INTRODUCTION
P ersistent fetal vasculature (PFV) results from persistence of the embryonic hyaloid vasculature manifesting variably with ocular abnormalities including cataracts which may require surgical removal[1-3]. PFV is significantly more common and constitute 24% of the patients with congenital cataract in the first 2y of life[4]. Anterior PFV was defined as fibrovascular membrane attached to the posterior capsule or around the lens but not extending beyond the midvitreous space[5]. Anterior PFV was also classified as a special type of unilateral congenital cataract[6], but with its own specific pathological changes compared to other types of congenital cataract: mainly opacification of the posterior lens capsule and usually complicated with other types of anterior segment abnormalities, so congenital cataract with PFV may undergo different way of surgical treatment including way of intraocular lens (IOLs) implantation[7-8], and may have different visual acuity (VA) and anatomical prognosis. Secondary IOL implantation is an effective way for aphakic children with congenital cataract without PFV[9]. However, studies on children with congenital cataract with anterior PFV undergoing secondary IOL implantation have been limited. We evaluated in this study the outcomes including VA, and complications in children with unilateral congenital cataract complicated with anterior PFV undergoing secondary sulcus IOL implantation.
SUBJECTS AND METHODS
Ethical Approval The study was approved by the Institutional Review Board of Beijing Tongren Hospital and was conducted in accordance with the Declaration of Helsinki. The guardians of all the children were fully informed of the purpose and methods of this study and had provided written informed consent.Children with unilateral congenital cataract complicated with anterior PFV who underwent secondary sulcus IOL implantation between January 2015 and September 2016 after lensectomy combined with vitrectomy (peripheral anterior lens capsule were kept intact with central anterior capsulotomy using vitrectomy probe in the primary surgery) at Beijing Tongren Eye Center were retrospectively reviewed.
In this study, congenital cataract complicated with anterior PFV was defined as fibrovascular membrane around the lens or attached to the posterior capsule involving the pupillary zone and also the presence of retrolental vitreous membrane or stalk reaching the optic nerve without retinal traction or detachment.Indications for IOL implantation in our study included: 1)patients older than 2y; 2) confirmation of adequate peripheral capsular support for sulcus IOL implantation; 3) patients with best-corrected visual acuity (BCVA) of logMAR 1.0 or better before IOL implantation; 4) poor compliance with wearing contact lens or spectacles or IOL implantation as requested by parents or by the ophthalmic surgeon because of economic reasons or concern about the possible complications of wearing contact lens; 5) follow-up of at least 12mo after IOLs implantation; 6) exclusion of patients with pre-existing microphthalmia, or corneal opacity, etc.
A tunnel incision of the clear corneal and paracentesis at 10 and 2 o'clock positions were made for acrylic foldable IOL insertion. Viscoelastic was injected in the anterior chamber to lyse possible adhesions between the iris and the peripheral anterior lens capsule, and an IOL was placed in front of the peripheral anterior lens capsule under viscoelastic within the ciliary sulcus. The clear corneal incision was closed using 10-0 non-absorbable monofilament nylon sutures (Figure 1).
The parameters studied were visual outcomes before IOL implantation and at the last follow-up; intraoperative and postoperative complications.
VA records included perception of light, and determination of VA using the Teller card, or Snellen acuity cards depending on the age and cooperation of the child, the age of secondary IOL implantation ranges from 26 to 79mo, patients that could not cooperate with Snellen acuity examination underwent Teller card examination. To achieve standardization and for statistical considerations, documented corrected VA was converted to logMAR values.
Pediatric ophthalmologists and optometrists were consulted for deprivational, refractive, cycloplegic correction and spectacles or contact lens fitting.
The IOL power was calculated with the SRK/T formula. The goal of implanted IOL was set at attaining a lower grade of hyperopia, which was based on the age of the child at the surgery as described by Enyedi et al[10].
Three complications were mainly reviewed and recorded:postoperative increased inflammation, glaucoma, and decentration of the IOL. Increased postoperative inflammation was defined as cells or flare >2+ in the anterior chamber,complicated secondary glaucoma was defined if the patient had intraocular pressure (IOP) >22 mm Hg with increased optic nerve cupping or unexpected myopic refractive shift or increased corneal diameter[11]. If the patient had increased IOP postoperatively less than a week but no associated ocular changes, we defined this as transient IOP rise. Decentration of IOL was defined when the distance of the IOL center from the corneal center was more than 5 mm.
Statistic analysis was performed using SPSS version 17.0(SPSS Inc., Chicago, IL, USA). Data are summarized as mean and standard deviation, and P<0.05 (two tail) was considered statistically significant.
RESULTS
This study included twenty-two children, of which 10 were boys and 12 were girls, the mean age was 41.05±15.41mo(range, 26 to 79mo; median, 35mo), and with a mean interval of 3.05±16.73mo (range, 12 to 70mo; median, 28mo) between the primary surgery of lensectomy combined with vitrectomy and the secondary sulcus IOL implantation. The mean followup duration was 16.55±5.86mo (range, 12 to 71mo; median,16mo; Table 1).
Pupilloplasty in 2 eyes and synechiolysis in 6 eyes were performed at the same time because of preoperative nondilating pupil and adhesion between the iris and the peripheral lens capsule. After thorough explanation with the parents about the benefits and drawbacks of secondary sulcus IOL implantation,ascertainment of the adequate peripheral capsular support, the operating surgeon advised secondary sulcus IOL implantation in 14 of 22 (63.6%) patients. Other indications included parental demand (3/22, 13.6%), contact lens intolerance or uncooperation (2/22, 9.1%), and spectacle noncompliance(3/22, 13.6%).
Two IOL models were used in patients included: SA60 AT(AcrySof, Alcon, Fort Worth, TX, USA); Hoya IOL (Hoya-PS AF-1 Series, Model PC-60AD, Hoya, Japan).Mean BCVA improved from 1.37±0.84 logMAR preoperatively to 0.74±0.57 logMAR postoperatively at final visit (P<0.001;Figure 2). Only 3 (13.64%) eyes attained a BCVA of 0.3 logMAR;12 (54.55%) eyes had BCVA of 0.7 logMAR or better, but worse than 0.3 logMAR; 5 (22.73%) eyes had a BCVA of 1.0 logMAR or better, but worse than 0.7 logMAR; and 2(9.10%) eyes had a BCVA worse than 1.0 logMAR at the last visit.
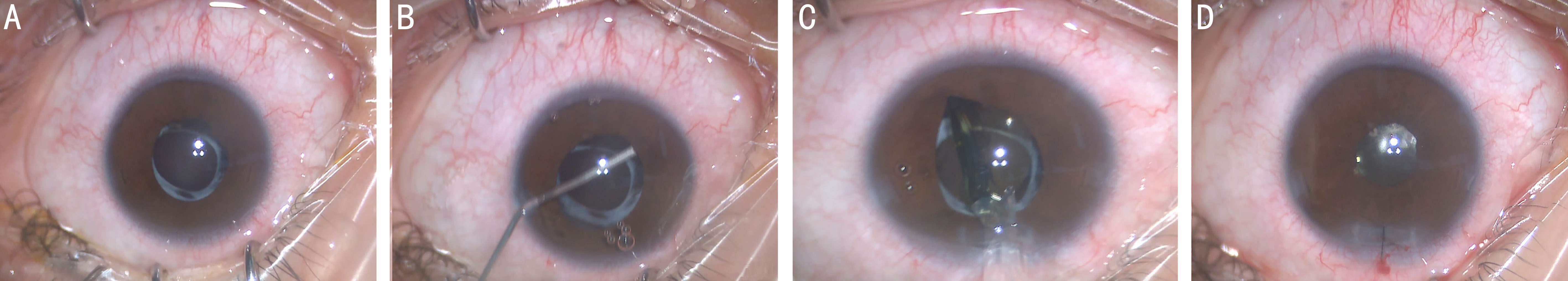
Figure 1 Images taken from surgical video in a boy (case 10) A: Opacified peripheral anterior capsule with clear optical media of the pupillary zone preoperatively; B: Synechiolysis of adhesions between the iris and the peripheral anterior lens capsule using viscoelastic; C: IOL was placed in front of the peripheral anterior lens capsule under viscoelastic; D: Adjustment of ciliary sulcus implanted IOL position and suturing of the clear corneal tunnel incision.
Table 1 Summary of 22 children with anterior PFV who underwent secondary sulcus-implanted IOL
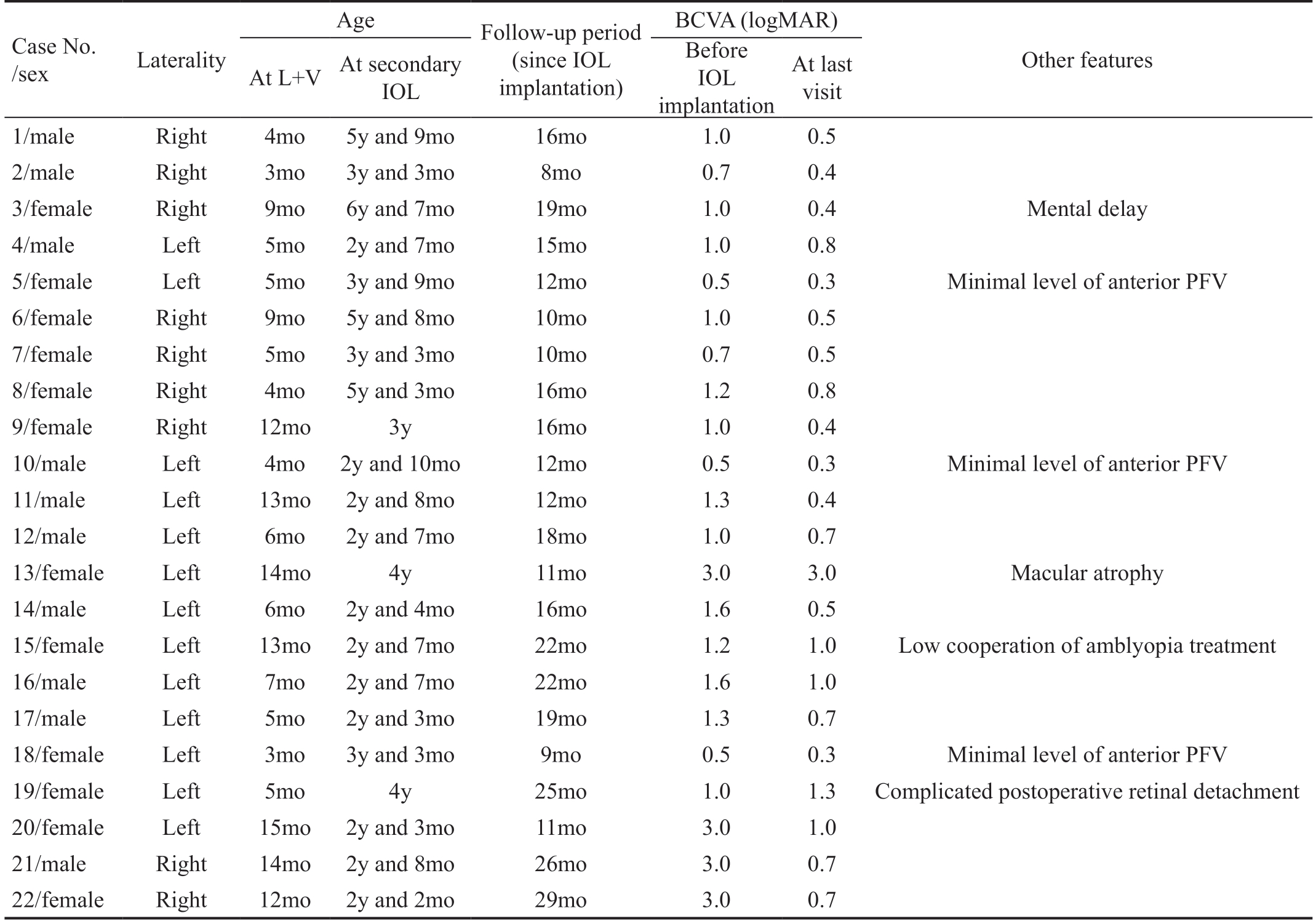
PFV: Persistent fetal vasculature; L+V: Lensectomy +vitrectomy.
Case No./sex Laterality Age Follow-up period(since IOL implantation)BCVA (logMAR)Other features At L+V At secondary IOL Before IOL implantation At last visit 1/male Right 4mo 5y and 9mo 16mo 1.0 0.5 2/male Right 3mo 3y and 3mo 8mo 0.7 0.4 3/female Right 9mo 6y and 7mo 19mo 1.0 0.4 Mental delay 4/male Left 5mo 2y and 7mo 15mo 1.0 0.8 5/female Left 5mo 3y and 9mo 12mo 0.5 0.3 Minimal level of anterior PFV 6/female Right 9mo 5y and 8mo 10mo 1.0 0.5 7/female Right 5mo 3y and 3mo 10mo 0.7 0.5 8/female Right 4mo 5y and 3mo 16mo 1.2 0.8 9/female Right 12mo 3y 16mo 1.0 0.4 10/male Left 4mo 2y and 10mo 12mo 0.5 0.3 Minimal level of anterior PFV 11/male Left 13mo 2y and 8mo 12mo 1.3 0.4 12/male Left 6mo 2y and 7mo 18mo 1.0 0.7 13/female Left 14mo 4y 11mo 3.0 3.0 Macular atrophy 14/male Left 6mo 2y and 4mo 16mo 1.6 0.5 15/female Left 13mo 2y and 7mo 22mo 1.2 1.0 Low cooperation of amblyopia treatment 16/male Left 7mo 2y and 7mo 22mo 1.6 1.0 17/male Left 5mo 2y and 3mo 19mo 1.3 0.7 18/female Left 3mo 3y and 3mo 9mo 0.5 0.3 Minimal level of anterior PFV 19/female Left 5mo 4y 25mo 1.0 1.3 Complicated postoperative retinal detachment 20/female Left 15mo 2y and 3mo 11mo 3.0 1.0 21/male Right 14mo 2y and 8mo 26mo 3.0 0.7 22/female Right 12mo 2y and 2mo 29mo 3.0 0.7

Figure 2 Box-and-whisker plot comparing the mean logMAR BCVA before IOL implantation and logMAR BCVA at last visit in children with unilateral anterior PFV underwent secondary sulcus IOL implantation (P<0.001).
Table 2 Summary of postoperative complications after secondary IOL implantation in patients with anterior PFV
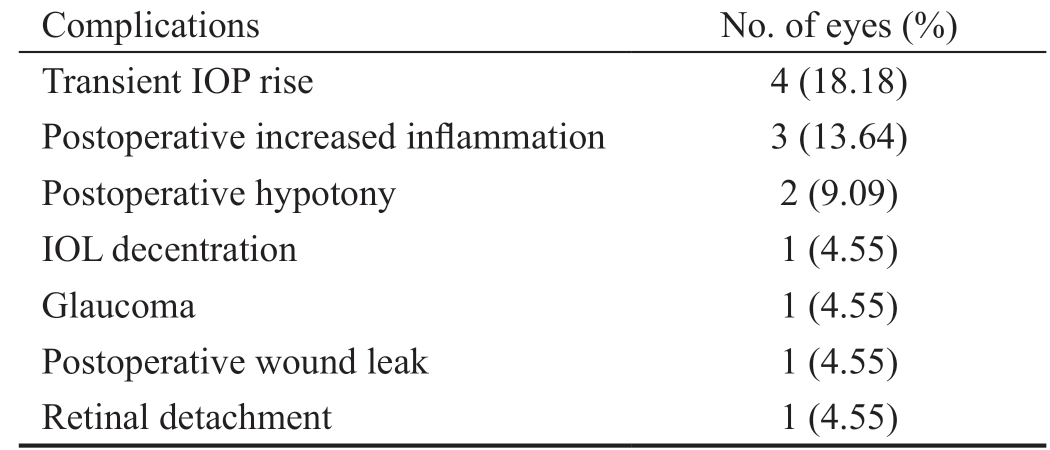
PFV: Persistent fetal vasculature.
Complications No. of eyes (%)Transient IOP rise 4 (18.18)Postoperative increased inflammation 3 (13.64)Postoperative hypotony 2 (9.09)IOL decentration 1 (4.55)Glaucoma 1 (4.55)Postoperative wound leak 1 (4.55)Retinal detachment 1 (4.55)
Transient IOP rise (4 eyes; 18.18%), postoperative increased inflammation (3 eyes; 13.64%) and postoperative hypotony(2 eyes; 9.09%) were common postoperative complications(Table 2).
DISCUSSION
There has been no consensus on the optimal age, method and intraocular location of the IOLs implantation in pediatric monocular congenital cataract especially cataract that complicated with PFV. Patients with congenital cataract complicated with anterior PFV are always complicated with other developmental anomaly of the anterior segment which results in the dilemma and the difficulty of primary IOL implantation. Posterior capsule opacification of these patients also necessitate the posterior capsulectomy or capsulotomy during the primary surgery, which results in the difficulty of IOL implantation in the capsular bag. We retrospectively studied the short-term results of 22 eyes of 22 pediatric patients with monocular congenital cataract complicated with anterior PFV underwent secondary sulcus IOL implantation in our hospital.
For secondary IOL implantation, the mean age in this study was 41.05mo, which was lower than that of Tadros et al's study (63.7mo)[12]. This may attribute to the fact that most children of this age (36-42mo) have the chance to go to the kindergartens in China and wearing contact lenses or thick aphakic spectacles may give the children a psychological burden since they become more active and more social.
Secondary IOL implantation in those children was according to the surgeon's advice in 63.6% of our patients, which was higher than that of the study conducted by Biglan et al[13].This difference may attribute to the treating ophthalmologist's advice regarding contact lens or spectacles noncompliance as a result of economic constraints or improperly monitoring of contact lens wearing.
Capsular bag is the ideal location for IOL implantation and it maintains better IOL centration and sequestrates the IOL from irritating the highly reactive ciliary body or iris. IOL was placed in the sulcus in our study with a posterior support of peripheral anterior capsule. This was attributed to the necessity of posterior capsulectomy during the primary surgery, and reservation of proper size of peripheral anterior capsule, so as to facilitate secondary implantation of IOL in future.
Although the ciliary sulcus has been the common site for secondary IOL implantation for many years[14-16], and previous reports have shown that IOL placed in the ciliary sulcus works well in pediatric patients[17], sulcus IOL implantation theoretically increases the risk of transient postoperative IOP rise or even glaucoma and increased postoperative inflammation as a result of iris chaffing or pigment dispersion,also the increased possibility of IOL decentration compared to in-the-bag implantation.
Postoperative IOP elevation was noted in 4 eyes (18.18%)in our study, of which 2 eyes were caused by postoperative inflammation and the other 2 eyes were caused by retained viscoelastics or steroid response. This was slightly lower than that reported by Crnic et al (22%)[16]. IOP were all controlled by topical antiglaucoma medication.
Postoperative increased inflammation was defied as cells or flare >2+ in the anterior chamber and 3 eyes (13.64%) were seen in our series which was slightly higher than that reported by Awad et al[17], but it was significantly lower than the 91.7% reported by Nihalani and Vanderveen[18]. This is likely because all the patients in our study had undergone posterior capsulectomy and anterior vitrectomy through the pars plana or pars plicata incisions during primary cataract surgery, which is known to reduce postoperative anterior chamber inflammation[19-20].
Decentration of the IOL was noted in 1 eye (4.55%) in the present study because of inadequate synechiolysis relieving of the adhesion between the iris and the peripheral lens capsule.This patient needed repositioning and the IOL was stable at the last follow-up.
One patient complicated with retinal detachment 12mo after IOL implantation because of accidental ocular trauma by a flying badminton, and further surgery was needed to reattach the retina.
Crnic et al[16] reported that 85% attained a final BCVA of 20/80 or better, and Awad et al[17] reported that 78% of eyes in their pediatric aphakic case series with secondary sulcus IOL implantation had 20/80 or better vision, in our study, 68.29%of the patients achieved a final BCVA of 0.7 logMAR or better,which was slightly lower than that of the reported studies.This may be resulted from the fact that our patients were all complicated with PFV and that children with unilateral congenital cataract usually had significant amblyopia before surgery, which led to poorer visual rehabilitations. The periodically and timely pre- and postoperative anti-amblyopia therapy may play an important role in the comparatively,reasonably good postoperative visual outcomes in our series.This retrospective study has many limitations including its relatively short time of follow-up and absence of comparison with primary or in the bag implantation of IOL, and also the potential bias that those 22 patients had unparalleled ages receiving lensectomy+vitrectomy, which will inevitably influence their further visual prognosis after secondary IOL surgery. But it has its advantage of being the largest series of pediatric patients with unilateral congenital cataract complicated with anterior PFV undergoing secondary sulcus IOL implantation, and the operations were all done by the same surgeon within a relatively short-period of time duration between January 2015 and September 2016.
Based on this retrospective studies, we demonstrate that properly preservation of the anterior lens capsule during the primary surgery facilitated secondary sulcus IOL implantation in pediatric patients with unilateral congenital cataract complicated with anterior PFV, and with favorable postoperative visual outcomes and compatible percentage of complications. However, with the long life span of these patients, further studies with longer-term follow up and more paralleled cases is necessary to explore the visual prognosis especially the related complications in the future.
ACKNOWLEDGEMENTS
Foundation: Supported by Beijing Tongren Hospital, Capital Medical University (No.TRZDYXZY201703).
Conflicts of Interest: Liu JH, None; Li SF, None; Deng GD,None; Jiao YH, None; Lu H, None.
1 Reese AB. Persistent hyperplastic primary vitreous. Am J Ophthalmol 1955;40(3):317-331.
2 Goldberg MF. Persistent fetal vasculature (PFV): an integrated interpretation of signs and symptoms associated with persistent hyperplastic primary vitreous (PHPV). LIV Edward Jackson Memorial Lecture. Am J Ophthalmol 1997;124(5):587-626.
3 Peyman GA, Sanders DR, Nagpal KC. Management of persistent hyperplastic primary vitreous by pars plana vitrectomy. Br J Ophthalmol 1976;60(11):756-758.
4 Solebo AL, Russell-Eggitt I, Cumberland P, Rahi JS. Congenital cataract associated with persistent fetal vasculature: findings from IoLunder2. Eye(Lond) 2016;30(9):1204-1209.
5 Anteby I, Cohen E, Karshai I, BenEzra D. Unilateral persistent hyperplastic primary vitreous: course and outcome. J AAPOS 2002;6(2):92-99.
6 Vasavada AR, Vasavada SA, Bobrova N, Praveen MR, Shah SK,Vasavada VA, Pardo A JV, Raj SM, Trivedi RH. Outcomes of pediatric cataract surgery in anterior persistent fetal vasculature. J Cataract Refract Surg 2012;38(5):849-857.
7 Matsuo T. Intraocular lens implantation in unilateral congenital cataract with minimal levels of persistent fetal vasculature in the first 18 months of life. Springerplus 2014;3:361.
8 Liu JH, Lu H, Li SF, Jiao YH, Lin N, Liu NP. Outcomes of small gauge pars plicata vitrectomy for patients with persistent fetal vasculature: a report of 105 cases. Int J Ophthalmol 2017;10(12):1851-1856.
9 Wilson ME Jr, Hafez GA, Trivedi RH. Secondary in-the-bag intraocular lens implantation in children who have been aphakic since early infancy. J AAPOS 2011;15(2):162-166.
10 Enyedi LB, Peterseim MW, Freedman SF, Buckley EG. Refractive changes after pediatric intraocular lens implantation. Am J Ophthalmol 1998;126(6):772-781.
11 Shenoy BH, Mittal V, Gupta A, Sachdeva V, Kekunnaya R.Complications and visual outcomes after secondary intraocular lens implantation in children. Am J Ophthalmol 2015;159(4):720-726.
12 Tadros D, Trivedi RH, Wilson ME, Davidson JD. Ocular axial growth in pseudophakic eyes of patients operated for monocular infantile cataract:a comparison of operated and fellow eyes measured at surgery and 5 or more years later. J AAPOS 2016;20(3):210-213.
13 Biglan AW, Cheng KP, Davis JS, Gerontis CC. Secondary intraocular lens implantation after cataract surgery in children. Am J Ophthalmol 1997;123(2):224-234.
14 Zhao YE, Gong XH, Zhu XN, Li HM, Tu MJ, Coursey TG, Pflugfelder SC, Gu F, Chen D. Long-term outcomes of ciliary sulcus versus capsular bag fixation of intraocular lenses in children: An ultrasound biomicroscopy study. PLoS One 2017;12(3):e0172979.
15 Wood KS, Tadros D, Trivedi RH, Wilson ME. Secondary intraocular lens implantation following infantile cataract surgery: intraoperative indications, postoperative outcomes. Eye (Lond) 2016;30(9):1182-1186.16 Crnic T, Weakley DR Jr, Stager D Jr, Felius J. Use of AcrySof acrylic foldable intraocular lens for secondary implantation in children. J AAPOS 2004;8(2):151-155.
17 Awad AH, Mullaney PB, Al-Hamad A, Wheeler D, Al-Mesfer S,Zwaan J. Secondary posterior chamber intraocular lens implantation in children. J AAPOS 1998;2(5):269-274.
18 Nihalani BR, Vanderveen DK. Secondary intraocular lens implantation after pediatric aphakia. J AAPOS 2011;15(5):435-440.
19 Hosal BM, Biglan AW. Risk factors for secondary membrane formation after removal of pediatric cataract. J Cataract Refract Surg 2002;28(2):302-309.
20 Plager DA, Lipsky SN, Snyder SK, Sprunger DT, Ellis FD, Sondhi N.Capsular management and refractive error in pediatric intraocular lenses.Ophthalmology 1997;104(4):600-607.