INTRODUCTION
K eratoconus is described as a bilateral, non-inflammatory,and ectatic corneal disorder. In early stages of keratoconus a satisfactory level of visual acuity can be achieved by using glasses and gas permeable contact lenses. However, corneal transplant surgery is required for patients with advanced stages of keratoconus and contact lens intolerance.
Penetrating keratoplasty (PKP) is the most commonly performed surgical option of keratoconus[1]. However, endothelial graft rejection after PKP, long-term steroid use depends on the development of secondary cataract and glaucoma complications such as the development affecting graft survival has led researchers to search for new treatments.
Anterior lamellar keratoplasty (ALK) is an alternative to PKP in keratoconus patients. Several researchers have identified ALK technique different from each other. ALK techniques aim to replace diseased corneal tissue with donor tissue. The main advantages of lamellar keratoplasty are preservation of endothelium, low risk for endothelial rejection, faster wound healing, and a short topical corticosteroid regimen. Anwar and Teichmann[2]'s big bubble deep anterior lamellar keratoplasty(DALK) aims to separete deep stroma from Descemet's membrane (DM) by creating air filled cavity. Another ALK technique used in this study is excimer laser assisted anterior lamellar technique (ELLK) that has been replaced by removal of diseased stroma lamellar donor cornea with a laser technique[3].
This study compared and evaluated the clinical outcomes of DALK and ELLK with keratoconus.
SUBJECTS AND METHODS
Ethical Approval This study was approved by the review board of Gazi University and conformed to the guidelines of the Declaration of Helsinki. An informed consent was obtained from all individual participants included in the study.
Patients In this study, clinical data of patients who underwent DALK and ELLK for treating keratoconus from 2013 to 2017 were reviewed retrospectively. Thirtyone eyes of 31 patients and twenty-six eyes of 25 patients were included in DALK and in ELLK group, respectively.The inclusion criteria were: moderate to severe keratoconus patients who had poor spectacle-visual acuity and contact lens intolerance. None of the patients had previous hydrops.Keratoconus diagnosis was based on the clinical findings of slit lamp examination, keratometric readings, and specific topographic patterns. Exclusion criteria included any coexisting ocular pathologies and the patients who had undergone previous collagen crosslinking. Preoperative and postoperative ophthalmic examinations included uncorrected visual acuity (UCVA) and best spectacle-corrected visual acuity (BSCVA), biomicroscopy of the anterior segment,tonometry, and refraction. Visual acuity was represented in decimal. Scheimpflug camera combined with Placido corneal topography (Sirius, CSO, Florence, Italy) was used for corneal measurements. Topographic data were obtained preoperatively and 1, 3, 6, 9 and 12mo after surgery.
Surgical Technique The operations were performed by same surgeons (Aydin B, Ozmen MC) under general anesthesia in the same clinic. The big-bubble technique described by Anwar and Teichmann[2] was used. A 7.5-mm diameter partial-thickness (60%-80% of stromal depth) trephination with a Hessburg-Barron suction trephine (Katena, Denville,New Jersey, USA) was performed. A 30-gauge needle bent 45 degrees with the bevel facing down was inserted into the stroma. Air was injected progressively into the stroma,in order to achieve formation of a large air bubble between the DM and posterior stroma. A peripheral paracentesis was performed, allowing some aqueous to escape and lower intraocular pressure. Viscoelastic material was injected into the space between posterior stroma and DM to maintain the space.Blunt tipped scissors were used to divide the remaining stroma into 4 quadrants, which were then removed by cutting each quadrant at the edge of the trephination, exposing the DM. A donor cornea, oversized by 0.25 mm, devoid of DM and was punched from endothelial side using Barron punch (Katena,Denville, NJ, USA). Donor cornea was sutured in place with a single running 10-0 nylon suture. In case of failure to achieve big bubble, manual dissection of stroma with blunt tipped fine scissors was performed in a way similar to the method defined by Anwar and Teichmann[2].
ELLK surgeries were performed under topical anesthesia.Phototherapeutic keratectomy ablation was applied using an MEL-70 excimer laser (Carl Zeiss Meditec). The laser settings was wavelength 193 nm, frequency 35 Hz, fluency 180 mJ/cm2 and ablation rate 0.25 µm. A 7.0 mm round stainless steel mask was placed on the cornea to create a vertical and regular edge of the ablation. The ablation depth setting ranged 120 to 200 µm and the residual corneal bed was left at least 200 µm. A 2.5 mm stromal pocket was created around the circumference of the ablation floor. Microkeratome was used for donor lamellae.Prepared donor and recipient corneal bed were washed with saline solution to remove foreign particles which could lead to formation of interface scarring. Donor cornea was secured in the recipient cornea with 10-0 running nylon suture.
Postoperative Medication and Follow-up After surgeries,topical moxifloxacin 0.5%, prednisolone acetate 1%, and preservative-free artificial tear eye drops 7 times for month were used. The eye drops were discontinued after 6mo.
All patients who received DALK or ELLK were scheduled to be followed up after 1wk, 1, 3, 6, 9 and 12mo. A detailed clinical examination was performed at every visit, including assessments of intraocular pressure, UCVA, BSCVA,refraction, graft clarity and secondary glaucoma. Selective removal of the suture was carried out on the basis of refractive astigmatism and was guided by topography in both groups during the follow-up period.
Statistical Analysis All the values are presented as mean±standard deviation. Baseline characteristics and outcome variables were compared between two groups by using the student's t-test for paired or unpaired data. A P value of <0.05 was considered to be statistically significant.
RESULTS
There was no statistically significant difference between DALK and ELLK groups in demographic data of patients(Table 1). DALK procedure were performed on 31 eyes,including 22 eyes (70%) using the big-bubble technique. In the remaining 9 eyes air injection did not result in big-bubble formation, so manual stromal dissection was performed to bare DM. Preoperative BSCVA appeared to be worse in the DALK group than in the ELLK group (P=0.005). At all the follow-up visits, BSCVA was better in DALK group (P=0.005; Table 2).Postoperative myopia in the DALK group was significantly lower than in the ELLK group (P=0.006). There were no statistically significant difference among groups in terms of mean postoperative Kmin, Kmax, cylindiric, topographic astigmatism and central corneal thickness (CCT) at last followup visit. After surgery, average endothelial cell density was 2430 cells/mm2 in DALK versus 2398 cells/mm2 in ELLK group, showing no statistically significant difference (P>0.05).The only statistically significant difference was spherical values among groups (Table 3). At last visit, the percentage of the eyes with a BSCVA≥20/40 was 72% in DALK and 26% in ELLK group (P=0.001).
The intraoperative and postoperative complications of the two groups are listed in Tables 4 and 5. Microperforation occurred in 7 out of 31 eyes in DALK group and DALK surgery was finished with manual dissection technique. Double chambers appeared after surgery in 3 eyes and air, sulfur hexafluoride(SF6) and perfluoropropane (C3F8) were injected into anterior chamber and resolved without complication. Graft-host
Table 1 Demographic data of patients in DALK and ELLK groups
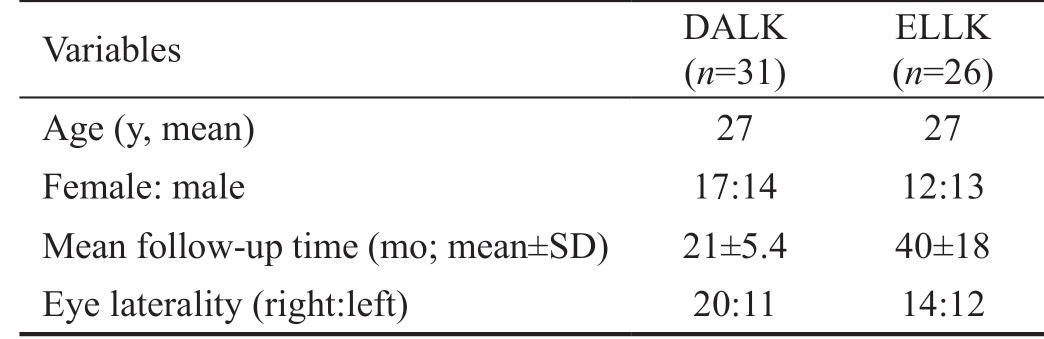
DALK: Deep anterior lamellar keratoplasty; ELLK: Excimer laser assisted anterior lamellar keratoplasty; SD: Standart deviation.
Variables DALK(n=31)ELLK(n=26)Age (y, mean) 27 27 Female: male 17:14 12:13 Mean follow-up time (mo; mean±SD) 21±5.4 40±18 Eye laterality (right:left) 20:11 14:12
Table 2 Preoperative and postoperative snellen visual acuity undergoing DALK and ELLK mean±SD
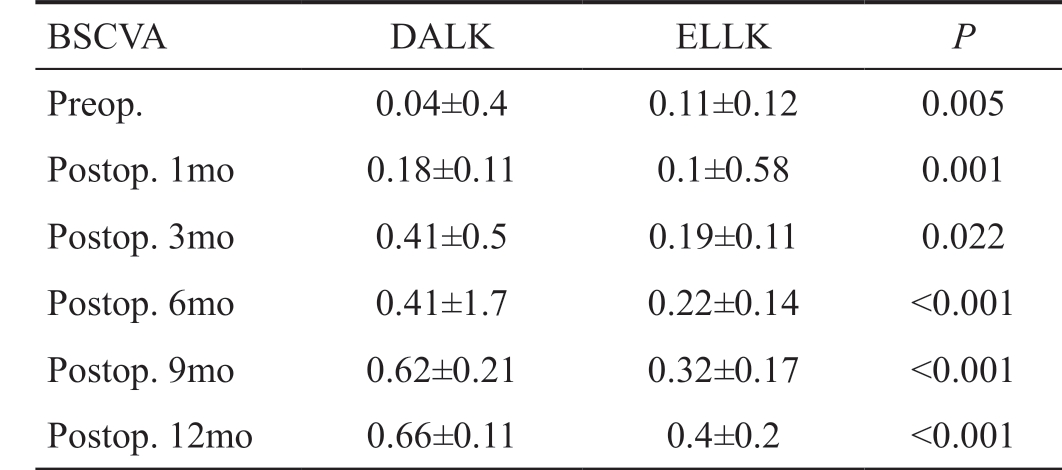
BSCVA DALK ELLK P Preop. 0.04±0.4 0.11±0.12 0.005 Postop. 1mo 0.18±0.11 0.1±0.58 0.001 Postop. 3mo 0.41±0.5 0.19±0.11 0.022 Postop. 6mo 0.41±1.7 0.22±0.14 <0.001 Postop. 9mo 0.62±0.21 0.32±0.17 <0.001 Postop. 12mo 0.66±0.11 0.4±0.2 <0.001
BSCVA: Best spectacle corrected visual acuity; DALK: Deep anterior lamellar keratoplasty; ELLK: Excimer laser assisted anterior lamellar keratoplasty; SD: Standart deviation; Preop.: Preoperative; Postop.:Postoperative.
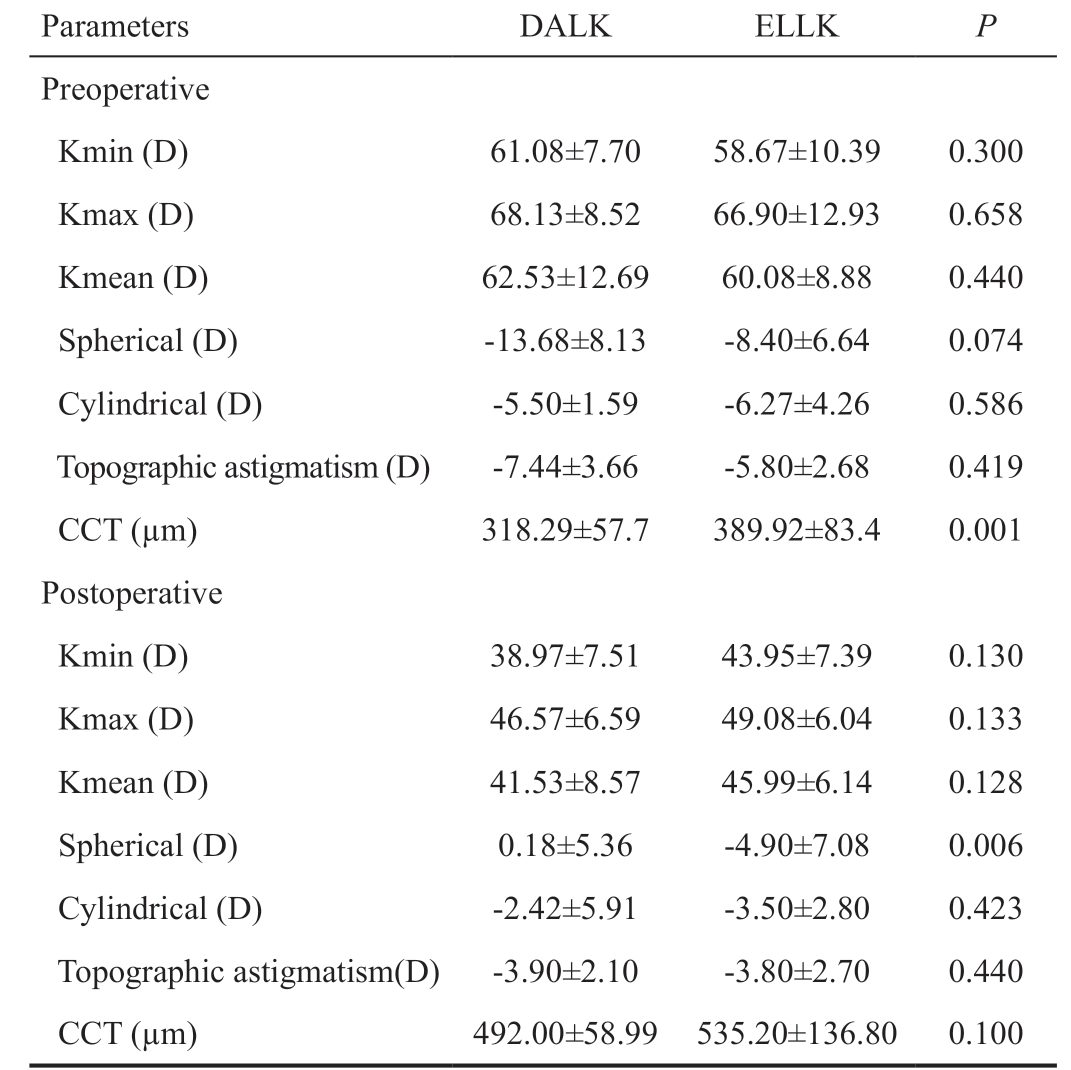
DALK: Deep anterior lamellar keratoplasty; ELLK: Excimer laser assisted anterior lamellar keratoplasty; SD: Standart deviation; CCT:Central corneal thickness; Min: Minimum; Max: Maximum; K:Keratometry; D: Diopters.
Parameters DALK ELLK P Preoperative Kmin (D) 61.08±7.70 58.67±10.39 0.300 Kmax (D) 68.13±8.52 66.90±12.93 0.658 Kmean (D) 62.53±12.69 60.08±8.88 0.440 Spherical (D) -13.68±8.13 -8.40±6.64 0.074 Cylindrical (D) -5.50±1.59 -6.27±4.26 0.586 Topographic astigmatism (D) -7.44±3.66 -5.80±2.68 0.419 CCT (µm) 318.29±57.7 389.92±83.4 0.001 Postoperative Kmin (D) 38.97±7.51 43.95±7.39 0.130 Kmax (D) 46.57±6.59 49.08±6.04 0.133 Kmean (D) 41.53±8.57 45.99±6.14 0.128 Spherical (D) 0.18±5.36 -4.90±7.08 0.006 Cylindrical (D) -2.42±5.91 -3.50±2.80 0.423 Topographic astigmatism(D) -3.90±2.10 -3.80±2.70 0.440 CCT (µm) 492.00±58.99 535.20±136.80 0.100
junction dehiscence occurred in three eyes of the DALK group,due to spontaneous wound dehiscence after suture removal at 3mo after surgery. DM wrinkles occurred in 17 out of 31 eyes but visual acuity was not affected in the DALK group.
In the follow up period, 3 eyes were treated steroid induced glaucoma. All of them returned to normal IOP following adjustment of the topical steroid together with topical antiglaucoma medication. There was no need for glaucoma surgery.
In ELLK group, microbial keratitis was seen in 1 eye, which were treated appropriate topical therapy. Pupillary block with a fixed dilated pupil occured after anterior chamber air injection in 1 eye. Interface haze and DM wrinkling had been in 4 eyes and in 6 eyes, respectively (Table 5). No graft rejection occurred in ELLK and in DALK group.
DISCUSSION
Lamellar surgery requires significant technical and surgical challenges. In spite of many advantages lamellar surgery,interface irregularity often results in suboptimal visual outcomes. Therefore, new techniques in lamellar keratoplasty have been developed and modified in the past years. Various lamellar keratoplasty techniques have been submitted like air injection[4], viscodissection[4], hydrodissection[5],microkeratome[6] and excimer laser[7]. However, none of these methods were as successful as air injection method. Anwar and Teichmann[2] then described the big-bubble technique toconsistently achieve separation of the DM from stroma after air filled injection. DALK is the low rate of endothelial rejection,endothelial loss and graft failure[8].
Table 4 Intraoperative and postoperative complications after DALK
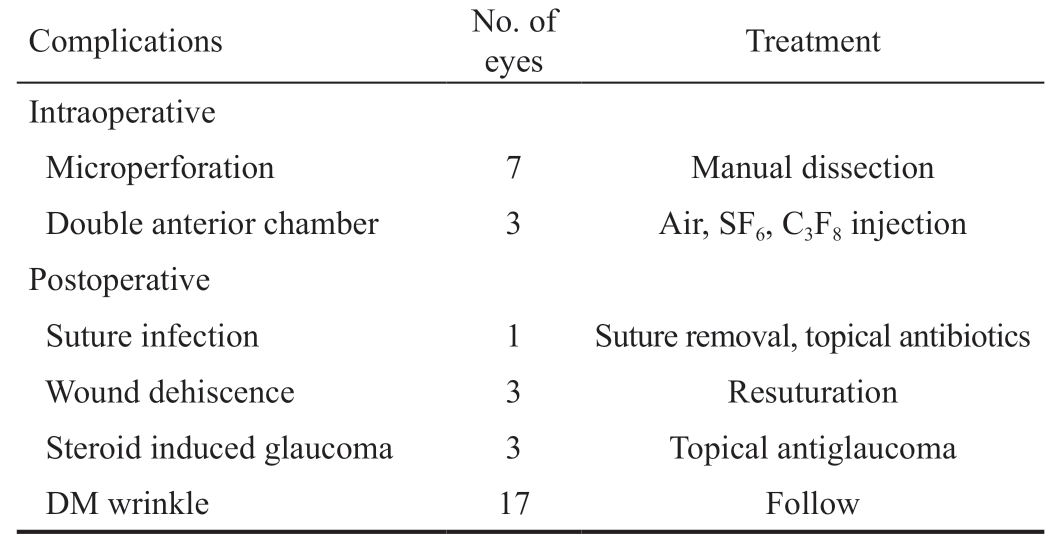
DALK: Deep anterior lamellar keratoplasty; SF6: Sulfurhexafluorise;C3F8 : Perfluoropropane; DM: Descemet's membrane.
Complications No. of eyes Treatment Intraoperative Microperforation 7 Manual dissection Double anterior chamber 3 Air, SF6, C3F8 injection Postoperative Suture infection 1 Suture removal, topical antibiotics Wound dehiscence 3 Resuturation Steroid induced glaucoma 3 Topical antiglaucoma DM wrinkle 17 Follow
Table 5 Intraoperative and postoperative complications after ELLK
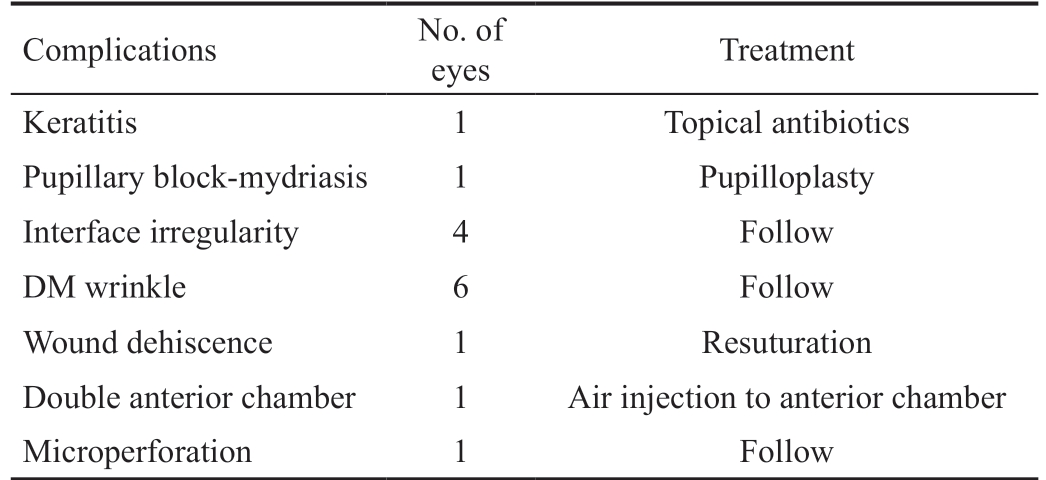
ELLK: Excimer laser assisted anterior lamellar keratoplasty; DM:Descemet's membrane.
Complications No. of eyes Treatment Keratitis 1 Topical antibiotics Pupillary block-mydriasis 1 Pupilloplasty Interface irregularity 4 Follow DM wrinkle 6 Follow Wound dehiscence 1 Resuturation Double anterior chamber 1 Air injection to anterior chamber Microperforation 1 Follow
In this study, visual and refractive outcomes were evaluated.At last examination, BSCVA was improved from its preoperative value all patients in both groups. In DALK group,postoperative BSVCA was 0.66±0.11 and 20/40 or better in 72% at the last visit. Similar results were also reported after DALK surgery in keratoconus patients, ranging between 76%and 91%[9-11]. Postoperative visual acuities were not different between manual (9 eyes) and big-bubble (22 eyes) groups in DALK (P=0.23). This is in line with previous papers[12-13].There were no interface irregularity in manual dissection group.In ELLK group, postoperative BSCVA was 0.4±0.2. Buratto et al[14] reported mean BSCVA of 20/30 in 20 keratoconus patients with ELLK. Spadea et al[3] reported mean BSCVA 0.11±0.11 logMAR in 41 keratoconus patients. Low visual acuity was observed in our study compared with the literature. We thought this was due to the reason of the interface irregularities. Also,topography guided excimer laser combined with PRK was used to improve postoperative residual refractive error in 9 patients (36%).
At the all postoperative period, BSCVA was lower in ELLK group (P<0.001). As reasons for the lack of visual acuity in ELLK group was failure to provide a smooth interface and presence of interface stromal irregularities. The all patients were performed in DALK had clear cornea at the last followup visit and no lack of vision due to interface irregularity.
The host-donor interface irregularities can limit visual acuity after ALK. In this study, irregularity at the interface limited vision in 4 eyes after ELLK. Big-bubble technique were performed these patients after 6y later from the first surgery.Visual acuity increased from 0.1 to 0.7 after new surgery. So,manual or big-bubble DALK can be performed after ELLK,safely.
ELLK is a technique which can be repeated and requires a short surgical time and risk of complications is low.Through these properties it has led to its availability of such young patients with keratoconus. ELLK does not disclaim the necessity for DALK or PKP subsequently and ELLK is technically easier than DALK. DM wrinkle is another complication that may affect visual acuity. According to the studies in the literature, high K values is a risk factor for DM wrinkle[15-16]. Totally, 17 patients (54.8%) were found to be DM wrinkles in DALK group. There was no difference between groups with and without DM wrinkles because the membrane was transparent and thin in DALK. ELLK group of 6 patients(23%) were followed DM wrinkles. The presence of stromal residue on DM and formation of wrinkles on thicker layers had negative effect on visual acuity.
DM micro and macroperforation is the most frequent complication of DALK and the most important complication that limited surgery. In order to avoid possible double anterior chamber and persistent corneal edema, PKP is preferred or the operation is resumed with manual dissection technique.DM microperforation occurred in 7 patients (23%) and the procedure was performed with manual stromal dissection technique. DM perforation rates are reported ranging between 0 and 50% in keratoconus patients after big-bubble DALK[17-20].DM thickness increases with age and DM is more strong in the elderly compared with young people[21-22].
Double anterior chamber is another significant complication after DALK and ELLK. DM microperforations during surgery, aqueous humor accumulation on the interface after surgery can cause double anterior chamber. In order to limit the microperforations or avoid double anterior chamber,air, 18% SF6 or 14% C3F8 can be injected into the anterior chamber. A large air bubble may need to be kept in the anterior chamber until there is a significant improvement (1-2wk).It can be difficult to maintain gas tamponade in tears that inferior or larger. Air bubble in the anterior chamber may cause a reduction in the number of endothelial cell count. In addition, the air may lead to pupillary block which causes air block glaucoma. Urrets-Zavalia was described as a syndrome which consisting of a group of complications such as air block glaucoma, pupillary dilation, synechiae[22]. In this study,double anterior chamber developed in 3 eyes in DALK group,postoperatively. Air, SF6 and C3F8 were injected into anterior chamber and resolved without complication. Urrets-Zavalia Syndrome was developed in 1 eye in ELLK group and 1y after the first surgery were treated with pupilloplasty.
Theorically, lamellar surgery decreases immune rejection risk because endothelium is the main objective for rejection. All types of graft rejection can develop after DALK surgery[23-24].In the current study, none of rejection or graft failure was observed in the two groups.
The major advantage of DALK is to protect the endothelial layer from possible stress. A report by Reinhart et al[25] showed that endothelial cell loss after the surgery was similar the gradual endothelial cell loss of a normal cornea. In our study,we found significant endothelial cell loss only during the first 6mo after surgery. At the last follow-up, there is no statistically significant difference in endothelial cell density between groups. These results are similar to other studies[5,12] .
In both groups, the mean CCT was significantly greater than preoperatively. CCT values showed no changes between groups postoperatively. The similarity the CCT values between 2 groups suggests that in our study, stromal dissection was conducted at very close to the DM.Since keratoconus patients are young, it is important to perform their treatment with less invasive methods and choose a step-by-step therapeutic plan. DALK is a difficult procedure and if micro-macroperforations occur, it may be necessary to convert to PKP. Moreover, the lack of standardization and reproducibility is a disadvantage of procedures involving DALK. Excimer laser may be an option to remove recipient corneal stroma for this problem. Therefore, ELLK could be a valuable alternative to PKP or DALK for keratoconus patients.Compared with DALK, complication rate is lower, the surgical technique is simpler, fast and ELLK requires less experience.Further, not achieved satisfactory visual acuity after ELLK,DALK can be performed.
ACKNOWLEDGEMENTS
Conflicts of Interest: Ceylanoglu KS, None; Aydin B, None;Ozmen MC, None.
1 Parker JS, van Dijk K, Melles GR. Treatment options for advanced keratoconus: a review. Surv Ophthalmol 2015;60(5):459-480.
2 Anwar M, Teichmann KD. Big-bubble technique to bare Descemet's membrane in anterior lamellar keratoplasty. J Cataract Refract Surg 2002;28(3):398-403.
3 Spadea L, Giammaria D, Fiasca A, Verrecchia V. Excimer laser-assisted lamellar keratoplasty for the surgical treatment of keratoconus. J Cataract Refract Surg 2009;35(1):105-112.
4 Alio JL, Shah S, Barraquer C, Bilgihan K, Anwar M, Melles GR. New techniques in lamellar keratoplasty. Curr Opin Ophthalmol 2002;13(4):224-229.
5 Sugita J, Kondo J. Deep lamellar keratoplasty with complete removal of pathological stroma for vision improvement. Br J Ophthalmol 1997;81(3):184-188.
6 Azar DT, Jain S, Sambursky R. A new surgical technique of microkeratome-assisted deep lamellar keratoplasty with a hinged flap.Arch Ophthalmol 2000;118(8):1112-1115.
7 Bilgihan K, Ozdek SC, Sari A, Hasanreisoğlu B. Excimer laser-assisted anterior lamellar keratoplasty for keratoconus, corneal problems after laser in situ keratomileusis, and corneal stromal opacities. J Cataract Refract Surg 2006;32(8):1264-1269
8 Chen Y, Hu DN, Xia Y, Yang L, Xue C, Huang Z. Comparison of femtosecond laser-assisted deep anterior lamellar keratoplasty and penetrating keratoplasty for keratoconus. BMC Ophthalmology 2015;15:144.
9 Romano V, Iovieno A, Parente G, Soldani AM, Fontana L. Long-term clinical outcomes of deep anterior lamellar keratoplasty in patients with keratoconus. Am J Ophthalmol 2015;159(3):505-511.
10 Söğütlü Sari E, Kubaloğlu A, Ünal M, Piñero Llorens D, Koytak A,Ofluoglu AN, Özertürk Y. Penetrating keratoplasty versus deep anterior lamellar keratoplasty: comparison of optical and visual quality outcomes.Br J Ophthalmol 2012;96(8):1063-1067.
11 Yüksel B, Kandemir B, Uzunel UD, Çelik O, Ceylan S, Küsbeci T.Comparison of visual and topographic outcomes of deep-anterior lamellar keratoplasty and penetrating keratoplasty in keratoconus. Int J Ophthalmol 2017;10(3):385-390.
12 Knutsson KA, Rama P, Paganoni G. Modified big-bubble technique compared to manual dissection deep anterior lamellar keratoplasty in the treatment of keratoconus. Acta Ophthalmol 2015;93(5):431-438.
13 Bhatt UK, Fares U, Rahman I, Said DG, Maharajan SV, Dua HS.Outcomes of deep anterior lamellar keratoplasty following successful and failed ‘big bubble'. Br J Ophthalmol 2012;96(4):564-569.
14 Buratto L, Belloni S, Valeri R. Excimer laser lamellar keratoplasty of augmented thickness for keratoconus. J Refract Surg 1998;14(5):517-525.15 Khakshoor H, Eslampoor A, Rad SS, Vejdani A. Modified deep anterior lamellar keratoplasty for the treatment of advanced keratoconus with steep corneal curvature to help in eliminating the wrinkles in the Descemet's membrane. Indian J Ophthalmol 2014;62(4):392-395.
16 Mohamed SR, Manna A, Amissah-Arthur K, McDonnell PJ. Nonresolving Descemet folds 2 years following deep anterior lamellar keratoplasty: the impact on visual outcome. Cont Lens Anterior Eye 2009;32(6):300-302.
17 Zhang YM, Wu SQ, Yao YF. Long-term comparison of full-bed deep anterior lamellar keratoplasty and penetrating keratoplasty in treating keratoconus. J Zhejiang Univ Sci B 2013;14(5):438-450.
18 Cheng YY, Visser N, Schouten JS, Wijdh RJ, Pels E, van Cleynenbreugel H, Eggink CA, Zaal MJ, Rijneveld WJ, Nuijts RM.Endothelial cell loss and visual outcome of deep anterior lamellar keratoplasty versus penetrating keratoplasty: a randomized multicenter clinical trial. Ophthalmology 2011;118(2):302-309.
19 Keane M, Coster D, Ziaei M, Williams K. Deep anterior lamellar keratoplasty versus penetrating keratoplasty for treating keratoconus.
Cochrane Database Syst Rev 2014(7):CD009700.
20 Leccisotti A. Descemet's membrane perforation during deep anterior lamellar keratoplasty: prognosis. J Cataract Refract Surg 2007;33(5):825-829.21 Shousha MA, Perez VL, Wang JH, Ide T, Jiao SL, Chen Q, Chang V,Buchser N, Dubovy SR, Feuer W, Yoo SH. Use of ultra-high-resolution optical coherence tomography to detect in vivo characteristics of Descemet's membrane in Fuchs' dystrophy. Ophthalmology 2010;117(6): 1220-1227.
22 Maurino V, Allan BD, Stevens JD, Tuft SJ. Fixed dilated pupil (Urrets-Zavalia syndrome) after air/gas injection after deep lamellar keratoplasty for keratoconus. Am J Ophthalmol 2002;133(2):266-268.
23 Fontana L, Parente G, Tassinari G. Clinical outcomes after deep anterior lamellar keratoplasty using the big-bubble technique in patients with keratoconus. Am J Ophthalmol 2007;143(1):117-124.
24 Al-Torbak AA, Al-Motowa S, Al-Assiri A, Al-Kharashi S, Al-Shahwan S, Al-Mezaine H, Teichmann K. Deep anterior lamellar keratoplasty for keratoconus. Cornea 2006;25(4):408-412.
25 Reinhart WJ, Musch DC, Jacobs DS, Lee WB, Kaufman SC, Shtein RM. Deep anterior lamellar keratoplasty as an alternative to penetrating keratoplasty a report by the american academy of ophthalmology.Ophthalmology 2011;118(1):209-218.