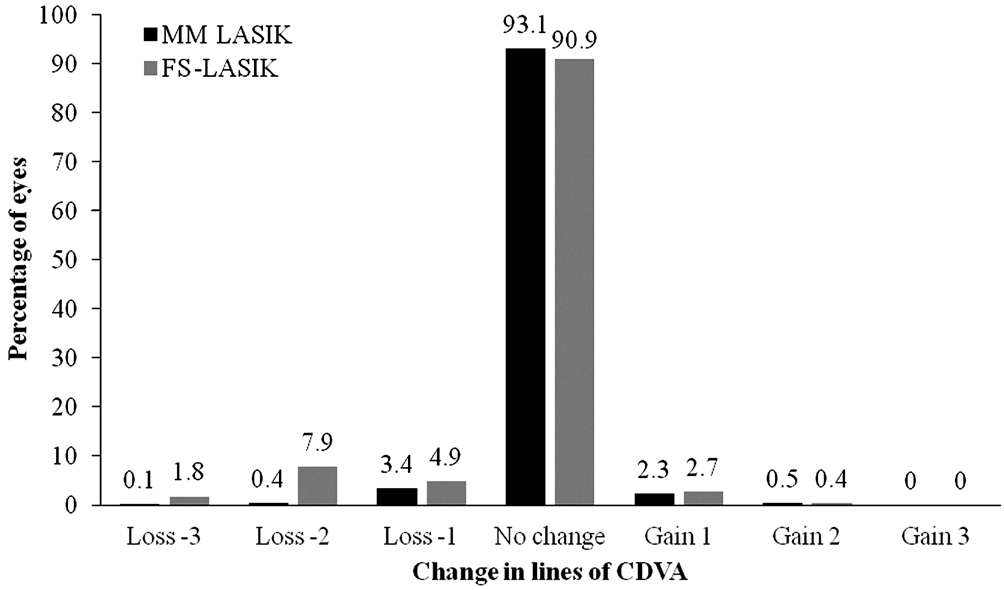
Figure 3 Changes in lines of corrected distance visual acuity after mechanical versus femtosecond LASIK in patients aged 18 to 40y CDVA: Corrected distance visual acuity; MM: Mechanical microkeratome; FS: Femtosecond.
Table 4 Refractive outcomes of postoperative 3-month in patients over 40y that underwent LASIK for the correction of myopia mean±SD (range)
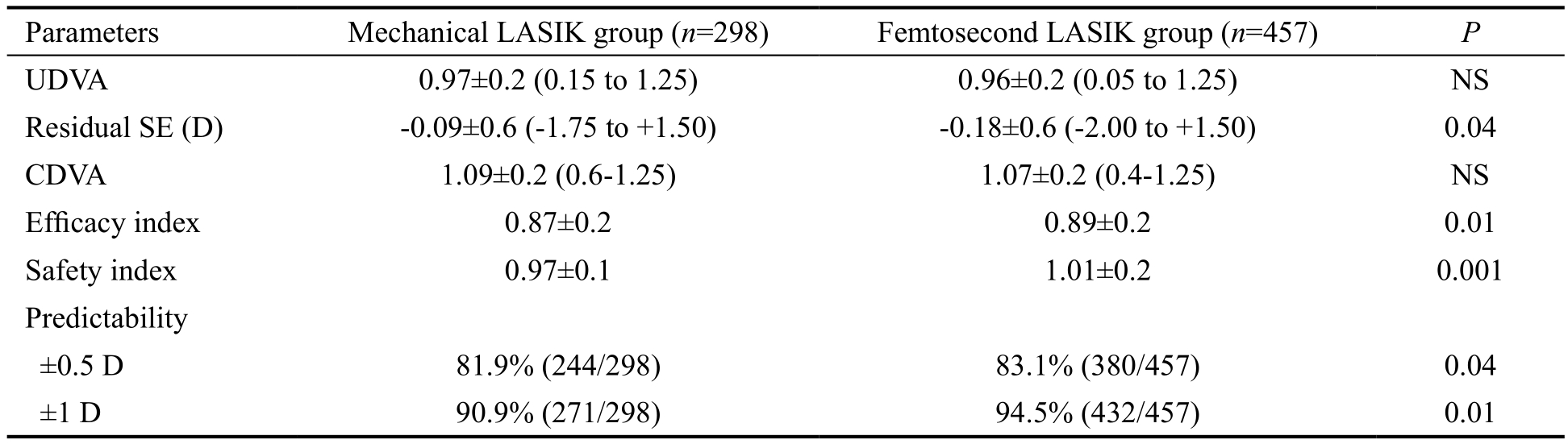
NS: Not significant; UDVA: Uncorrected distance visual acuity; SE: Spherical equivalent; CDVA: Corrected distance visual acuity.
Parameters Mechanical LASIK group (n=298) Femtosecond LASIK group (n=457) P UDVA 0.97±0.2 (0.15 to 1.25) 0.96±0.2 (0.05 to 1.25) NS Residual SE (D) -0.09±0.6 (-1.75 to +1.50) -0.18±0.6 (-2.00 to +1.50) 0.04 CDVA 1.09±0.2 (0.6-1.25) 1.07±0.2 (0.4-1.25) NS Efficacy index 0.87±0.2 0.89±0.2 0.01 Safety index 0.97±0.1 1.01±0.2 0.001 Predictability±0.5 D 81.9% (244/298) 83.1% (380/457) 0.04±1 D 90.9% (271/298) 94.5% (432/457) 0.01
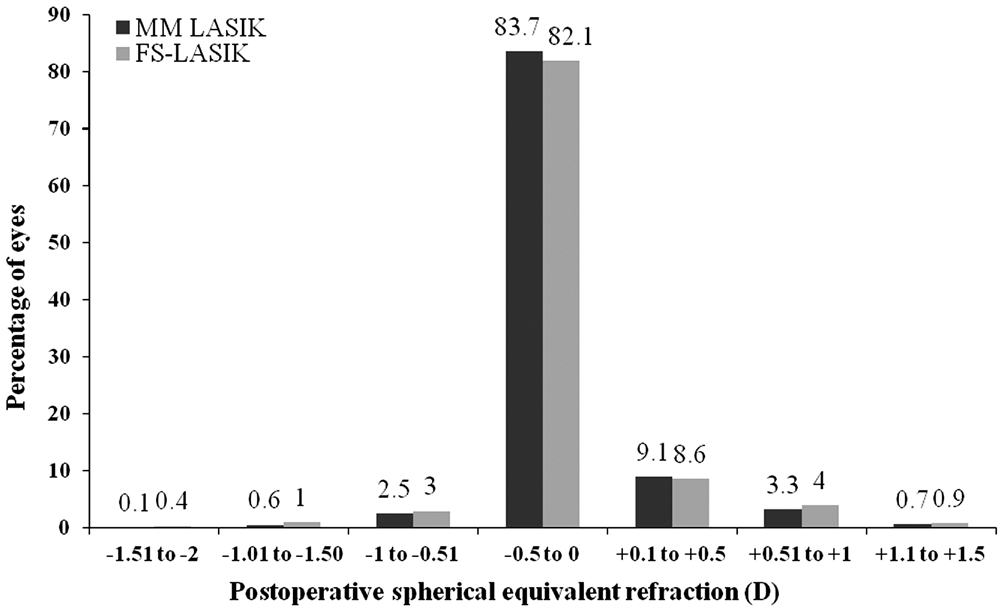
Figure 4 Comparison of predictability of LASIK performed with a mechanical microkeratome versus a femtosecond laser in patients aged 18 to 40y ±0.5 D: 92.9% MM vs 90.7% FS,P=0.01; ±1 D: 98.6% MM vs 97.7% FS, P=0.04. MM: Mechanical microkeratome; FS: Femtosecond.
Table 4 shows the visual and refractive outcomes 3mo after mechanical or FS LASIK in patients older than 40y. We found a slight tendency toward undercorrection in this age group,independently of the flap creation technique. Although no significant differences were seen in the 3-month postoperative UDVA or CDVA between the two devices, the efficacy and safety indexes were significantly better in the FS-LASIK group. Changes in lines of CDVA after 3mo of follow-up is shown in Figure 5.
In the mechanical LASIK group, 244 eyes (81.9%) compared to 380 eyes (83.1%) in the FS-LASIK group were within 0.5 D of emmetropia (P=0.04) whereas 271 eyes (90.9%) versus 432 eyes (94.5%) were within 1.00 D of emmetropia in the mechanical and FS LASIK group, respectively (P=0.01); i.e.predictability of LASIK was significantly higher when FS laser was performed in patients older than 40 years of age.Predictability of LASIK in patients over 40y is shown in Figure 6.
DISCUSSION
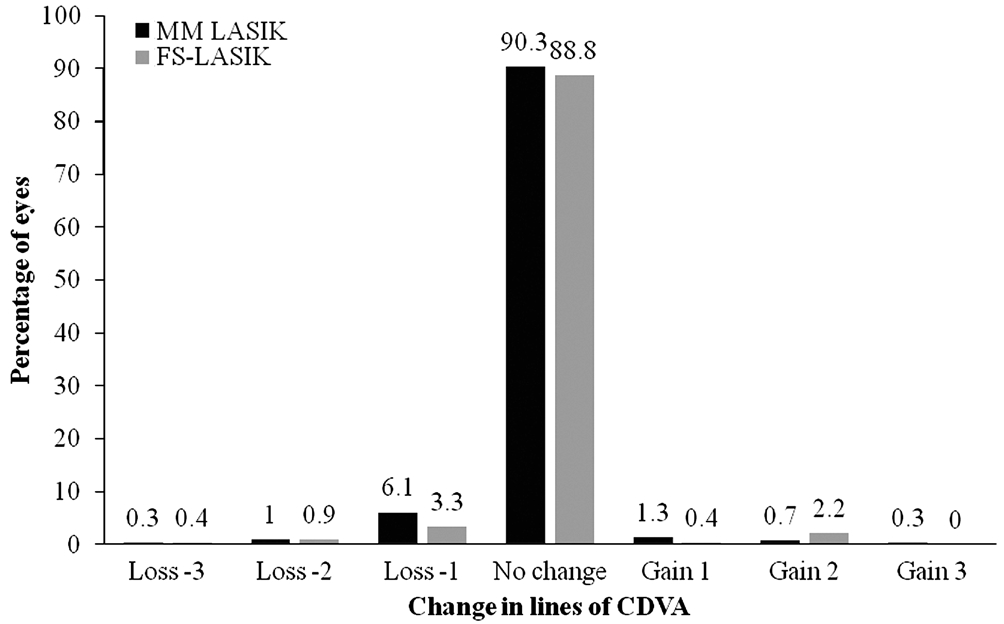
Figure 5 Changes in lines of corrected distance visual acuity after mechanical versus femtosecond LASIK in patients over 40y CDVA: Corrected distance visual acuity.
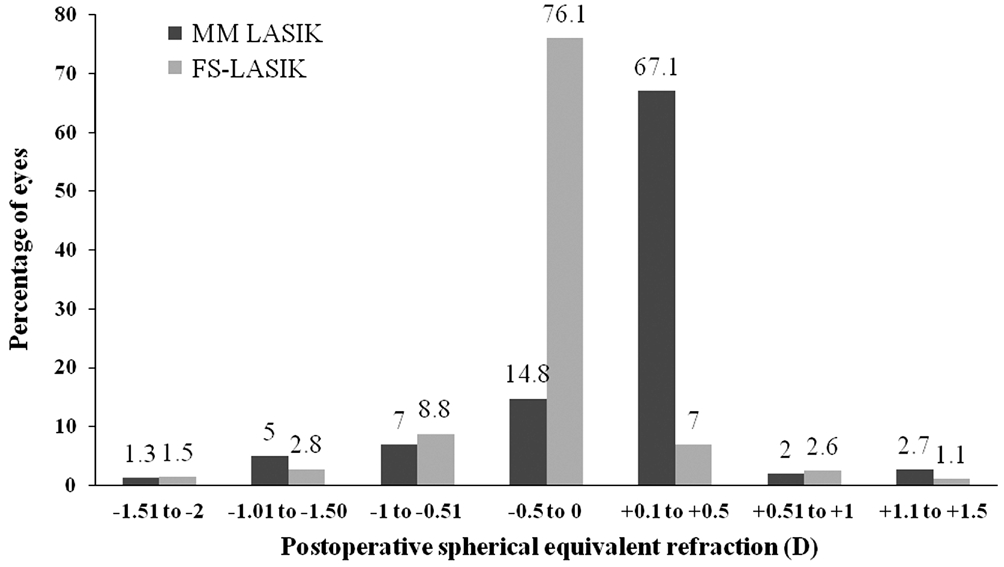
Figure 6 Comparison of predictability of mechanical LASIK versus femtosecond LASIK in patients over 40y ±0.5 D: 81.9%MM vs 83.1% FS, P=0.04; ±1 D: 90.9% MM vs 94.5% FS, P=0.01.MM: Mechanical microkeratome; FS: Femtosecond.
In the current study, a slight tendency toward undercorrection and less predictability was found with increasing age after myopic LASIK, regardless of whether mechanical or FS LASIK was performed. Regarding efficacy and predictability,the MM provided slightly but significantly better results in patients between 18 and 40y, and the FS laser did so in patients over 40y. Regarding safety, FS LASIK provided better outcomes than the MM in both age groups.
Several studies have compared LASIK outcomes with different MM to the results obtained with FS lasers to correct myopia.In fact, two published Meta-analysis[14-15] showed that FS laser and MM have comparable efficacy[14-15], safety[14-15], and predictability[15] for the correction of myopia. However, we want to remark that the vast majority of randomized controlled trials included in both Meta-analysis evaluated together young and older patients, assuming that both mechanical and FS-LASIK provided the same visual and refractive results irrespective of patient age. For this reason, we believe that the main finding of our study, which is the largest case series evaluated to date, is that the MM provided slightly but significantly better results in patients between 18 and 40y regarding efficacy and predictability, and the FS laser did so in patients over 40 years. However, we believe that because of the number of eyes included in the group of young patients(1427 eyes treated with MM vs 1644 eyes treated with FS),the statistical analyses identified significant better results in the mechanical LASIK group than in the FS-LASIK group, even if these differences are minute and subsequently not clinically relevant.
Therefore, and to the best of our knowledge, this is the first study that has focused on the effect of age on the refractive results after both procedures when correcting myopia.Although some studies have suggested that older age is a risk factor for mechanical LASIK enhancement[8-10], only the study of Ghanem et al[7] was designed specifically to analyze the visual results of LASIK in presbyopic patients. That study included 511 myopic eyes and 199 hyperopic eyes treated with two excimer lasers, the VISX Star (S4 or S2, VISX Inc., Santa Clara, CA, USA) or the Technolas 217z (Zyoptic or PlanoScan,Bausch & Lomb, Claremont, CA, USA). It is noteworthy that the authors evaluated together eyes treated with the IntraLase FS laser and the Hansatome microkeratome for flap creation,assuming that both techniques provided the same visual and refractive outcomes in presbyopic patients, as they seem to do in young myopic patients[14-16]; however, this hypothesis has not yet been proved.
It is well known that the corneal biomechanical properties change with age as a result of structural changes in the stromal collagen framework. X-ray scattering studies have shown three-dimensional growth of the collagen fibrils[17], glycationinduced cross-linking of collagen molecules[18], and changes in proteoglycan content of the interfibrillary matrix[17] in the human corneal stroma with age. All these age-related structural changes in the stromal framework may contribute separately to age-related changes in the corneal biomechanical properties,i.e. increased stiffness[19] and decreased viscoelastic properties with age[20].
On the other hand, both laser ablation and the flap modify the corneal biomechanical properties[21]. This biomechanical behavior is affected by the technology used to create the flap[22], the flap thickness, the excimer laser used for the ablation[23], and the ablation profile and depth. The FS laser is advantageous in that it creates a predictable thin and planar corneal flap, which is thought to have lower biomechanical impact on the cornea than the thicker, meniscus-shaped flap usually obtained with an MM[2-3,24]. Moreover, Kim et al[25]reported that the FS laser is likely to reliably create corneal flaps with similar thicknesses regardless of patient age.
Therefore, based on our results, the lower impact on the corneal biomechanics expected with the FS laser compared to the MM significantly affected the visual and refractive results with aging (i.e. FS laser provided significantly better efficacy, safety and predictability outcomes than the MM in presbyopic patients). However, we found a similar trend toward undercorrection with increasing age with both techniques.We are conscious that it would have been very interesting to analyze the changes in the corneal biomechanics before and after both MM and FS, but unfortunately devices such as Ocular Response Analyzer (Reichert Ophthalmic Instruments,Depew, New York) ORA or Corvis ST (Oculus Optikgeräte GmbH) were not available at the clinic at the time interval of the study.
Another factor that undermines the predictability and stability of a refractive surgical procedure is the corneal wound-healing properties[26]. Younger patients tend to have a more severe healing response, which might contribute to some regression of the treatment effect[7]. For this reason, nomogram adjustments have been proposed based on age[13] to increase the amount of correction in younger patients. In contrast, older patients may have to be undercorrected intentionally[13] to account for the diminished wound-healing response.
Nevertheless, when an age-based nomogram was applied in the current study, we detected that LASIK (regardless of whether MM or FS laser was performed) was more predictable in young patients, and a trend to undercorrection of the myopia was found after both procedures with increasing age.However, the correlations were very weak (r2=0.004 with the MM; r2=0.02 with the FS laser). For this reason, and based on our results, an overcorrection from the intended spherical correction seems to be adequate in young patients, in which this residual refractive overcorrection might not affect the efficacy index and the postoperative UDVA as a result of their preserved accommodative response. Moreover, a slight overcorrection might be desirable in very young patients in order to compensate a possible late myopic regression. In contrast, further studies are needed to better clarify if an agebased nomogram might or not be applied in patients older than 40y, in order to improve the predictability of myopic LASIK in this population.
On the other hand, even if a greater stromal inflammatory response is expected after a FS laser-created flap than after an MM-created flap[4,22,27], based on our results, no additional nomogram adjustments are needed when the FS laser is used instead of an MM.
We are aware that one limitation of the current study is that it was uncontrolled. Thus, a better study design would have been to randomize all eyes in two refractive-matched groups,one eye of each patient using a mechanical microkeratome and the fellow eye of the same patient using a femtosecond laser for LASIK flap creation. However, we want to remark that the main purpose of our study was to evaluate, in a high sample of eyes, the predictability of LASIK in different age groups when using two different technologies (MM versus FS) are used for LASIK flap creation. For this reason, we do believe that the design (nonrandomized but including a large sample size) is adequate for the purpose of the current study.
Another limitation of the current study was that we did not evaluate the induction of higher-order aberrations after both techniques. The increased ocular coma and spherical aberration expected with age[28] may be the reasons that we found a tendency toward lower safety of both techniques with age.However, lower induction of higher-order aberrations expected with the IntraLase FS laser would explain why this technique provides slightly better safety than the Moria microkeratome.The third limitation was that we included only eyes with myopia. Interestingly, hyperopic LASIK performed with the FS laser seemed to obtain better refractive results compared to the MM 3mo postoperatively[29]. Therefore, more studies are needed to determine whether the FS laser is or is not advantageous in terms of refractive results for treating hyperopia and high astigmatism with age.
In conclusion, according to our results, a tendency toward undercorrection and less predictability was found with aging after myopic LASIK regardless of whether the flap was created with an MM or an FS laser. However, FS laser provided significantly better results in terms of efficacy, safety and predictability compared to MM for the treatment of myopia in patients over 40y.
ACKNOWLEDGEMENTS
Authors’ contributions: Design of the study: Garcia-Gonzalez M, Teus MA; data collection: Garcia-Gonzalez M, Rodriguez-Perez I, Rodero A; analysis of the data: Garcia-Gonzalez M,Teus MA; writing the manuscript: Garcia-Gonzalez M; final revision: Garcia-Gonzalez M, Rodriguez-Perez I, Gros-Otero J, Rodero A, Teus MA.
Conflicts of Interest: Garcia-Gonzalez M, None; Gros-Otero J, None; Rodriguez-Perez I, None; Rodero A, None;Teus MA, None.
1 Alió JL, Muftuoglu O, Ortiz D, Pérez-Santonja JJ, Artola A, Ayala MJ,Garcia MJ, de Luna GC. Ten-year follow-up of laser in situ keratomileusis for myopia of up to -10 diopters. Am J Ophthalmol 2008;145(1):46-54.e1.2 Zhang Y, Chen YG, Xia YJ. Comparison of corneal flap morphology using AS-OCT in LASIK with the WaveLight FS200 femtosecond laser versus a mechanical microkeratome. J Refract Surg 2013;29(5):320-324.
3 Ahn H, Kim JK, Kim CK, Han GH, Seo KY, Kim EK, Kim TI.Comparison of laser in situ keratomileusis flaps created by 3 femtosecond lasers and a microkeratome. J Cataract Refract Surg 2011; 37(2):349-357.
4 Santhiago MR, Kara-Junior N, Waring GO 4th. Microkeratome versus femtosecond flaps: accuracy and complications. Curr Opin Ophthalmol 2014;25(4):270-274.
5 Kohnen T, Schwarz L, Remy M, Shajari M. Short-term complications of femtosecond laser-assisted laser in situ keratomileusis cuts: review of 1210 consecutive cases. J Cataract Refract Surg 2016;42(12):1797-1803.
6 Rao SN, Chuck RS, Chang AH, LaBree L, McDonnell PJ. Effect of age on the refractive outcome of myopic photorefractive keratectomy. J Cataract Refract Surg 2000;26(4):543-546.
7 Ghanem RC, de la Cruz J, Tobaigy FM, Ang LP, Azar DT. LASIK in the presbyopic age group: safety, efficacy, and predictability in 40- to 69-yearold patients. Ophthalmology 2007;114(7):1303-1310.
8 Mimouni M, Vainer I, Shapira Y, Levartovsky S, Sela T, Munzer G,Kaiserman I. Factors predicting the need for retreatment after laser refractive surgery. Cornea 2016;35(5):607-612.
9 Pokroy R, Mimouni M, Sela T, Munzer G, Kaiserman I. Myopic laser in situ keratomileusis retreatment: incidence and associations. J Cataract Refract Surg 2016;42(10):1408-1414.
10 Kruh JN, Garrett KA, Huntington B, Robinson S, Melki SA. Risk factors for retreatment following myopic LASIK with femtosecond laser and custom ablation for the treatment of myopia. Semin Ophthalmol 2017;32(3):316-320.
11 Bailey MD, Mitchell GL, Dhaliwal DK, Boxer Wachler BS, Zadnik K.Patient satisfaction and visual symptoms after laser in situ keratomileusis.Ophthalmology 2003;110(7):1371-1378.
12 Pop M, Payette Y. Risk factors for night vision complaints after LASIK for myopia. Ophthalmology 2004;111(1):3-10.
13 Luger MH, Ewering T, Arba-Mosquera S. Influence of patient age on high myopic correction in corneal laser refractive surgery. J Cataract Refract Surg 2013;39(2):204-210.
14 Zhang ZH, Jin HY, Suo Y, Patel SV, Montés-Micó R, Manche EE,Xu X. Femtosecond laser versus mechanical microkeratome laser in situ keratomileusis for myopia: Meta analysis of randomized controlled trials.J Cataract Refract Surg 2011;37(12):2151-2159.
15 Chen S, Feng Y, Stojanovic A, Jankov MR 2nd, Wang Q. IntraLase femtosecond laser vs mechanical microkeratomes in LASIK for myopia:a systematic review and meta-analysis. J Refract Surg 2012;28(1):15-24.
16 Cosar CB, Gonen T, Moray M, Sener AB. Comparison of visual acuity,refractive results and complications of femtosecond laser with mechanical microkeratome in LASIK. Int J Ophthalmol 2013;6(3):350-355.
17 Daxer A, Misof K, Grabner B, Ettl A, Fratzl P. Collagen fibrils in the human corneal stroma: structure and aging. Invest Ophthalmol Vis Sci 1998;39(3):644-648.
18 Malik NS, Moss SJ, Ahmed N, Furth AJ, Wall RS, Meek KM. Ageing of the human corneal stroma: structural and biochemical changes. Biochim Biophys Acta 1992;1138(3):222-228.
19 Knox Cartwright NE, Tyrer JR, Marshall J. Age-related differences in the elasticity of the human cornea. Invest Ophthalmol Vis Sci 2011;52(7):4324-4329.
20 Kamiya K, Shimizu K, Ohmoto F. Effect of aging on corneal biomechanical parameters using the ocular response analyzer. J Refract Surg 2009;25(10):888-893.
21 Dupps WJ Jr, Roberts C. Effect of acute biomechanical changes on corneal curvature after photokeratectomy. J Refract Surg 2001;17(6):658-669.
22 Javaloy Estañ J, Vidal MT, Quinto A, De Rojas V, Alió JL. Quality assessment model of 3 different microkeratomes through confocal microscopy. J Cataract Refract Surg 2004;30(6):1300-1309.
23 Waheed S, Chalita MR, Xu M, Krueger RR. Flap-induced and laserinduced ocular aberrations in a two-step LASIK procedure. J Refract Surg 2005;21(4):346-352.
24 Ortiz D, Alió JL, Piñero D. Measurement of corneal curvature change after mechanical laser in situ keratomileusis flap creation and femtosecond laser flap creation. J Cataract Refract Surg 2008;34(2):238-242.
25 Kim CY, Song JH, Na KS, Chung SH, Joo CK. Factors influencing corneal flap thickness in laser in situ keratomileusis with a femtosecond laser. Korean J Ophthalmol 2011;25(1):8-14.
26 Dupps WJ Jr, Wilson SE. Biomechanics and wound healing in the cornea. Exp Eye Res 2006;83(4):709-720.
27 Netto MV, Mohan RR, Medeiros FW, Dupps WJ Jr, Sinha S, Krueger RR, Stapleton WM, Rayborn M, Suto C, Wilson SE. Femtosecond laser and microkeratome corneal flaps: comparison of stromal wound healing and inflammation. J Refract Surg 2007;23(7):667-676.
28 Amano S, Amano Y, Yamagami S, Miyai T, Miyata K, Samejima T, Oshika T. Age-related changes in corneal and ocular higher-order wavefront aberrations. Am J Ophthalmol 2004;137(6):988-992.
29 Antonios R, Arba Mosquera S, Awwad ST. Hyperopic laser in situ keratomileusis: comparison of femtosecond laser and mechanical microkeratome flap creation. J Cataract Refract Surg 2015;41(8):1602-1609.