INTRODUCTION
he influence of micro-incisi on phacoemulsification on biomechanical parameters of the cornea has been
T discussed in several studies, emphasising the role of viscous dampening [corneal hysteresis (CH) parameter], viscoelasticity and stiffness [corneal resistance factor (CRF)][1-10]. It has been proved that corneal biomechanics plays an important role in healing process of the cornea and allows accurate measurement of intraocular pressure (IOP)[11-15]. What's more, according to the 10th Consensus Meeting: Diagnosis of Primary Open Angle Glaucoma Seattle, USA, Goldman applanation tonometry(GAT) is no longer recommended as “the gold standard” in routine IOP measurement[13,15-17]. Currently it is believed that corneal biomechanical properties have greater impact on IOP measurements than corneal thickness or curvature [11,13,15]. In clinical practice, there are two devices measuring corneal biomechanical properties (CH, CRF) and corneal corrected IOP e.g. the Ocular Response Analyzer (ORA; Reichert Technologies, USA) as a dynamic bidirectional applanation device, and the Corvis ST (Oculus Optikgeräte Germany),as a dynamic Scheimpflug analyser device[9-10]. In our study biomechanical properties of the cornea (CH and CRF) and IOP[Goldmann correlated IOP (IOPg), corneal compensated IOP(IOPcc)] and waveform score (WS) were measured with ORA.Recently studies showed that CH remains relatively stable after micro-incision cataract surgery; however, there are various factors (e.g. refractive error, history of refractive surgery,corneal ectatic disorders) that may influence CH, CRF and thus precise estimation of IOP[1-7]. It has been shown that CH is decreased in high myopia and increased in high hyperopia while CRF is not affected by spherical refractive error[18]. The specification of corneal biomechanics in eyes with definite corneal astigmatism, prior and following cataract surgery remains unclear. To our knowledge, this problem has not been sufficiently described so far[19-21].Aim of this study was to define the CH, CRF, IOPg and IOPcc prior to and following coaxial micro-incision phacoemulsification in patients with corneal astigmatism.
SUBJECTS AND METHODS
Ethical Approval The prospective clinical study was performed in the Department of Ophthalmology of our hospital. The official approval by the Ethics Committee conformed to the Declaration of Helsinki was obtained. All subjects enrolled in the study signed an informed consent.
Inclusion criteria were: diagnosis and qualification for cataract surgery, corneal astigmatism equal to or less than +2.25 D in order to make the research group coherent. Only patients with “against the rule” astigmatism were enrolled in the study,as it is well known that corneal astigmatism tends to change towards “against the rule“ in adults, regardless if the patient had cataract surgery or not [18-20].
The exclusion criteria were: corneal astigmatism higher than+2.25 D, history of any corneal ectatic conditions, dystrophies or degenerations of the cornea, pseudoexfoliation syndrome,glaucoma and use of anti-glaucoma eye drops for more than one year, blepharitis, dry eye, use of contact lenses within three months before surgery, diabetes or a history of corneal refractive surgery.
All of the measurements were done by same physician, blinded to the astigmatism of the patients. WS was the parameter defining quality of each measurement taken. Only the measurements of relatively good quality (WS>5/10) have been subjected to the statistics. Biometry, including axial length(AXL), keratometry and intraocular lens (IOL) calculation were performed in the eye requiring cataract surgery with use of a Tomey Optical Biometer OA 2000 to measure. The patients enrolled were divided into two groups, based on their astigmatism range. Group 1 consisted of patients with corneal astigmatism lower than +1.0 D (K1-K2<+1.0 D), and group 2 of corneal astigmatism equal or higher than +1.0 D and equal or lower than +2.25 D (+1.0≤K2-K1≤+2.25). IOP values and corneal biomechanical parameters were analysed between the two study groups preoperatively, one week and one month postoperatively. Additionally, the differences in IOP values and corneal biomechanics were analysed separately in groups 1 and 2 preoperatively, one week and one month postoperatively.
The surgical technique was coaxial micro-incision phacoemulsification with implantation of a foldable acrylic hydrophobic AcrySof® IQ Monofocal (Model Number:SN60WF; Optic Type: Biconvex; Optic Diameter: 6.0; Overall Length: 13.0 mm, Aspheric, A-constant 118.7; Refractive Index: 1.55; Light filtration: UV and blue light) IOL. All of the surgeries were done by the same, highly experienced surgeon, under local (4% Alcaine drops) and intracameral(1% preservative-free lidocaine) anaesthesia. The device used to perform phacoemulsification was an INFINITI® Vision System, OZil® Torsional Handpiece. The corneal opening of 2.0 mm was done with use of Straigh Diamond Knife 2 mm,Trapezoidal, t AE-8192. In each patient main clear corneal incision was placed on at 12 o'clock regardless of steep axis of the cornea, while side port on 2 o'clock (same in right and left eyes). Simultaneously, no corneal relaxing incisions were applied intraoperatively.
The compatibility of a normal distribution has been checked for all measurable variables using λ-Kolmogorov test. We used Student's t-test for independent samples as well as t-test for dependent samples to compare two measurements of the same parameter in the same group pre- and postoperatively. The differences between the mean values and the dependencies between attributes have been found as statistically significant,where the error of probability was P<0.05.
RESULTS
Among 97 subjects enrolled in the study, 58 were females and 39 were males, having a mean age of 72.22±9.67y. Group 1 consisted of 51 patients with a mean age of 72.04±8.97y and mean astigmatism value of +0.49± 0.25 D. Group 2 included 46 patients with a mean age of 72.41±10.47y and astigmatism of +1.43±0.43 D. The mean values of parameters measured preoperatively, 1wk and 1mo postoperatively in study groups are shown in Table 1.
Statistical analysis of independent samples revealed no significant differences between study groups, neither preoperatively nor at any point of the postoperative examinations (P>0.05; Table 2).In group 1, CRF (t=2.68, P<0.05), CH (t=2.64, P<0.05)and WS (t=3.51, P<0.05) were significantly lower one week postoperatively, when compared to the preoperative values(Table 3). Similarly, CRF significantly decreased (t=3.61,P<0.05) when measured one month following the surgery.In contrast, neither the values of IOPg nor IOPcc were significantly different when measured one week or one month postoperatively (Table 3).
In group 2 CH (t=5.92, P<0.05), and WS (t=3.96, P<0.05)were significantly lowered one week after cataract surgery(Table 4). Moreover, we observed a significant decrease in IOPg (t=2.24, P<0.05), CRF (t=5.05, P<0.05) and CH(t=2.31, P<0.05) one month after phacoemulsification.
Table 1 Characteristics of parameters measured preoperatively,1wk and 1mo postoperatively in groups 1 and 2 mean±SD (mm Hg)
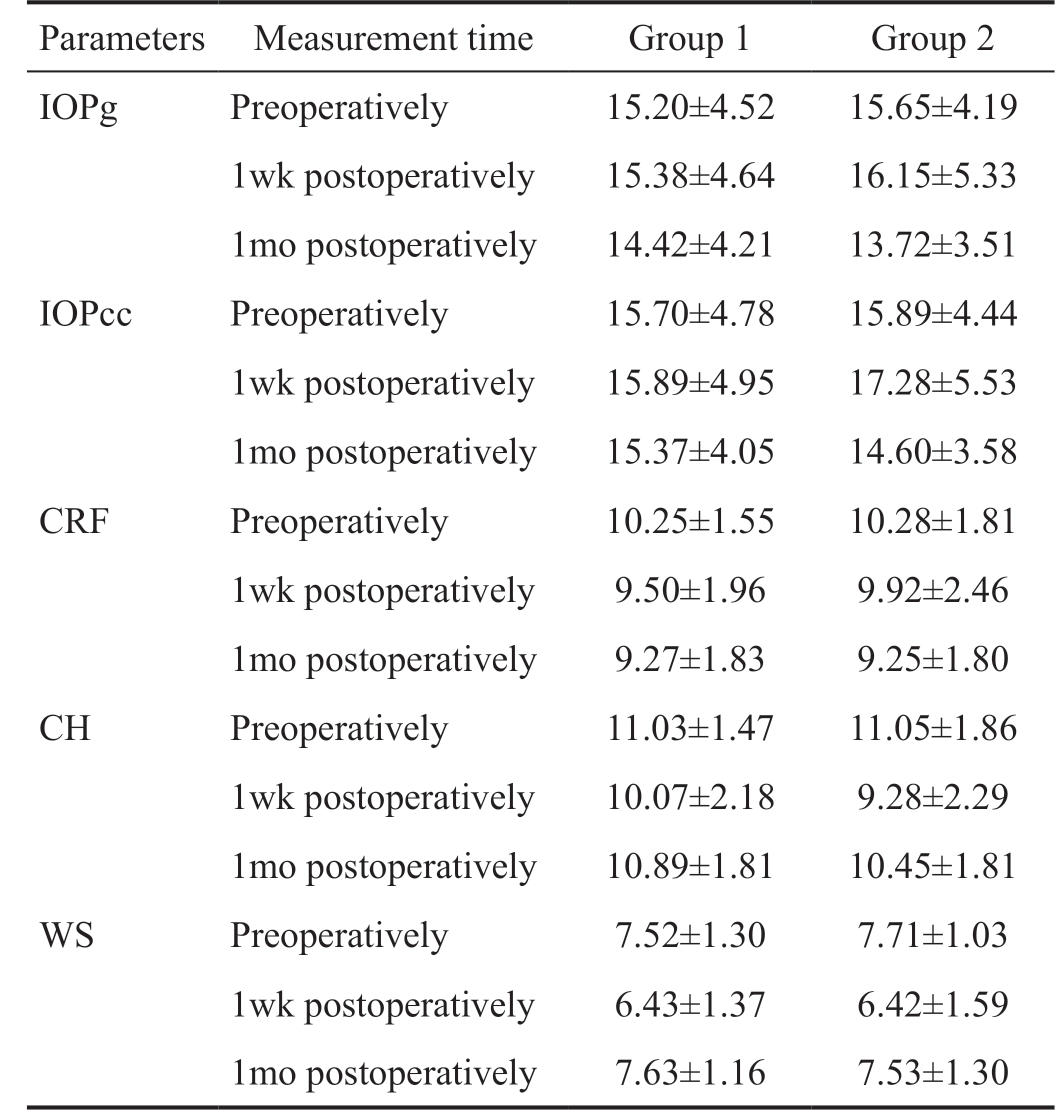
Parameters Measurement time Group 1 Group 2 IOPg Preoperatively 15.20±4.52 15.65±4.19 1wk postoperatively 15.38±4.64 16.15±5.33 1mo postoperatively 14.42±4.21 13.72±3.51 IOPcc Preoperatively 15.70±4.78 15.89±4.44 1wk postoperatively 15.89±4.95 17.28±5.53 1mo postoperatively 15.37±4.05 14.60±3.58 CRF Preoperatively 10.25±1.55 10.28±1.81 1wk postoperatively 9.50±1.96 9.92±2.46 1mo postoperatively 9.27±1.83 9.25±1.80 CH Preoperatively 11.03±1.47 11.05±1.86 1wk postoperatively 10.07±2.18 9.28±2.29 1mo postoperatively 10.89±1.81 10.45±1.81 WS Preoperatively 7.52±1.30 7.71±1.03 1wk postoperatively 6.43±1.37 6.42±1.59 1mo postoperatively 7.63±1.16 7.53±1.30
Group 1: Patients with corneal astigmatism <+1.0 D; Group 2: Patients with corneal astigmatism ≥+1.0 D and ≤+2.25 D;IOPg: Goldmann correlated intraocular pressure; IOPcc: Corneal compensated intraocular pressure; CRF: Corneal resistance factor;CH: Corneal hysteresis; WS: Waveform score. Surgical procedure:Coaxial micro-incision phacoemulsification with implantation of foldable IOL into the posterior capsule.
Table 2 Differences between groups 2 and 1 preoperatively, 1wk and 1mo postoperatively
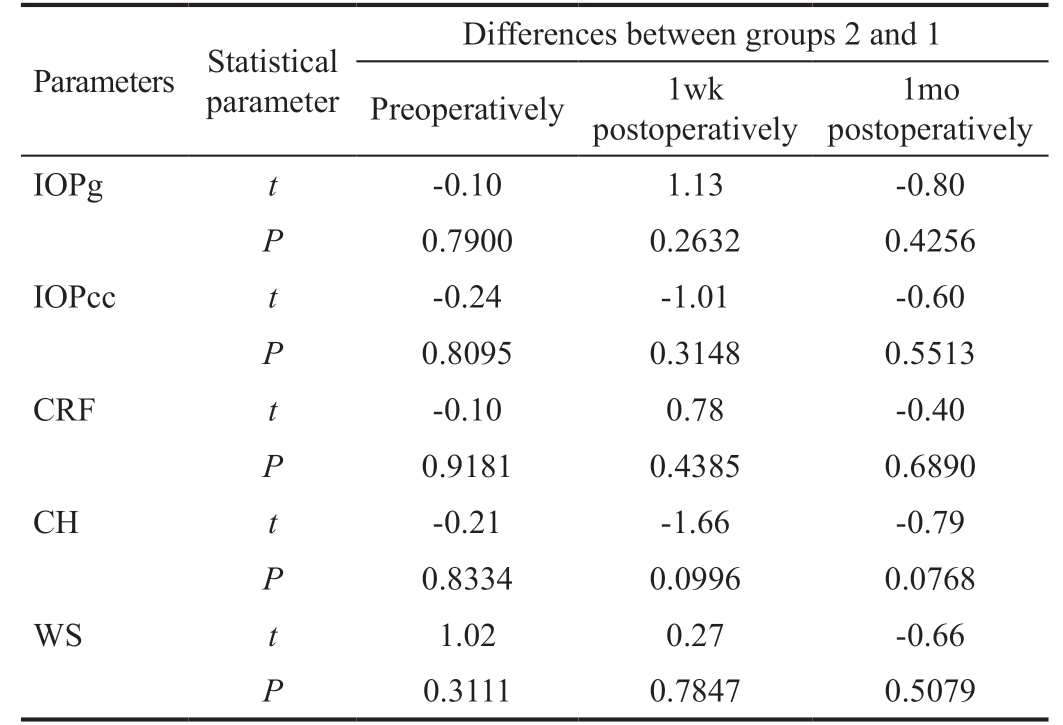
Group 1: Patients with corneal astigmatism <+1.0 D; Group 2:Patients with corneal astigmatism ≥+1.0 D and ≤+2.25 D; t: The calculated difference between groups 2 and 1 represented in units of standard error; P: Error of probability (statistically significant when P<0.05); IOPg: Goldmann correlated intraocular pressure;IOPcc: Corneal compensated intraocular pressure; CRF: Corneal resistance factor; CH: Corneal hysteresis; WS: Waveform score.Surgical procedure: Coaxial micro-incision phacoemulsification with implantation of foldable IOLs into the posterior capsule.
Parameters Statistical parameter Differences between groups 2 and 1 Preoperatively 1wk postoperatively 1mo postoperatively IOPg t -0.10 1.13 -0.80 P 0.7900 0.2632 0.4256 IOPcc t -0.24 -1.01 -0.60 P 0.8095 0.3148 0.5513 CRF t -0.10 0.78 -0.40 P 0.9181 0.4385 0.6890 CH t -0.21 -1.66 -0.79 P 0.8334 0.0996 0.0768 WS t 1.02 0.27 -0.66 P 0.3111 0.7847 0.5079
Table 3 Differences between parameters measured preoperatively vs 1wk and 1mo postoperatively in group 1
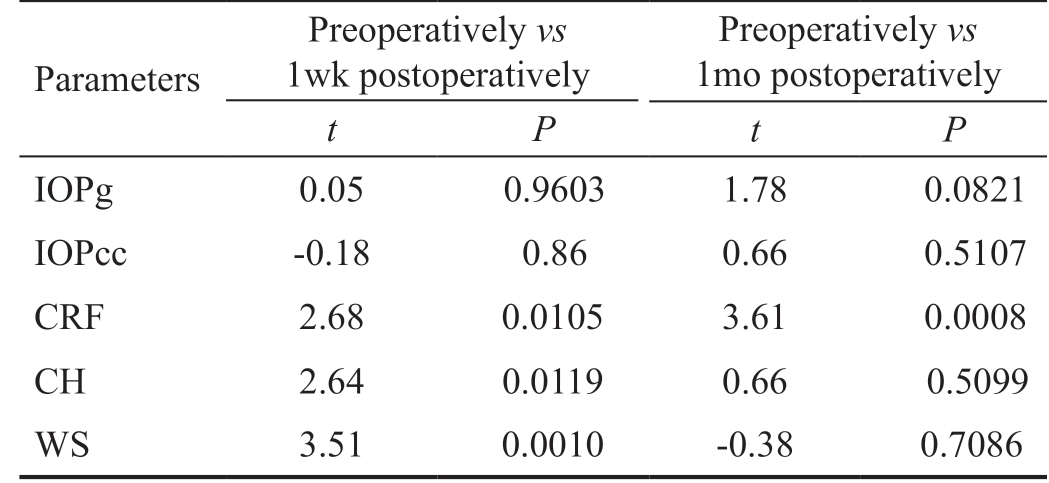
Group 1: Patients with corneal astigmatism <1.0 D; Group 2: Patients with corneal astigmatism >1.0 D and <2.25 D; t: The calculated difference represented in units of standard error; P: Error of probability (statistically significant when P<0.05); IOPg: Goldmann correlated intraocular pressure; IOPcc: Corneal compensated intraocular pressure; CRF: Corneal resistance factor; CH: Corneal hysteresis; WS: Waveform score. Surgical procedure: Coaxial microincision phacoemulsification with implantation of foldable IOLs into the posterior capsule.
Parameters Preoperatively vs 1wk postoperatively Preoperatively vs 1mo postoperatively t P t P IOPg 0.05 0.9603 1.78 0.0821 IOPcc -0.18 0.86 0.66 0.5107 CRF 2.68 0.0105 3.61 0.0008 CH 2.64 0.0119 0.66 0.5099 WS 3.51 0.0010 -0.38 0.7086
Table 4 Differences between parameters measured preoperatively vs 1wk and 1mo postoperatively in group 2
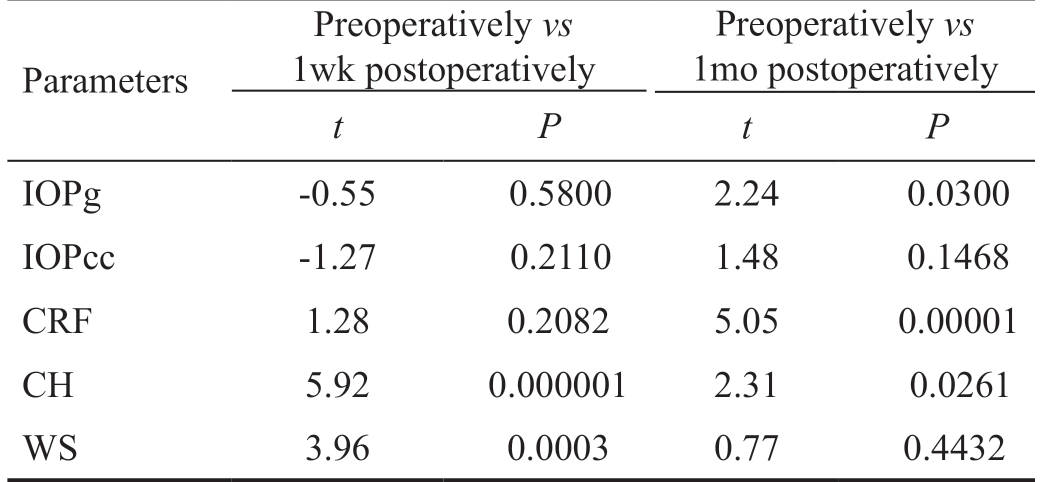
Parameters Preoperatively vs 1wk postoperatively Preoperatively vs 1mo postoperatively t P t P IOPg -0.55 0.5800 2.24 0.0300 IOPcc -1.27 0.2110 1.48 0.1468 CRF 1.28 0.2082 5.05 0.00001 CH 5.92 0.000001 2.31 0.0261 WS 3.96 0.0003 0.77 0.4432
Group 1: Patients with corneal astigmatism <1.0 D; Group 2: Patients with corneal astigmatism >1.0 D and <2.25 D; t: The calculated difference represented in units of standard error; P: Error of probability (statistically significant when P<0.05); IOPg: Goldmann correlated intraocular pressure; IOPcc: Corneal compensated intraocular pressure; CRF: Corneal resistance factor; CH: Corneal hysteresis; WS: Waveform score. Surgical procedure: Coaxial microincision phacoemulsification with implantation of foldable IOLs into the posterior capsule.
IOPcc did not differ when assessed one week and one month postoperatively (P>0.05; Table 4).
There was no statistically significant difference in AXL (t=-0.83,P=0.41) between group 2 and group 1 (Table 5). In each group,mean AXL did not correlate with corneal astigmatism, IOPg,IOPcc, CH, CRF and WS (P>0.05) before and after cataract surgery.
In group 2, corneal astigmatism of +1.0≤K2-K1≤+2.25 D correlated positively with preoperative IOPg (r2=0.14, P<0.05)and IOPcc (r2=0.18, P<0.05). In contrast, in group 1 the significant correlation between corneal astigmatism of K2-K1<+1.0 D and IOPg (r2=0.03, P>0.05) or IOPcc (r2=0.02,P>0.05) was not observed (Table 6).
DISCUSSION
Cataract surgery may be the cause of early postoperative complications affecting the ocular surface as: corneal oedema, loss of corneal endothelial cells and following corneal decompensation, erosion, irritation of conjunctiva and symptoms of dry eye syndrome[22]. These factors may, in turn, affect the parameters of corneal biomechanics, causing significant decrease in CH (group 1, t=2.64, P<0.05; group 2,t=5.72, P<0.05) and CRF (group 1, t=2.68, P<0.05) within the first postoperative week, as presented in our results (Tables 3 and 4). Moreover, in our study CRF remained lowered throughout the first postoperative month in patients with corneal astigmatism of +1.0≤K2-K1≤+2.25 D (group 2). This outcome disagree with the findings of Kamiya et al[4], where CH and CRF were decreased only on the first postoperative day then recovered to preoperative values within one week after cataract surgery.
Due to the early postsurgical complications and healing process of the cornea, the quality of measurement may be significantly decreased. Also in our study there was the significant decrease in WS (group 1, t=3.51, P<0.05; group 2, t=3.96, P<0.05)within the first postsurgical week. WS returned to the preoperative level after the period of 1mo postoperatively in group 1 (t=-0.38, P>0.05) and in group 2 (t=0.77, P>0.05;Tables 3 and 4).
There was no statistically significant difference in AXL between group 2 and group 1 (Table 5). In each study group,mean AXL did not correlate with corneal astigmatism, IOPg,IOPcc, CH, CRF and WS (P>0.05) before and at any point of time after cataract surgery.
Corneal astigmatism of +1.0≤K2-K1≤+2.25 D (group 2)correlated positively with preoperative IOPg (r2=0.14, P<0.05)and IOPcc (r2=0.18, P<0.05). In contrast, the significant correlation between corneal astigmatism of K2-K1<+1.0 D(group 1) and IOPg (r2=0.03, P>0.05) or IOPcc (r2=0.02,P>0.05) was not observed preoperatively. These results suggest that corneal astigmatism may affect IOP values when measured prior to the cataract surgery.
IOPg and IOPcc measured in group 1 (K1-K2<+1.0 D) did not differ from preoperative values and remained relatively constant, when measured at 1wk and 1mo postoperatively(Table 3).
Similarly, in group 2 (+1.0≤K2-K1≤+2.25), there was no significant change in IOPcc following cataract surgery (Table 4).It is well known that IOPcc is less affected by central corneal thickness and corneal properties of the cornea (CH, CRF),thus it remains unchanged following surgical procedures on the anterior segment of the eye[23-25]. In turn, IOPg wassignificantly lower in group 2, when measured one month after phacoemulsification. Conclusively, instability of CH, CRF and IOPg in eyes with corneal astigmatism at the level of +1.0≤K2-K1≤+2.25 (group 2) may lead to underestimation of the real IOP postoperatively. Heinrich et al[7], compared GAT and dynamic contour tonometry (DCT) before and after cataract surgery. The authors reported that GAT IOP in pseudophakic eyes was improperly low when compared with DCT outcomes,and thus should be precisely monitored for development of glaucoma[7]. In our study, IOPg corresponds to GAT IOP,and IOPcc to DCT IOP. Our results agree with the results of Heinrich et al[7], showing that the objective cause of lower postoperative GAT IOP (IOPg) or dynamic contour tonometry(DCT) IOP (IOPcc) should be explored. Based on our results,it is clearly observed that preoperative corneal astigmatism in the range of +1.0 D to +2.25 D may be the reason for lowered IOP measured one month postoperatively. It is therefore necessary, to precisely monitor IOP in these patients and remain suspicious, especially when diagnosing low-tension or normal-tension glaucoma.
Table 5 Differences of AXL between groups 1 and 2 mean±SD

AXL: Axial length; Group 1: Patients with corneal astigmatism <1.0 D;Group 2: Patients with corneal astigmatism >1.0 D and <2.25 D; t:The calculated difference represented in units of standard error; P:Error of probability (statistically significant when P<0.05).
Groups AXL t P 1 23.28±1.07 -0.83 0.4085 2 23.03±1.84
Table 6 Correlations between corneal astigmatism and IOPg,IOPcc, CH, CRH and WS in groups 1 and 2
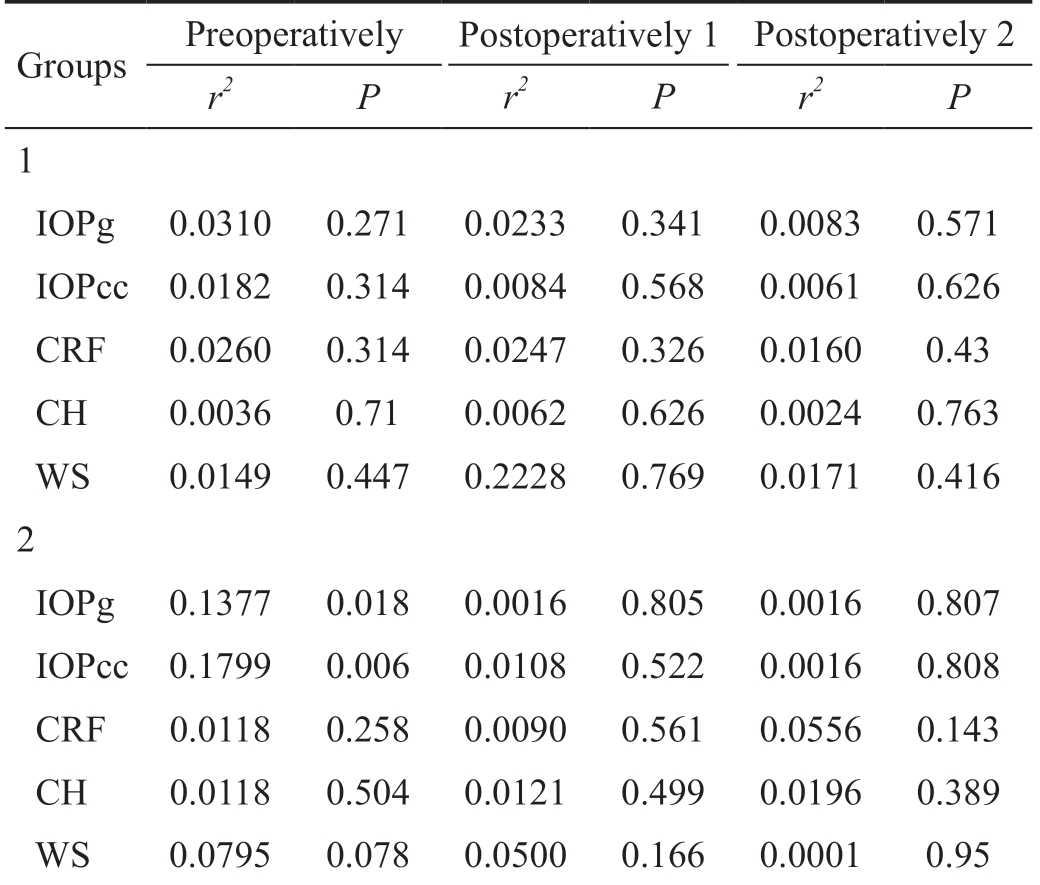
Group 1: Patients with corneal astigmatism <1.0 D; Group 2: Patients with corneal astigmatism >1.0 D and <2.25 D; r2: Correlation coefficient; P: Error of probability (statistically significant when P<0.05); IOPg: Goldmann correlated intraocular pressure; IOPcc:Corneal compensated intraocular pressure; CRF: Corneal resistance factor; CH: Corneal hysteresis; WS: Waveform score. Surgical procedure: Coaxial micro-incision phacoemulsification with implantation of foldable IOLs into the posterior capsule.
Groups Preoperatively Postoperatively 1 Postoperatively 2 r2 P r2 P r2 P 1 IOPg 0.0310 0.271 0.0233 0.341 0.0083 0.571 IOPcc 0.0182 0.314 0.0084 0.568 0.0061 0.626 CRF 0.0260 0.314 0.0247 0.326 0.0160 0.43 CH 0.0036 0.71 0.0062 0.626 0.0024 0.763 WS 0.0149 0.447 0.2228 0.769 0.0171 0.416 2 IOPg 0.1377 0.018 0.0016 0.805 0.0016 0.807 IOPcc 0.1799 0.006 0.0108 0.522 0.0016 0.808 CRF 0.0118 0.258 0.0090 0.561 0.0556 0.143 CH 0.0118 0.504 0.0121 0.499 0.0196 0.389 WS 0.0795 0.078 0.0500 0.166 0.0001 0.95
In conclusion, in short-term follow up of one month postoperatively, we observed significantly reduced CRF, CH and IOPg, in patients with preoperative corneal astigmatism equal or higher than +1.0 D and lower than +2.25 D. Hence,bias of IOPg measurement in patients with preoperative corneal astigmatism equal or higher than +1.0 D and lower than +2.25 D may cause underestimation of the real IOP both before and after cataract surgery. The measurement of IOPcc allows the precise assessment of IOP pre- and postoperatively,independently on corneal astigmatism, CH and CRF values.
ACKNOWLEDGEMENTS
Conflicts of Interest: Pniakowska Z, None; Jurowski P,None.
1 Alió JL, Agdeppa MC, Rodrıguez-Prats JL, Amparo F, Piñero DP.Factors influencing corneal biomechanical changes after micro-incision cataract surgery and standard coaxial phacoemulsification. J Cataract Refract Surg 2010;36:90-897.
2 Kandarakis A, Soumplis V, Karampelas M, Koutroumanos I, Panos C, Kandarakis S, Karagiannis D. Response of corneal hysteresis and central corneal thickness following clear corneal cataract surgery. Acta Ophthalmol 2012;90(6):526-529.
3 Terai N, Raiskup F, Haustein M, Pillunat LE, Spoerl E. Identification of biomechanical properties of the cornea: the ocular response analyzer. Curr Eye Res 2012;37(7):553-562.
4 Kamiya K, Shimizu K, Ohmoto F, Amano R. Time course of corneal biomechanical parameters after phacoemulsification with intraocular lens implantation. Cornea 2010;29(11):1256-1260.
5 Pakravan M, Afroozifar M, Yazdani S. Corneal biomechanical changes following trabeculectomy, phaco-trabeculectomy, ahmed glaucoma valve implantation and phacoemulsification. J Ophthalmic Vis Res 2014;9(1):7-13.6 Denoyer A, Ricaud X, Van Went C, Labbé A, Baudouin C. Influence of corneal biomechanical properties on surgically induced astigmatism in cataract surgery. J Cataract Refract Surg 2013;39(8):1204-1210.
7 Heinrich MA, Eppig T, Langenbucher A, Walter S, Behrens-Baumann W, Viestenz A. Comparison of Goldmann applanation and dynamic contour tonometry before and after cataract surgery. J Cataract Refract Surg 2012;38(4):683-689.
8 Wei YJ, Xu LX, Song H. Application of Corvis ST to evaluate the effect of femtosecond laser-assisted cataract surgery on corneal biomechanics.Exp Ther Med 2017;14(2):1626-1632.
9 Piñero DP, Alcón N. Corneal biomechanics: a review. Clin Exp Optom 2015;98(2):107-116.
10 Koç M, İlhan Ç, Koban Y, Özülken K, Durukan İ, Yılmazbaş P. Effect of corneal biomechanical properties on surgically-induced astigmatism and higher-order aberrations after cataract surgery. Arq Bras Oftalmol 2016;79(6):380-383.
11 Roberts CJ, Liu J. Corneal Biomechanics: From Theory to Practice.The Netherlands: Kugler Publications;2016.
12 Sródka W. Goldmann applanation tonometry-not as good as gold. Acta Bioeng Biomech 2010;12(2):39-47.
13 Jedzierowska M, Koprowski R, Wróbel Z. Overview of the Ocular Biomechanical Properties Measured by the Ocular Response Analyzer and the Corvis ST. Information Technologies in Biomedicine 2014;4:377-386.14 Tanaka M, Wada S, Nakamura M. Computational Biomechanics:Theoretical Background and Biological/Biomedical Problems. Tokyo:Springer;2012.
15 Wilson A, Marshall J, Tyrer JR. The role of light in measuring ocular biomechanics. Eye (Lond) 2016;30(2):234-240.
16 10th Consensus Meeting: Diagnosis of Primary Open Angle Glaucoma Seattle, USA, April 30, 2016 Edited by: R.N. Weinreb, D.F. Garway-Heath, C. Leung, F.A. .Medeiros, J. Liebmann 2016. Many photos and figures. Hardbound. ISBN-10: 90 6299 262 5. ISBN-13: 978 90 6299 262 1 Published by: Kugler Publications. Available at: https://books.google.pl/books?id=MDbTDgAAQBAJ&lpg=PP1&hl=pl&pg=PP1#v=onepage&q&f=false.
17 Deol M, Taylor DA, Radcliffe NM. Corneal hysteresis and its relevance to glaucoma. Curr Opin Ophthalmol 2015;26(2):96-102.
18 İnceoğlu N, Emre S, Ulusoy MO. Investigation of corneal biomechanics at moderate to high refractive errors. Int Ophthalmol 2018;38(3):1061-1067.
19 Trivizki O, Shahar J, Levinger S, Levinger E. Air-pulse corneal applanation signal curve parameters for characterization of astigmatic corneas. Cornea 2014;33(7):721-725.
20 Han X, Guo X, Lee PY, Morgan IG, He M. Six-year changes in refraction and related ocular biometric factors in an adult Chinese population. PLoS One 2017;12(8):e0183364.
21 Hayashi K, Manabe SI, Hirata A, Yoshimura K. Changes in corneal astigmatism during 20 years after cataract surgery. J Cataract Refract Surg 2017;43(5):615-621.
22 McKellar MJ, Elder MJ. The early complications of cataract surgery:is routine review of patients 1 week after cataract extraction necessary?Ophthalmology 2001;108(5):930-935.
23 Touboul D, Roberts C, Kérautret J, Garra C, Maurice-Tison S,Saubusse E, Colin J. Correlations between corneal hysteresis, intraocular pressure, and corneal central pachymetry. J Cataract Refract Surg 2008;34(4):616-622.
24 Osman IM, Helaly HA, Abdalla M, Shousha MA. Corneal biomechanical changes in eyes with small incision lenticule extraction and laser assisted in situ keratomileusis. BMC Ophthalmol 2016;16:123.25 Salman AG. Corneal biomechanical and anterior chamber parameters variations after 1-year of transepithelial corneal collagen cross-linking in eyes of children with keratoconus. Middle East Afr J Ophthalmol 2016;23(1):129-134.