Dear Editor,
W e are writing this letter to report an unexpected rare case of central retinal artery occlusion (CRAO)happened after stent-assisted coiling for internal carotid artery(ICA) aneurysm in a female patient. CRAO is a devastating ocular emergency with poor visual prognosis and no universal accepted treatment at present. CRAO is usually associated with arterial hypertension, diabetes mellitus, renal disease,ischemic heart disease, carotid artery disease and trauma[1-2].However, our case occurred accidentally following a carotid artery aneurysm surgery. The study followed the tenets of the Declaration of Helsinki and informed consent was obtained from the patient.
A 55-year-old female was diagnosed as the right ICA aneurysm identified using cerebral catheter angiography in August 2018. The size of the aneurysm was about 4.2×3.8×3.2 mm3 and its neck was 3.9 mm wide. The right ophthalmic artery(OphA) originated from the part opposite to the aneurysm at the right ICA (Figure 1A, 1B). Previously abnormal systemic or ophthalmic history was denied. When endovascular stentassisted coiling of the ICA aneurysm was performed, any surgical complications were not noticed. Intra-operative ICA angiograms demonstrated the competence of the OphA with choroidal blush after complete obliteration of the aneurysm by endovascular coils embolization (Figure 1C, 1D). Heparin infusion was continuously applied during and after the surgery.Unfortunately, when the patient woke up from general anesthesia, she noticed blurred vision with her right eye.Twelve hours after surgery, she complained about not able to see with her right eye to her attending doctor. Patient’s blood pressure, glucose, lipid and coagulation profiles, as well as her erythrocyte sedimentation rate and C-reactive protein were all checked within normal levels. Her visual acuity diminished prominently to counting fingers and lost light reflexes in her right eye. Her best-corrected visual acuity (BCVA) was 20/20(Snellen equivalent) in the left eye. Intraocular pressure was normal and the anterior segment findings were unremarkable for both eyes except no direct light reflex of the right pupil.Fundus examination of the right eye revealed retinal edema and patched cotton-wool spots in the posterior retina (Figure 2A,2B). Fundus fluorescein angiography (FFA) detected slightly delayed perfusion at the artery phase and artery branches were partially occluded at the arteriovenous phase. At the late phase,fluorescence leakage and staining occurred segmentally in arteriolae and the optic disc, which differed from complete artery block (Figure 2C-2F). Spectral domain optical coherence tomography (SD-OCT) revealed an irregular macular edema with a hyperreflective, thickened inner retina (Figure 3).Considering therapy window and side effects of intra-arterial thrombolysis, the patient was immediately given conventional treatment, including ocular massage, intraocular pressurelowering agents (Carteolol Hydrochloride, Methazolamide),oxygen inhalation, vasodilators (Nitroglycerine, Alprostadil,Cinepazide Maleate) and neuroprotective agent (Cobamamide),but these therapies did not show any positive effectiveness.One week later, edema was mostly relieved as shown in OCT images (Figure 3). However, visual acuity of her right eye remained counting fingers. The patient was asked to return for follow up, but she was not back.
Conventional treatment modalities for CRAO are widely used,although its efficacy for visual outcome has not been clearly proved[3]. On the other hand, intra-arterial and intravenous thrombolysis has demonstrated variable results for improving visual acuity. However, the use of thrombolytics in CRAO remains controversial because of its potential side effects as hemorrhagic or ischemic complications of the brain[4], as well as major methodological flaws in most of thrombolysis studies,as the absence of a well-designed randomized controlled study[5]. Therapeutic window for rescuing retinal ischemia is another important issue. Animal model studies have suggested ideal therapeutic window is less than 4h. Six-hour therapeutic window might be suggested for patients with incomplete CRAO[6].
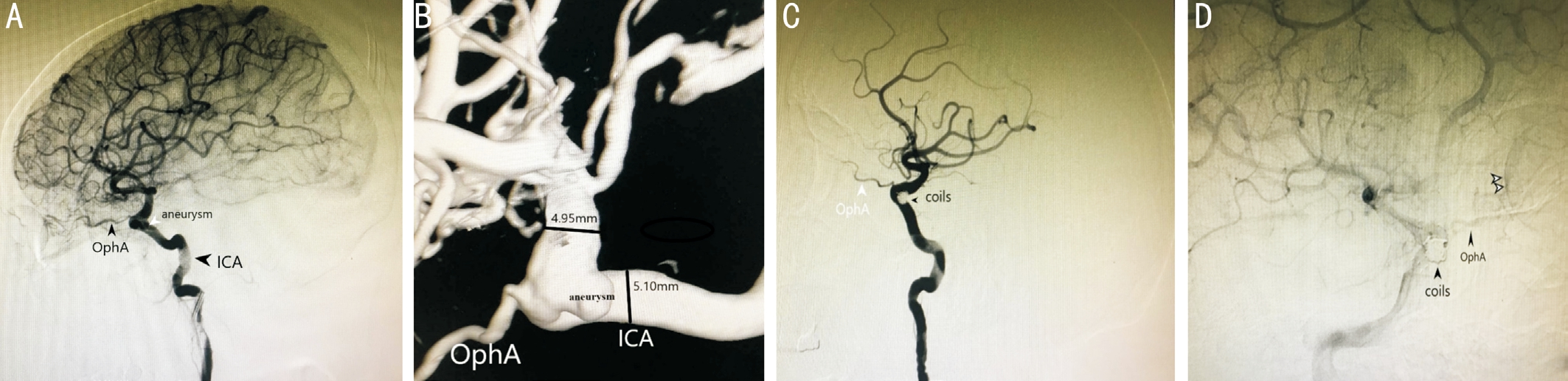
Figure 1 ICA angiograms and three-dimensional reconstructed images A: Cerebral catheter angiography shows an aneurysm in the right ICA and the OphA originates from the opposite part; B: Three-dimensional reconstructed images demonstrate a wide necked ICA aneurysm, with the size of 4.2×3.8×3.2 mm3; C, D: ICA angiograms immediately after complete obliteration of the aneurysm by endovascular coils embolization show OphA and the posterior eye bulbs, a phenomenon known as choroidal blush (two white arrowheads) proved the patency of the OphA.
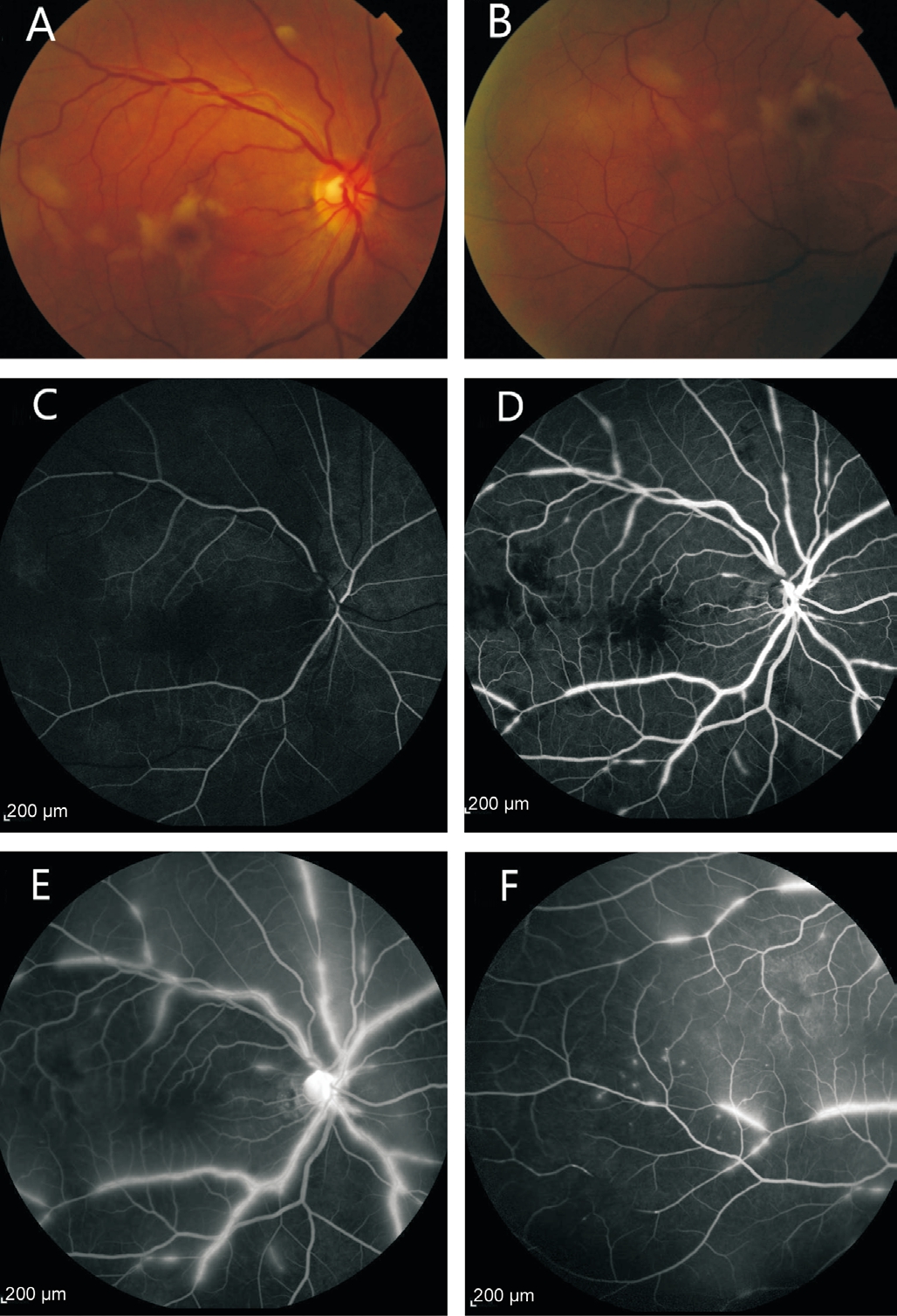
Figure 2 Fundus photography, FFA after coils embolization A, B:Color fundus photograph of the right eye shows edema and cottonwool spots in the retina; C, D: FFA detected slightly delayed perfusion at the artery phase (19s) and arteriole branches were partially occluded at the arteriovenous phase (37s); E, F: At the late phase,fluorescence leakage and staining occurred segmentally in arteriolae and the optic disc.
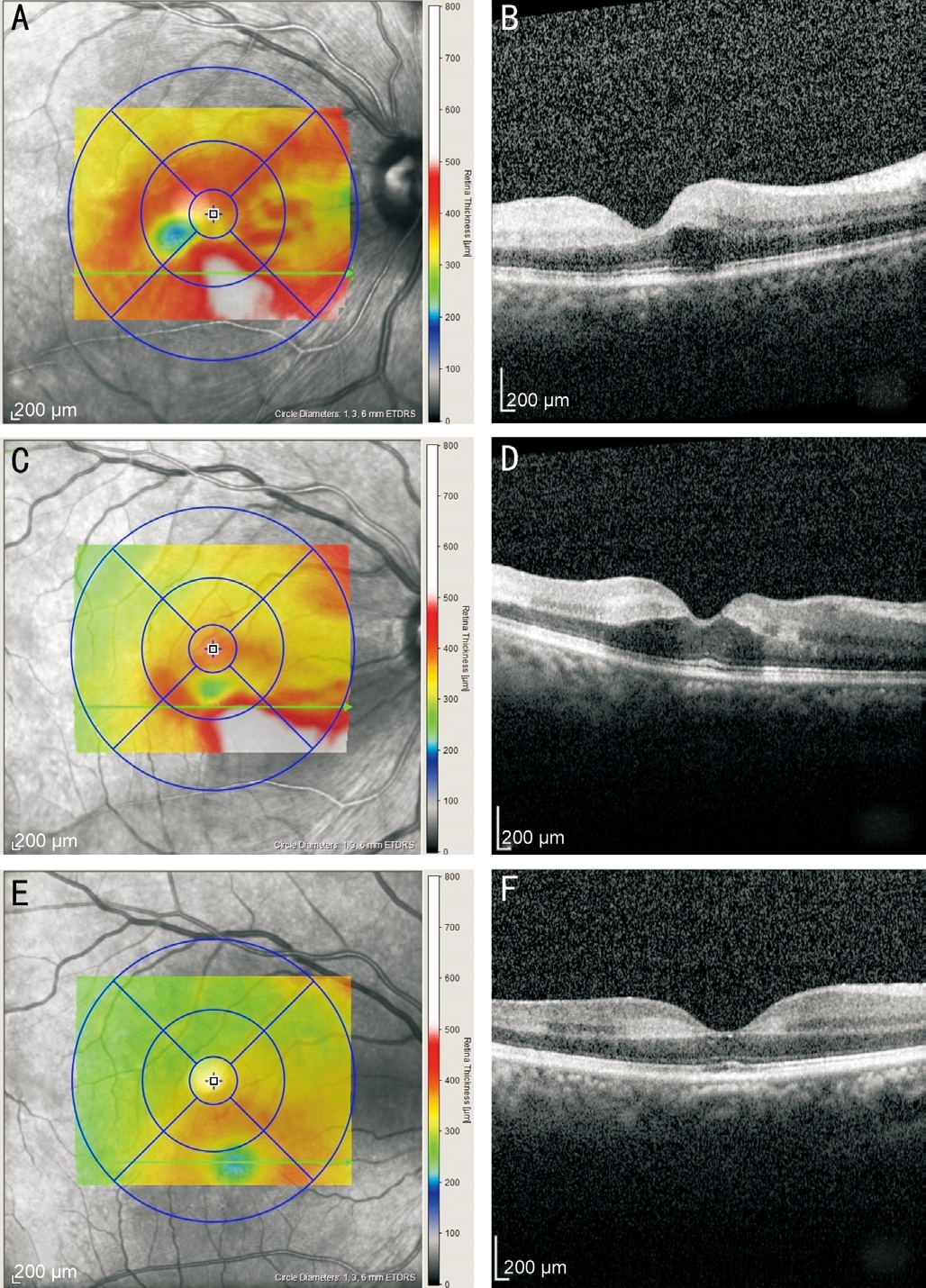
Figure 3 SD-OCT images at different stages of CRAO A, B: OCT presents an irregular macular edema with a hyperreflective, thickened inner retina before treatment; C, D: Two days after CRAO, macular thickness slightly decreased; E, F: Retinal thickness nearly recovered one week after CRAO.
CRAO caused by intracranial aneurysm embolism has rarely been reported. Kim et al[7] reported a case of CRAO associated with peripheral OphA aneurysm. Patient complained of sudden visual loss to light perception for 15h. After urgent intra-arterial thrombolysis therapy, patient visual acuity marginally improved to hand motion in 4mo follow up.
Most common complication of coil embolization for cerebral aneurysms is thrombo-embolic stroke. In rare cases, these strokes could be presented as CRAO. The visual prognosis for CRAO following coil embolization is not well established. A latest review of 9 cases demonstrated that, for patients with visual loss occurred immediately after coil embolization,their final visual acuity could virtually recover to pre-CRAO baseline. In contrast, if visual loss occurred several hours or days after surgery, visual acuity was unlikely to recover with either conventional treatment or intra-arterial thrombolysis[8].In our case, embolism from ICA aneurysm sac or microcatheter caused endothelial injury was the probable etiology. After 12h of visual loss, conventional treatment was not effective and visual acuity remained as counting fingers.
We would like to highlight that during endovascular stentassist coiling embolization of the ICA aneurysm, the risk of visual loss due to thromboembolic complications at OphA cannot be ignored, either after surgery or in the follow up period.
ACKNOWLEDGEMENTS
Conflicts of Interest: Wang YL, None; Hui YN, None;Chen R, None; Jin YY, None; Tao J, None; Zhou YM,None.
1 Hayreh SS, Podhajsky PA, Zimmerman MB. Retinal artery occlusion:associated systemic and ophthalmic abnormalities. Ophthalmology 2009;116(10):1928-1936.
2 Zvorničanin J, Kuhn F, Halilbašić M, Mušanović Z. Central retinal artery occlusion and traumatic optic neuropathy following blunt ocular trauma. Int J Ophthalmol 2018;11(5):893-897.
3 Arnold M, Koerner U, Remonda L, Nedeltchev K, Mattle HP, Schroth G, Sturzenegger M, Weber J, Koerner F. Comparison of intraarterial thrombolysis with conventional treatment in patients with acute central retinal artery occlusion. J Neurol Neurosurg Psychiatry 2005;76(2):196-199.
4 Page PS, Khattar NK, White AC, Cambon AC, Brock GN, Rai SN,James RF. Intra-arterial thrombolysis for acute central retinal artery occlusion:a systematic review and meta-analysis. Front Neurol 2018;9:76.
5 Biousse V. Thrombolysis for acute central retinal artery occlusion: is it time? Am J Ophthalmol 2008;146(5):631-634.
6 Hayreh SS. Intra-arterial thrombolysis for central retinal artery occlusion. Br J Ophthalmol 2008;92(5):585-587.
7 Kim YW, Woo SJ, Ahn J, Park KH, Kwon OK. Ophthalmic artery aneurysm: potential culprit of central retinal artery occlusion. Korean J Ophthalmol 2013;27(6):470-473.
8 Yoo M, Jin SC, Kim HY, Choi BS. Intra-arterial thrombolysis for central retinal artery occlusion after the coil embolization of paraclinoid aneurysm. J Cerebrovasc Endovasc Neurosurg 2016;18(4):369-372.