INTRODUCTION
Silicone oil (SO) has been commonly used as a longterm tamponade agent after pars plana vitrectomy for more than fifty years[1-2]. Although SO endotamponade acts effectively for retinal reattachment, the occurrence of postoperative complications was one of the main concerns for the surgeons. The well-known complications of SO included:secondary glaucoma, cataract formation/deterioration, bandshaped degeneration of the cornea, emulsification, migration to the anterior chamber or subretinal space, retinal toxicity,etc[1,3-11]. Therefore, SO removal is usually scheduled once anatomic success is achieved, or at the inevitable occurrence of complication. The most advised time to have SO removal is 4-6mo after SO injection[1,5,9,12-14]. In our clinical practice two years ago, we noticed that the occurrence of SO emulsification became earlier and more frequent than before.SO emulsification has been found to be related with various factors, including intravitreal hemorrhage and inflammatory reaction, etc[1,4,12,15-17]. Although SO emulsification is an inherent problem if it remains intravitreally for prolonged duration, the earlier occurrence of which would cause more unscheduled surgical interventions and possibly unsatisfactory retinal reattachment. Therefore, we conducted the current study to find out the factors related to earlier SO emulsification.
SUBJECTS AND METHODS
Ethical Approval The study was approved by the Institutional Review Board of Zhongshan Ophthalmic Center affiliated to Sun Yat-sen University (Guangzhou, China), and performed in accordance with the World Medical Association’s Declaration of Helsinki. Informed consent was waived due to the retrospective nature of the study.
SO emulsification was defined as the appearance of significant emulsified droplets (by fundoscopy) in the vitreous cavity when the eyes were currently tamponaded with SO. And earlier SO emulsification in our current study was limited within six months after primary SO injection. We retrospectively examined the files of all patients who underwent both SO injection and SO removal (from August 2014 to August 2015).Patients undergone SO removal because of emulsification were included. Exclusion criteria were as follows: SO removal for various postoperative complications other than emulsification within 6mo after SO injection; undergone other ophthalmic surgeries during the period between primary SO injectionand removal; scheduled SO removal when complete retinal reattachment was achieved within 6mo after SO injection; with uncomplete follow-up data.
Table 1 The statistical analysis of the brand and type of SO related with earlier SO emulsification
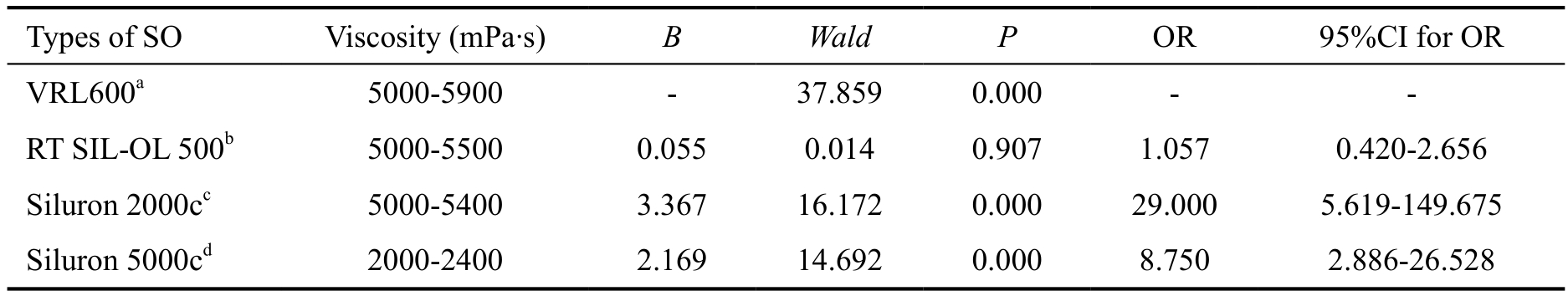
aBausch&Lomb®; Bausch&Lomb, Incorporated; Waterford, Ireland; bCarl Zeiss®; Carl Zeiss Meditec AG; Berlin, Germany;cGueder®; Fluoron GmbH; Ulm, Germany; dGueder®; Fluoron GmbH; Ulm, Germany.
Types of SO Viscosity (mPa·s) B Wald P OR 95%CI for OR VRL600a 5000-5900 - 37.859 0.000 - -RT SIL-OL 500b 5000-5500 0.055 0.014 0.907 1.057 0.420-2.656 Siluron 2000cc 5000-5400 3.367 16.172 0.000 29.000 5.619-149.675 Siluron 5000cd 2000-2400 2.169 14.692 0.000 8.750 2.886-26.528
All primary vitrectomy with SO injection surgeries were done by the surgeons in our hospital. Standard 3-port pars plana vitrectomy was performed with the Alcon Constellation(Alcon Laboratories, Fort Worth, TX, USA) or Bausch &Lomb’s Stellaris (Bausch & Lomb Incorporated, Rochester,New York, USA) vitrectomy platform. Noncontact wide-angle viewing system (Carl Zeiss Meditec AG, Jena, Germany)or contact lens was used on all patients according to the surgeons’ using habit. According to the patients’ file records,the possible related factors were collected for further analysis.We collected the following independent factors: macula status(on/off), concomitant phacoemulsification with the surgery of SO tamponading, concomitant status of proliferative vitreoretinopathy (PVR), combined surgery of retinotomy,time to have emulsification (<6mo or ≥6mo after primary SO injection), route of SO injection (anterior or posterior), lens status (aphakic, pseudophakic or phakic), anesthesia (local or general), brands and type of SO, with/without episcleral cryotherapy, with/without hypertension, with/without diabetes,with/without intraoperative use of triamcinolone acetonide.
All data were analyzed using the SPSS 19.0 statistical software(SPSS Inc., Chicago, IL, USA). Binary logistic regression and Chi-square analysis were used to analyze the factors related to earlier SO emulsification as appropriate. All the continuous data were expressed as mean±standard deviation (SD). P values <0.05 was considered statistically significant.
RESULTS
Six hundred and fifty-seven consecutive patients who underwent SO removal in our hospital between the period mentioned above were reviewed. Finally, 182 ones (136 males and 46 females) were eligible and recruited into the study, with the mean age of 38.6±17.83y. Among the recruited cases, 81 ones began to have SO emulsification more than six months after primary SO injection, and the other 101 ones less than six months.Emulsified SO in the anterior chamber was detected in 82 eyes(45.05%). Phacoemulsification was performed in 34 patients(18.68%) with the surgery of SO tamponade. The percentage to have concomitant retinotomy was 6.59% (12 patients).
Among all the patients, 52 eyes (28.6%) were found to be macula-off before surgery of SO tamponading, and 80 eyes(44.0%) were with PVR. Elevated intraocular pressure(IOP) was measured in 20 eyes (11.0%) when found to have emulsified SO in the vitreous cavity. Totally 26 eyes (14.3%)underwent the primary surgery of SO tamponading for reoperation due to recurrent retinal detachment.
We found gender had no statistically significant role in the time (<6mo or ≥6mo after primary SO injection; χ2=0.026,P=0.505). Binary logistic regression revealed that type and brand of SO was the statistically significant factor related to earlier SO emulsification (χ2=55.136, P<0.001). The results of the logistic regression were listed in Table 1.
DISCUSSION
Emulsification of SO can lead to various complications,including glaucoma, inflammation, and PVR formation and progression[1,5,8-10]. The current study is up to date the first one reporting earlier SO emulsification related to one specific brand and type of SO. SO was firstly introduced as an internal tamponading agent in 1961[2]. It has served as an invaluable tool to the retinal surgeon in the surgical treatment of vitreoretinal disorders under complex status, especially those with severe PVR.
Nowadays, various types and brands of SO have obtained approval for ophthalmic use. However, there is still no international standard for the manufacturing process and the purity grading of SO product. In China, multiple kinds of SO are being used in the large number of vitreoretinal patients[5,13-14,18-19]. SO is generally classified into different types according to their average viscosities and specific gravities.While we should keep in mind that the commercially available SOs are of mixture of compounds, viscosity is judged by measuring the overall average value. The lower-molecularweight SO tends to occur emulsification, which is consistent with the result in the current study[1,4,17].
Emulsification of SO is an inherent problem. Emulsification is reported to occur as quickly as 1wk after the initial surgery[1].Although SO emulsification seems an inevitable postoperative complication of SO tamponading, it should be noted that earlier emulsification would be a negative effect for the vitreoretinal recovery. The ideal timing for SO emulsification is generally considered as more than three months after surgery.We should have some physic knowledge of SO emulsification at the current scenario. Dispersion of SO refers to the breaking up of large bubbles into the smaller ones. Emulsifications only occurs when surface tension of the droplets is reduced in the presence of surfactants. The potential surfactants include phospholipid, protein, lipoprotein. Therefore, the current study collected the general characteristics and specific factors into considerations, to find out the underlying factor related to the phenomenon of earlier SO emulsification. Finally, we found out that the Siluron 2000c (Gueder®; Fluoron GmbH; Ulm,Germany) SO was one independent factor related with earlier emulsification of SO. The underlying mechanism is warranted further investigations. Apart from that, other unusual but challenging complications of SO tamponade should be paid attention[20-22].
Although we have tried our best effort to find out the independent factor causing the unfavorable complication,there are several limitations of the current study should be acknowledged. As earlier emulsification of SO is a unfavorable condition, the current study could only be designed as a retrospective one. Prospective or randomized design was not acceptable at that scenario. It would not be highly convincing to have the conclusion that one specific type of SO was directly correlated with earlier emulsification of SO in the current study, due to the known limitations of the current study.
In conclusion, the current study revealed that the Siluron 2000c (Gueder®; Fluoron GmbH; Ulm, Germany) SO is the independent significant factor related to earlier SO emulsification in our hospital. The application of it has be paused after we observed this unusual phenomenon. We are looking forwards to a multi-center analysis of different brands and types of SO to have better conclusion of the factors related to earlier emulsification of SO.
ACKNOWLEDGEMENTS
Conflicts of Interest: Ni Y, None; Fang H, None; Zhang X,None; Lin XF, None; Guo WJ, None.
1 Feng X, Li C, Zheng Q, Qian XG, Shao W, Li Y, Li W, Yin L,Wang Y, Gao Q. Risk of silicone oil as vitreous tamponade in pars plana vitrectomy: a systematic review and meta-analysis. Retina 2017;37(11):1989-2000.
2 Cibis PA, Becker B, Okun E, Canaan S. The use of liquid silicone in retinal detachment surgery. Arch Ophthalmol 1962;68:590-599.
3 Kaneko H, Matsuura T, Takayama K, Ito Y, Iwase T, Ueno S, Nonobe N, Yasuda S, Kataoka K, Terasaki H. Increased retinal thinning after combination of internal limiting membrane peeling and silicone oil endotamponade in proliferative diabetic retinopathy. Ophthalmologica 2017;238(4):226-235.
4 Kawaguchi M. Silicone oil emulsions stabilized by polymers and solid particles. Adv Colloid Interface Sci 2016;233:186-199.
5 Zhang Z, Wei Y, Jiang X, Qiu S, Zhang S. A machine-independent method to have active removal of 5000 centistokes silicone oil using plastic infusion tube and 23-gauge microcannulas. BMC Ophthalmol 2015;15:114.
6 Moya R, Chandra A, Banerjee PJ, Tsouris D, Ahmad N, Charteris DG.The incidence of unexplained visual loss following removal of silicone oil. Eye (Lond) 2015;29(11):1477-1482.
7 Ghoraba HH, Ghali AA, Mansour HO. Aqueous misdirection following pars plana vitrectomy and silicone oil injection. Clin Ophthalmol 2015;9:903-906.
8 Romano V, Cruciani M, Semeraro F, Costagliola C, Romano MR.Development of ocular hypertension secondary to tamponade with light versus heavy silicone oil: A systematic review. Indian J Ophthalmol 2015;63(3):227-232.
9 Tavares RLP, Nóbrega MJ, Nóbrega FAJ, De Novelli FJ, De Oliveira CAC. Timing and outcomes after silicone oil removal in proliferative vitreoretinopathy: a retrospective clinical series. Int J Retina Vitreous 2015;1:2.10 Wang L, Liu J, Lu T. Clinical analysis of early and mid-late elevated intraocular pressure after silicone oil injection. Eye Sci 2014;29(2):85-89.
11 Henderer JD, Budenz DL, Flynn HW Jr, Schiffman JC, Feuer WJ,Murray TG. Elevated intraocular pressure and hypotony following silicone oil retinal tamponade for complex retinal detachment: incidence and risk factors. Arch Ophthalmol 1999;117(2):189-195.
12 Chan YK, Cheng HC, Wu J, Tang YHM, Chan ST, Wong D, Shum HC. A perfluorobutylpentane (F4H5)-based solution for the removal of residual emulsified silicone oil. Acta Ophthalmol 2018;96(1):e38-e45.
13 Zhu YC, Yuan DQ, Xie P, Liu XY, Yuan ST, Liu QH. Phacoemulsification combined with transpupillary removal of silicone oil and intracapsular intraocular lens implantation. Int J Ophthalmol 2017;10(11):1693-1697.
14 Song ZM, Hu XT, Wang L, Hu ZX, Zhao PQ, Chen D. A modified approach to actively remove high viscosity silicone oil through 23-gauge cannula. Int J Ophthalmol 2016;9(9):1294-1298.
15 Russo A, Morescalchi F, Donati S, Gambicorti E, Azzolini C,Costagliola C, Semeraro F. Heavy and standard silicone oil: intraocular inflammation. Int Ophthalmol 2018;38(2):855-867.
16 Ghoraba HH, Zaky AG, Abd Al Fatah HM, El Gemai EEDM, Heikal MA. Sticky silicone oil. Retina 2017;37(8):1599-1606.
17 Zafar S, Shakir M, Mahmood SA, Amin S, Iqbal Z. Comparison of 1000-centistoke versus 5000-centistoke silicone oil in complex retinal detachment surgery. J Coll Physicians Surg Pak 2016;26(1):36-40.
18 Liu Z, Fu G, Liu A. The relationship between inflammatory mediator expression in the aqueous humor and secondary glaucoma incidence after silicone oil tamponade. Exp Ther Med 2017;14(6):5833-5836.
19 Li YF, Li DJ, Wang ZY, Chen W, Zhao Q, Cui R, Shen L, Yang WL.Ultrasonic diagnosis of retinal detachment in eyes with silicone oil tamponade. Zhonghua Yan Ke Za Zhi 2017;53(11):842-846.
20 Bobba S, Fox OJK, Lee MB, Parker R, Jain NS, Semmonds AK, Agar A, Francis IC. Contiguous silicone oil migration from the vitreous cavity to the optic tract. J Neuroophthalmol 2017;37(4):464-465.
21 Ali Bautista S, Wladis EJ, Farber M, Falk NS, Phelps PO. Silicone oil migration into the orbit. Orbit 2018;37(5):368-370.
22 Madanagopalan VG, Velis G, Devulapally S. Emulsified silicone oil droplets in the canal of Schlemm. Int Ophthalmol 2018;Mar 2.