INTRODUCTION
The treatment of inferior retinal detachment (RD) with proliferative vitreoretinopathy (PVR) in the lower retinal periphery represents a challenge for vitreoretinal surgeons.PVR is the most relevant complication associated with RD surgery and the main cause of poor anatomical and functional outcomes[1-4]. Pars plana vitrectomy (PPV) and silicone oil tamponade associated with scleral buckling are considered the treatment of choice of advanced PVR. Lighter-than-water tamponades allow the support of the superior retinal periphery and the posterior pole in the upright position. Nevertheless the surface of the lower retinal periphery is not efficiently covered by the silicon oil tamponade, hence allowing a mixture of aqueous humor and growth factors (“PVR soup”) to concentrate here. The “PVR soup” moves to the pre-macular area, enhancing the risk of formation of pre-macular epiretinal membranes, cystoid macular edema and recurrence of inferior RD[2,5-7]. Havier-than-water intraocular tamponades have been developed to resolve this problem, thanks to their many advantages over conventional tamponades. Indeed a heavy silicone oil (HSO) can efficiently tamponade breaks and areas of retinotomy in the lower retinal periphery in the upright position. It displaces the “PVR soup” away from the lower retina and the posterior pole, leading to a quicker and durable reattachment of the macula. Re-detachments are likely to occur mainly in the superior periphery where they can be easily treated with gas tamponade[1].
Densiron® 68 (Fluoron Co, Neu-Ulm, Germany) is a solution of perfluorohexyloctane (F6H8) and 5000 cSt silicone oil[4],characterized by an increased viscosity of F6H8 (from 2.5 to 1387 mPa) and a resulting reduction of the tendency to disperse[8-9]. Several studies, including the “Heavy Silicone Oil Study” (HSO Study), evaluated the efficacy and safety of Densiron 68, mainly on patients with complex RD[10-16].
The main purpose of our study was the anatomic reattachment of the retina following Densiron 68 removal and to evaluate functional outcomes, the rate of recurrences, the presence of inflammatory complications and intraocular pressure alterations.
SUBJECTS AND METHODS
Ethical Approval This was a consecutive, retrospective,nonrandomized case review. The study was performed in accordance with the current version of the Declaration of Helsinki (52nd WMA General Assembly, Edinburgh, Scotland,October, 2000) and written informed consent was obtained from all patients prior to participation in the study. Institutional Review Board/Ethics Committee approval was obtained.
We reviewed the records of 49 eyes of 49 patients affected by complex inferior RD who underwent PPV at Careggi University Hospital, Florence, Italy, between November 2014 and February 2017 with a follow-up of at least 6mo. All the patients had undergone only one vitreoretinal procedure before.The surgical procedures were performed by 4 experienced surgeons (Rizzo S, Caporossi T, Barca F, Giansanti F). Twentyfive or 23-gauge PPV were selected and no encircling buckling was combined. In eyes tamponed with standard silicone oil (SSO) in previous surgery the oil was then removed; in patients who underwent scleral buckling in previous surgery,the buckling was not removed. Peripheral vitreous remnants were checked and shaving vitrectomy was extended when needed. Vital dye (Dual Blue, DORC, The Neederlands) was injected into the vitreous chamber on the retinal contraction area to evidence epiretinal PVR. Perfluorodecalin (F Decalin,Fluoron, Germany) was injected in order to flatten the retina up to the periphery to stabilize detached retinal movement during PVR peeling. If the retina contraction did not relax sufficiently after the peeling, a retinectomy was performed. In all the cases a 360° endolaser was performed. Every case was tamponed with Densiron® 68 (Fluoron Co, Neu-Ulm, Germany) HSO. A 23-gauge PPV was selected to remove Densiron 68. After silicone oil extraction dyeing of the epiretinal membrane remnants was performed and eventually laser treatment was applied over any new retinal breaks. Finally, an endotamponade (gas, SSO or HSO) was chosen depending on the retinal status.
The main outcome measures were the mean change in best corrected visual acuity (BCVA; logMAR, Snellen ratio), the anatomic reattachment of the retina following Densiron 68 removal, the rate of recurrences, the mean time of Densiron 68 intraocular tamponade, the presence of inflammatory complications and intraocular pressure alterations. The data also included the state of the lens and the kind of surgery performed. Statistical analyses were performed by means of Stata 12.1 software (StataCorp, College Station, TX, USA).The results were expressed as the mean±standard deviation of the mean (standard error, SE). Paired samples t-tests were used to compare preoperative and postoperative logMAR visual acuities. A P value of 0.05 or less was considered statistically significant.
RESULTS
Forty-nine eyes of 49 patients (M:F=38:11) affected by pathologic complex retinal re-detachment were included. The characteristics of all patients are presented in Table 1.
The mean age of patients was 58.9y (±8.7); 17 patients previously underwent PPV with gas endotamponade or scleral buckling and 32 patients were tamponed with SSO at first surgery. Forty-three eyes were pseudophakic, 6 cases had been made aphakic during previous surgery and in 4/6 cases an intraocular lens (IOL) was implanted during the first surgery. In 26 cases we performed 25-G vitrectomy and in the remaining 23 cases a 23-G PPV was selected. In 2 cases a penetrating keratoplasty was combined to solve corneal opacization which can occur during SSO persistence. We did not perform vitrectomy and scleral buckling together in any case. In all cases we found the presence of PVR (grade C1-3-D),in 3 cases there was a macular hole and in 1 case there was a choroidal detachment. Eleven cases (22.4%) were traumatic RD; 8 cases (16.3%) were high myopic eyes (over 7 diopters);3 cases (6.1%) were already being treated for glaucoma.
The mean BCVA before surgery with Densiron 68 was 1.9 logMAR (20/2000; SE:0.064). The mean BCVA after Densiron 68 removal was 0.95 logMAR (20/200;SE:0.068). The mean follow-up was 7.6mo (±1.5). Rate of retinal reattachment after first surgery was 61.2% (30 eyes).In 19 cases (38.8%) we had recurrences with Densiron 68: in 26.3% (5 cases) the recurrence involved the inferior retina.In patients who underwent PPV with gas endotamponade or scleral buckling (17 patients) there were 11 recurrences of RD(64.7%). In patients with SSO at previous surgery (32 patients),8 eyes (25%) had recurrences with Densiron 68 (4 cases in the superior retina). The Chi-square statistic test showed a statistically significant difference between the two groups(P<0.05). All re-detachment cases underwent vitrectomy with gas tamponade in 2 cases and SSO tamponade in 16 cases. In one eye HSO was used again to solve complicated inferior RD with wide inferior retinectomy. Final retinal reattachment rate was 81.6% (40 eyes; Table 2).
After a mean time of 3.5mo Densiron 68 was removed,according to the clinical retinal status. In 13 cases (26.5%) we had inflammatory complications: emulsion and inflammation in the anterior chamber. In 17 (34.7%) cases we found ocular hypertension with Densiron permanency that needed medical treatment; after Densiron 68 removal, ocular pressure returned to a normal value in 4 cases (23.5%), the remaining 13 cases continued with the medical treatment. No eyes needed incisional glaucoma surgery. Two cases of corneal opacification and 1 case of phthisis occurred. In 6 cases we had anterior chamber inflammation and ocular hypertension at
the same time. In 1 case we registered a central vein occlusion during the silicone tamponade.
Table 1 Pre-operative demographic data and findings of 49 eyes of 49 patients enrolled

PPV: Pars plana vitrectomy; SSO: Standard silicon oil; PVR: Proliferative vitreoretinopathy.
ID Age (y) Gender Eye Comorbidity Previous surgery PVR BCVA 1 53 M L High myopia Scleral buckling Yes 20/20000 2 54 F L Post-traumatic PPV+SSO Yes 20/20000 3 25 F R Post-traumatic PPV+SSO Yes 20/80 4 60 M R / PPV+SSO Yes 20/80 5 78 F R / PPV+SSO Yes 20/250 6 85 M R / PPV+SSO Yes 20/20000 7 54 F L / PPV+SSO Yes 20/20000 8 70 M R / Scleral buckling Yes 20/250 9 72 F L High myopia PPV+SSO Yes 20/100 10 52 M R / PPV+SSO Yes 20/20000 11 49 M L / PPV+SSO Yes 20/20000 12 42 M R High myopia PPV+SSO Yes 20/80 13 75 M L / PPV+SSO Yes 20/200 14 69 M R / Scleral buckling Yes 20/20000 15 37 M R / PPV+SSO Yes 20/20000 16 43 M L / PPV+SSO Yes 20/250 17 86 F R Post-traumatic PPV+gas Yes 20/20000 18 49 M L Post-traumatic PPV+SSO Yes 20/20000 19 82 M R / PPV+gas Yes 20/20000 20 80 M R / PPV+SSO Yes 20/20000 21 29 M L / PPV+gas Yes 20/20000 22 73 M R / PPV+SSO Yes 20/400 23 58 M R / PPV+SSO Yes 20/20000 24 69 M L Post-traumatic PPV+SSO Yes 20/20000 25 52 M R / PPV+SSO Yes 20/200 26 30 M R Post-traumatic PPV+SSO Yes 20/2000 27 19 M R / PPV+SSO Yes 20/20000 28 66 M R / Scleral buckling Yes 20/200 29 50 F R / PPV+gas Yes 20/32 30 80 M L Post-traumatic PPV+gas Yes 20/100 31 24 F L Post-traumatic Scleral buckling Yes 20/20000 32 71 M R / Scleral buckling Yes 20/400 33 52 M R / PPV+SSO Yes 20/100 34 53 M R / PPV+SSO Yes 20/200 35 38 F L Post-traumatic PPV+SSO Yes 20/100 36 89 M R High myopia PPV+SSO Yes 20/20000 37 45 M L / PPV+gas Yes 20/400 38 64 M R / PPV+gas Yes 20/200 39 54 M L / PPV+gas Yes 20/20000 40 76 M L / PPV+SSO Yes 20/250 41 67 M R Post-traumatic PPV+SSO Yes 20/20000 42 57 F R High myopia PPV+SSO Yes 20/20000 43 81 M L / PPV+SSO Yes 20/20000 44 57 M L Post-traumatic PPV+SSO Yes 20/80 45 60 M R / PPV+gas Yes 20/20000 46 75 F R / PPV+SSO Yes 20/80 47 70 M R / PPV+SSO Yes 20/200 48 61 M R / Scleral buckling Yes 20/250 49 53 M L / Scleral buckling Yes 20/80
Table 2 Anatomic and functional outcomes
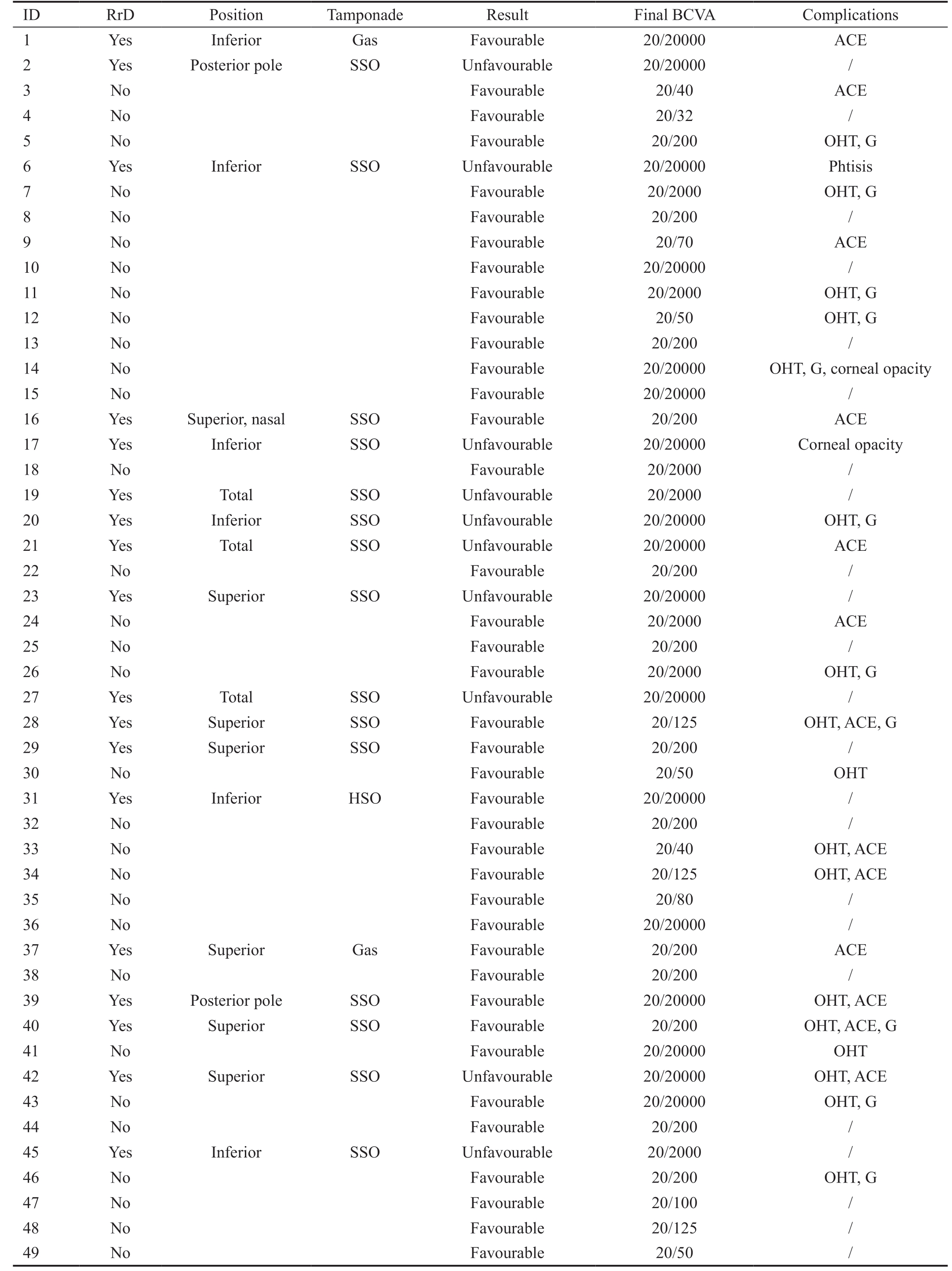
RrD: Retinal re-detachment after Densiron 68 removal; SSO: Standard silicon oil; HSO: Heavy silicon oil; ACE: Anterior chamber emulsification; OHT: Ocular hypertension with densiron; G: Glaucoma after PDMS removal.
ID RrD Position Tamponade Result Final BCVA Complications 1 Yes Inferior Gas Favourable 20/20000 ACE 2 Yes Posterior pole SSO Unfavourable 20/20000 /3 No Favourable 20/40 ACE 4 No Favourable 20/32 /5 No Favourable 20/200 OHT, G 6 Yes Inferior SSO Unfavourable 20/20000 Phtisis 7 No Favourable 20/2000 OHT, G 8 No Favourable 20/200 /9 No Favourable 20/70 ACE 10 No Favourable 20/20000 /11 No Favourable 20/2000 OHT, G 12 No Favourable 20/50 OHT, G 13 No Favourable 20/200 /14 No Favourable 20/20000 OHT, G, corneal opacity 15 No Favourable 20/20000 /16 Yes Superior, nasal SSO Favourable 20/200 ACE 17 Yes Inferior SSO Unfavourable 20/20000 Corneal opacity 18 No Favourable 20/2000 /19 Yes Total SSO Unfavourable 20/2000 /20 Yes Inferior SSO Unfavourable 20/20000 OHT, G 21 Yes Total SSO Unfavourable 20/20000 ACE 22 No Favourable 20/200 /23 Yes Superior SSO Unfavourable 20/20000 /24 No Favourable 20/2000 ACE 25 No Favourable 20/200 /26 No Favourable 20/2000 OHT, G 27 Yes Total SSO Unfavourable 20/20000 /28 Yes Superior SSO Favourable 20/125 OHT, ACE, G 29 Yes Superior SSO Favourable 20/200 /30 No Favourable 20/50 OHT 31 Yes Inferior HSO Favourable 20/20000 /32 No Favourable 20/200 /33 No Favourable 20/40 OHT, ACE 34 No Favourable 20/125 OHT, ACE 35 No Favourable 20/80 /36 No Favourable 20/20000 /37 Yes Superior Gas Favourable 20/200 ACE 38 No Favourable 20/200 /39 Yes Posterior pole SSO Favourable 20/20000 OHT, ACE 40 Yes Superior SSO Favourable 20/200 OHT, ACE, G 41 No Favourable 20/20000 OHT 42 Yes Superior SSO Unfavourable 20/20000 OHT, ACE 43 No Favourable 20/20000 OHT, G 44 No Favourable 20/200 /45 Yes Inferior SSO Unfavourable 20/2000 /46 No Favourable 20/200 OHT, G 47 No Favourable 20/100 /48 No Favourable 20/125 /49 No Favourable 20/50 /
DISCUSSION
Treating a complex RD is a very interesting and difficult challenge. However in severe PVR, especially in patients with previous multiple vitreous surgery and persistent RD of the inferior quadrants, the outcome can be discouraging even with silicone oil. Silicone oil limits, but does not exclude, the diffusion of proliferative cells and inflammatory mediators through the vitreous cavity. If the silicon does not completely fill the eye, it may lead to an incomplete tamponade in the inferior retina, exposed breaks and an accumulation of fluid containing proliferative cells. Therefore, in patients with complex inferior RD a tamponade with heavier-thanwater density could be useful[17]. In our series we had retinal attachment after the first surgery in 61.2% of the patients and recurrences in 38.7%; 32 patients had SSO at first surgery.Densiron removal was performed after an average of 3.5mo(±0.8). Most of our recurrences were in the superior retina, in agreement with the “HSO versus SSO study” by Joussen et al[16]. In patients with gas or scleral buckling at the first surgery(17 patients), we had 11 recurrences (64.7%). In patients with SSO at the first surgery (32 patients), 8 had recurrences with Densiron 68 (25% of 32 patients). Wong et al[18] showed good anatomical and functional results: in his case series no patients developed macula-off detachments once Densiron 68 was used,even though a percentage of patients underwent re-operations involving gas or silicone oil injection; re-attachment in a single operation using Densiron 68 occurred in 81% (34 of 42) of patients, and after additional surgical interventions it became 93% (39 of 42 patients); silicone oil remained in situ in 4 of the 42 patients; re-attachment without any tamponade occurred in 86% (36 of 42) of patients[18]. In Auriol et al[10] case series,total anatomic success at the last follow-up visit was achieved in 25 of the 27 patients (92.5%) who had inferior complex RD treated with Densiron 68. In his series Sandner et al[19]treated 12 patients with complex inferior RD with Densiron 68: he achieved retinal attachment in all eyes at the end of the first surgery. However both when Densiron 68 was in situ and during follow-up after removal, only in four of the 12 patients(30%) the retinal condition was stable; 8 eyes developed redetachment. Nevertheless, after re-intervention in 9 out of the 12 patients (75%) a re-attachment was achieved; in 10 of the 12 patients (83.3%) the macula had re-attached (in 7 without endotamponade) at the 1-year follow up. We also evaluated the functional result: final mean visual acuity was 0.95 logMAR.Wong et al[18] registered visual acuity improvement from a mean logMAR of 1.41 to a mean of 0.94 after surgery. In Sandner's series the mean post-operative logMAR visual acuity increased to 1.87 logMAR[19]. Significant initial anatomical success and a mean final visual acuity of 1.52 logMAR were reported by Tognetto et al[20]. However visual function results are not easy to compare due to differences in previous retinal conditions. In other studies complications after HSO tamponade include severe inflammation, HSO emulsification/dispersion, new retinal tears in the superior retina, retinal vascular changes, cataract, ocular hypertension and hypotension. Inflammatory reactions, including exudation and membrane formation are quite common complications[21].In our series, ocular hypertension was found in 17 patients(34.7%; mean value 25 mm Hg) and was treated with glaucoma drugs. Three of these patients had pre-existing medicallycontrolled glaucoma before surgery. After Densiron 68 removal did ocular pressure returned to normal values only in 4 of the 17 cases (23.5%) while the other cases continued with the glaucoma therapy. Tognetto et al[20] observed 5 cases of ocular hypertension after Densiron 68 tamponade; 3 were easily controlled by medication and 2 were resolved after Densiron 68 removal. Wong et al[18] reported that 6 patients had an IOP higher than 30 mm Hg at the 5-week follow-up after heavy oil surgery and 3 patients had an IOP higher than 30 mm Hg at the last follow-up (3mo after oil removal). All cases of high IOP were successfully treated medically. Sandner et al[19]found an increased IOP during Densiron 68 tamponade in 4 patients: it persisted after silicone oil removal in 3 cases and in all eyes it was treated successfully with topical anti-glaucoma medication. In 13 cases (26.5%) we had inflammatory complications such as emulsion and inflammation in the anterior chamber: a few drops of silicone oil adhered to the posterior capsule and to the iris and/or in the inferior part of the anterior chamber. We found 2 cases of corneal opacification but it is important to remember that the corneal condition was already complex prior to surgery. In 6 cases we had both anterior chamber inflammation and ocular hypertension.Wong et al[18] reported 3 cases of moderate anterior chamber inflammatory activity at 1wk after the initial operation and a minor dispersion of silicone oil detected postoperatively in 3 patients at 1wk and in 6 patients at 1mo follow-up.They had a few drops attached to the posterior capsule and/or in the inferior part of the anterior chamber; none had any retrolental membranes or epiretinal membranes which had been previously observed in case series with F6H8[16]. Sandner et al[19] did not observe chronic inflammatory reaction in the anterior segment or endothelial precipitates in his series but in 3 patients they found a progression of intra-retinal gliosis;this was suspected during the Densiron 68 endotamponade.They also found epiretinal membrane development, probably due to the F6H8 component which activated an inflammatory response and resulted in a considerable intra-retinal gliotic reaction associated with additional retinal shortening, leading to a tractional re-detachment[19]. In contrast to Tognetto et al[20] and Wong et al[18], Sandner et al[19] noted the dispersion of Densiron in 2 eyes with notable pseudohypopyon after 33d and 56d, respectively. Recently Dresp and Menz[22] observed that the tendency of silicone oil to emulsify might be triggered by impurities derived from remnants of heavy liquids used intraoperatively or from residual silicon oil particles located on the vitreoretinal devices.
In conclusion, the retinal re-attachment rate after one surgical operation in our case series is slightly inferior compared with literature but we have to consider the complexity of the cases we selected: 11 eyes (22.4%) had post traumatic RD. We usually use Densiron 68 as a second choice for inferior RD recurrence in eyes which have already undergone PPV with lighter-thanwater gas or SSO endotamponade, which should contrast upper retinal PVR development. Densiron 68 efficiently tamponades the inferior retinal periphery during second surgery for inferior RD recurrence and may lower the risks of PVR in the inferior quadrant. The displacement of the mixture of aqueous humor and growth factors away from the lower retina and the posterior pole to the upper quadrants had been used to contrast PVR and cystoid macular edema development.The purpose of our study was to evaluate the efficacy and safety of Densiron 68 in the treatment of complex retinal redetachments, especially those treated with SSO during the first surgery. In these cases we have found a 25% recurrence rate after Densiron 68 removal with a final re-attachment rate of 81.2%. We believe that Densiron 68 is a useful surgical tool to manage inferior complex RD, as a second step for eyes which have already undergone PPV with a SSO tamponade to contrast inferior PVR development. Further studies are needed to evaluate its use.
ACKNOWLEDGEMENTS
Conflicts of Interest: Caporossi T, None; Franco F, None;Finocchio L, None; Barca F, None; Giansanti F, None;Tartaro R, None; Virgili G, None; Rizzo S, None.
1 Heimann H, Stappler T, Wong D. Heavy tamponade 1: a review of indications, use, and complications. Eye (Lond) 2008;22(10):1342-1359.2 Garweg JG, Tappeiner C, Halberstadt M. Pathophysiology of proliferative vitreoretinopathy in retinal detachment. Surv Ophthalmol 2013;58(4):321-329.3 Schwartz SG, Flynn HW, Lee WH, Wang X. Tamponade in surgery for retinal detachment associated with proliferative vitreoretinopathy.
Cochrane Database Syst Rev 2014;2:CD006126.
4 Russo A, Morescalchi F, Donati S, Gambicorti E, Azzolini C,Costagliola C, Semeraro F. Heavy and standard silicone oil: intraocular inflammation. Int Ophthalmol 2018;38(2):855-867.
5 Parapuram SK, Chang BY, Li L, Hartung RA, Chalam KV, Nair-Menon JU, Hunt DM, Hunt RC. Differential effects of TGFbeta and vitreous on the transformation of retinal pigment epithelial cells. Invest Ophthalmol Vis Sci 2009;50(12):5965-5974.
6 Tan HS, Dell'omo R, Mura M. Silicone oil removal after rhegmatogenous retinal detachment: comparing techniques. Eye (Lond) 2012;26(3):444-447.
7 Choudhary MM, Choudhary MM, Saeed MU, Ali A. Removal of silicone oil: prognostic factors and incidence of retinal redetachment.Retina 2012;32(10):2034-2038.
8 Lappas A, Foerster AM, Kirchhof B. Use of heavy silicone oil(Densiron-68) in the treatment of persistent macular holes. Acta Ophthalmol 2009;87(8):866-870.
9 Kim YK, Gunther B, Meinert H. A new, heavier-than-water silicone oil: a solution of perfluorohexyloctane in polydimethylsiloxane. Eur J Ophthalmol 2005;15(5):627-637.
10 Auriol S, Pagot-Mathis V, Mahieu L, Lemoine C, Mathis A. Efficacy and safety of heavy silicone oil Densiron 68 in the treatment of complicated retinal detachment with large inferior retinectomy. Graefes Arch Clin Exp Ophthalmol 2008;246(10):1383-1389.
11 Levasseur SD, Schendel S, Machuck RW, Dhanda D. High-density silicone oil Densiron-68 as an intraocular tamponade for primary inferior retinal detachments. Retina 2013;33(3):627-633.
12 Stappler T, Heimann H, Gibran SK, Groenewald C, Pearce IA,Wong D. Densiron-68 heavy silicone oil in cases of PVR. Anatomic and functional outcomes. Ophthalmologe 2009;106(4):320-326.
13 MacÍas-Murelaga B, Ruiz M, Bascarán L, Gibelalde A, Aldazabal M, Irigoyen C. Heavy silicone oil (Densiron® 68) in proliferative vitreoretinopathy: 4 years of experience. Arch Soc Esp Oftalmol 2013;88(11):445-449.
14 Hussain RN, Banerjee S. Densiron 68 as an intraocular tamponade for complex inferior retinal detachments. Clin Ophthalmol 2011;5:603-607.15 Liu F, Li H, Feng L, Wang F. Anatomical and functional outcomes after Densiron 68 heavy silicone oil tamponade for complicated retinal detachment in Chinese eyes. Int J Ophthalmol 2014;7(3):469-473.
16 Joussen AM, Kirchhof B, Schrage N, Ocklenburg C, Hilgers RD, HSO Study Group. Heavy silicone oil versus standard silicone oil as vitreous tamponade in inferior PVR (HSO Study): design issues and implications.
Acta Ophthalmol Scand 2007;85(6):623-630.
17 Sandner D, Engelmann K. First experiences with high-density silicone oil (Densiron) as an intraocular tamponade in complex retinal detachment.
Graefes Arch Clin Exp Ophthalmol 2006;244(5):609-619.
18 Wong D, Van Meurs JC, Stappler T, Groenewald C, Pearce IA,McGalliard JN, Manousakis E, Herbert EN. A pilot study on the use of a perfluorohexyloctane/silicone oil solution as a heavier than water internal tamponade agent. Br J Ophthalmol 2005;89(6):662-665.
19 Sandner D, Herbrig E, Engelmann K. High-density silicone oil(Densiron) as a primary intraocular tamponade: 12-month follow up.
Graefes Arch Clin Exp Ophthalmol 2007;245(8):1097-1105.
20 Tognetto D, Minutola D, Sanguinetti G, Ravalico G. Anatomical and functional outcomes after heavy silicone oil tamponade in vitreoretinal surgery for complicated retinal detachment: a pilot study. Ophthalmology 2005;112(9):1574.
21 Mete M, Parolini B, Maggio E, Pertile G. 1000 cSt silicone oil vs heavy silicone oil as intraocular tamponade in retinal detachment associated to myopic macular hole. Graefes Arch Clin Exp Ophthalmol 2011;249(6):821-826.
22 Dresp JH, Menz DH. Interaction of different ocular endotamponades as a risk factor for silicone oil emulsification. Retina 2005;25(7):902-910.