INTRODUCTION
W ith the rapid development of obstetrics and neonatal medical technologies, the treatment for premature infants has made great progress, and diseases associated with premature infants have also increased. In ophthalmology,retinopathy of prematurity (ROP) is a common disease in premature infants[1] and the most important cause of blindness among preschool children[2]. ROP is a progressive and controllable disease, and early screening and treatment play a vital role in stopping ROP in its initial stage to preserve the child's effective vision. In addition to early screening and therapy, following the diopters and related visual treatments is also important to preserving vision in children throughout life. Therefore, we have summarized the incidence of ROP,analyzed outcomes in treatments for ROP, and explored late refractive status. At the Second Affiliated Hospital of Nanchang University, Department of Pediatric Ophthalmology,we began screening the fundus of premature infants in October 2007. To increase our understanding of the eye status of premature children, we have summarized and analyzed data on the incidence of ROP and the refractive status of 562 premature children.
SUBJECTS AND METHODS
Ethical Approval The study protocol conformed to the tenets of the Declaration of Helsinki and was approved by the Ethics Committee of the Second Affiliated Hospital of Nanchang University, China. All participants (or their parents/legal guardians, as applicable) consented to the original measurements and a review of their medical records.
Subjects In all, 562 cases of premature infants who underwent fundus screening in the Department of Pediatric Ophthalmology at the Second Affiliated Hospital of Nanchang University from October 2007 to September 2017.
Included subjects: premature infants who underwent fundus screening in the Outpatient Clinic or by a doctors in the ward.Excluded subjects: term or premature infants who were lost to follow-up before they were 1 year old.
Retinopathy of Prematurity Diagnosis and Treatment
We used “Guidelines for the treatment of premature infants with oxygen and the prevention and treatment of retinopathy(2005)”[3] and “Screening Guidelines for Retinopathy of Prematurity in China (2014)”[4], and “Screening Examination in Premature Infants for Retinopathy of Prematurity (2013)”[5].Based on the lesion site, the retina was divided into 3 regions,and the degree of lesion was divided into 5 stages. The extent of the lesion was calculated as the number of hour points. The treatment criteria were as follows: zone I: ROP in any stage with plus disease or stage 3 with no plus disease, or zone II:stage 2 or 3 with plus disease or stage 4-5 regardless of the zone.
Inspection Content The premature infants' gestational age(GA), the correct GA, birth weight (BW), and any history of asphyxia, oxygen inhalation, rescue, heart and brain disease or systemic condition were collected. From October 2007 to February 2013, fundus screening was performed as an indirect fundoscopy combined with a scleral compressor. From March 2013 to September 2017, fundus screening was performed with a Retcam 3 wide-angle fundus camera combined with indirect fundoscopy. Before the examination, tropicamide phenylephrine eye drops were applied 4 times at 10min intervals. After the examination, an antibiotic gel was applied 2 times/d for three days.
Refractive State Inspection A mydriatic retinoscopy was performed at the age of 6mo in premature infants (tropicamide phenylephrine eye drops, every 10min, three times) and at 1 year old using atropine sulfate eye ointment (atropine sulfate eye ointment, two times a day for three days). The patients were followed up after three weeks. Until 3 years old, atropine ophthalmic gel mydriasis was performed twice per year, then one time per year from 4 to 10 years old. The final results were recorded and statistically analyzed.
General Examination The following examinations were performed: slit lamp, fundus, extraocular muscle function, and A and B ultrasound. Corneal topography and optical coherence tomography (OCT) were performed as appropriate, and older children were tested for logarithmic visual acuity or visual acuity.
Statistical Analysis All statistical analyses were performed using SPSS 22.0. Count data were analyzed by the χ2 test.When n<40, Fisher's exact test was used. The difference was considered statistically significant when P<0.05.
RESULTS
General Information Among the premature infants in whom the fundus of the eye was screened, there were 378 boys (756 eyes), 184 girls (368 eyes), 36 pairs of twins (144 eyes) and 490 infants from single births (980 eyes). The BW was 891-2550 g (mean, 1645.5 g), and the GA at birth was 27wk+5d-37wk (mean, 31.6wk). The Apgar scores were 1-3 points in 46 cases, 4-6 points in 152 cases and 7-10 points in 364 cases(Table 1). A total of 450 cases were given oxygen (different concentrations), and of these, 263 cases involved the use of a breathing machine for a duration of 1-12d (mean, 5.34d). At the time of birth, 162 cases had asphyxia, and 400 cases did not.
Retinopathy of Prematurity Incidence, Treatment and Outcomes There were 93 cases of ROP infants (93/562,16.55%). Of these, 52 cases (52/562, 9.25%) were diagnosed as stage I, 23 cases (23/562, 4.09%) as stage II, 11 cases (11/562,1.96%) as stage III, 2 cases (2/562, 0.36%) as stage IV and 5 cases (5/562, 0.89%) as stage V. All stage IV and V patients occurred before 2010, and were not examined after birth, until the infants could not see anything and had white pupils. Due to economic and ideological constraints, 4 cases with stage V ROP gave up treatment. In these infants, only a little light was visible in one eye of one of the twins, and the remaining 7 eyes did not perceive light (Table 2). The male to female ratio for ROP was 2:1 (61 male infant cases of ROP, 61/378, 16.14%;and 32 female cases of ROP, 32/184, 17.39%), and there was no significant difference in the incidence of ROP between males and females. However, all of the cases of serious ROP(stage VI and V) were male (Table 3, Figure 1).
Table 1 General informations of premature infants
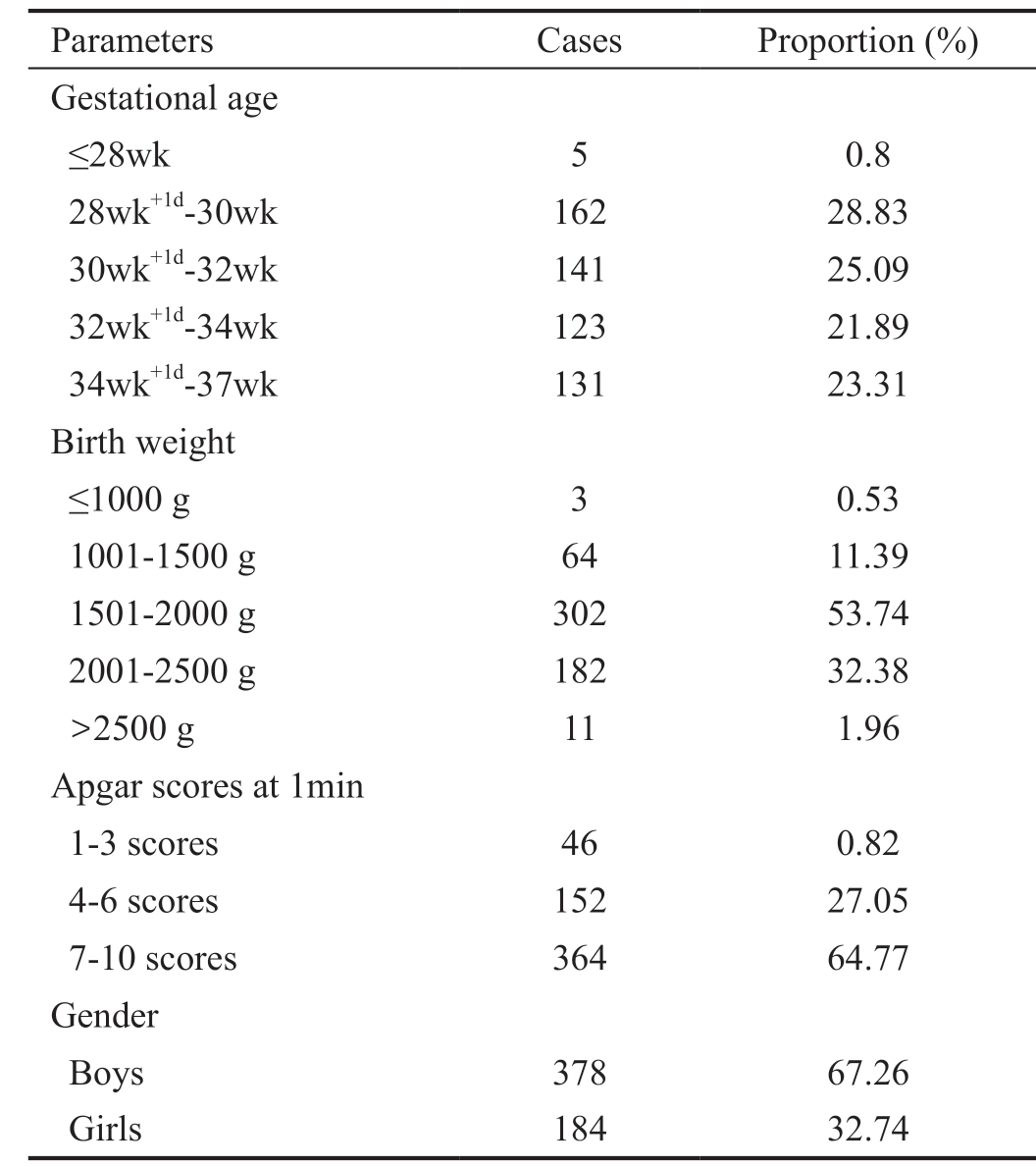
Parameters Cases Proportion (%)Gestational age≤28wk 5 0.8 28wk+1d-30wk 162 28.83 30wk+1d-32wk 141 25.09 32wk+1d-34wk 123 21.89 34wk+1d-37wk 131 23.31 Birth weight≤1000 g 3 0.53 1001-1500 g 64 11.39 1501-2000 g 302 53.74 2001-2500 g 182 32.38>2500 g 11 1.96 Apgar scores at 1min 1-3 scores 46 0.82 4-6 scores 152 27.05 7-10 scores 364 64.77 Gender Boys 378 67.26 Girls 184 32.74
Table 2 ROP incidence, treatment and outcomes

Stages Cases (%) Treatment Outcomes Non-ROP 469 (83.45) - -ROP 93 (16.55) - -Stage I 52 (9.25) Frequent observation Self-healing Stage II 23 (4.09) 18 cases frequent observation, 3 cases intravitreal injection, 2 cases zone 2 plus with endolaser photocoagulation 18 cases self-healing, 3 cases healing after intravitreal injection, 2 cases visible after endolaser photocoagulation,fundus laser scar Stage III 11 (1.96) 5 cases frequent observation, 3 cases intravitreal injection, 2 cases laser photocoagulation, 1 case intravitreal injection+endolaser photocoagulation 5 cases self-healing, 3 cases healing after intravitreal injection, 3 cases visible after endolaser photocoagulation,fundus laser scar Stage VI 2 (0.36) 2 cases vitrectomy+retinal detachment surgery+endolaser photocoagulation Light preception Stage V 5 (0.89) 4 cases give up treatment, 1 case vitrectomy+retinal detachment surgery+endolaser photocoagulation 4 cases (7 eyes) blind without treatment, only 1 eye can perceive light. Both eyes can perceive light after surgey
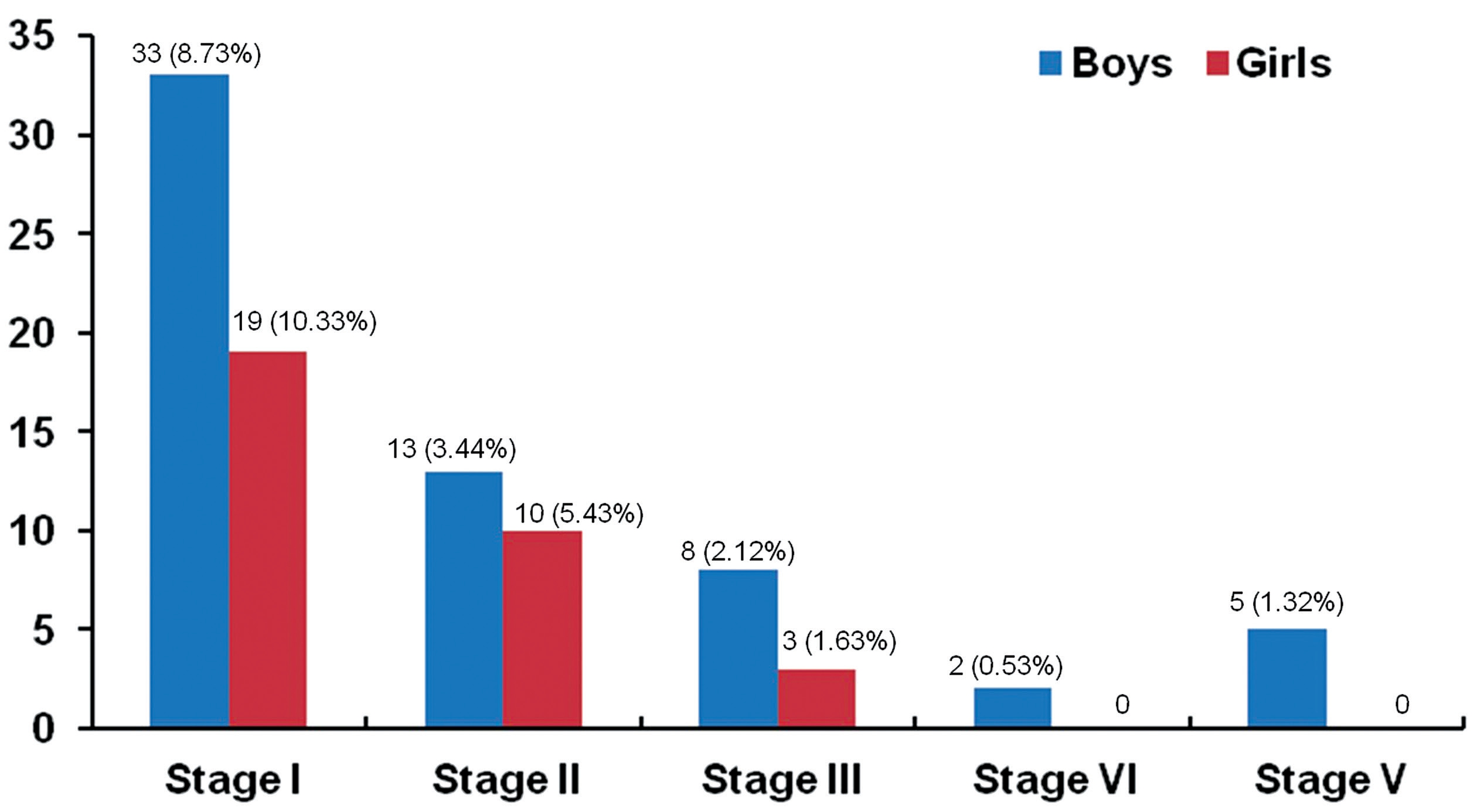
Figure 1 Proportion of ROP stages of boys and girls in premature infates.
Table 3 ROP incidence of males and females in premature infants
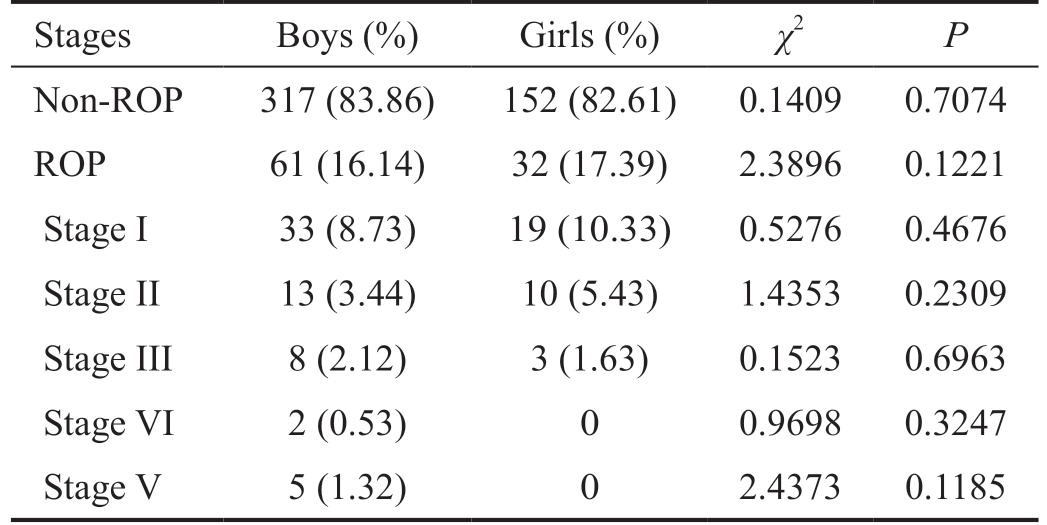
Stages Boys (%) Girls (%) χ2 P Non-ROP 317 (83.86) 152 (82.61) 0.1409 0.7074 ROP 61 (16.14) 32 (17.39) 2.3896 0.1221 Stage I 33 (8.73) 19 (10.33) 0.5276 0.4676 Stage II 13 (3.44) 10 (5.43) 1.4353 0.2309 Stage III 8 (2.12) 3 (1.63) 0.1523 0.6963 Stage VI 2 (0.53) 0 0.9698 0.3247 Stage V 5 (1.32) 0 2.4373 0.1185
Analysis of Refractive Results of Premature Infants The results of mydriasis (atropine sulfate eye ointment) were recorded in all but 2 cases of stage IV and 5 cases of stage V ROP. The first time the mydriasis results were recorded when the premature infants were 1 year old. Among the premature infants, 205 cases were 1-3 years old (205/562, 36.48%), 256 were 3-7 years old (256/562, 45.55%), and 101 were 8-10 years old (101/562, 17.97%). In refractive type patients, myopia combined with astigmatism was more common (30.99%)and was followed by hyperopia (27.75%) and hyperopia with astigmatism (27.21%). With regard for refractive degree (D),0-2.00 D was the most common (45.95%) and was followed by 2.00-4.00 D (32.79%), whereas >8.00 D was rare (3.42%). In the non-ROP group, hyperopic refraction (including hyperopia and hyperopia combined with astigmatism) was more common(266/469 cases, 56.72%), however, in the ROP group, myopic refraction (including myopia and myopia combined with astigmatism) was more common (42/86 cases, 48.84%).Among the diopters, 0-2.00 D was the most common and was followed by 2.00-4.00 D. In the > 8.00 D group, the incidence of ROP was significantly higher than in the non-ROP group(Table 4).
In the ROP-treated group, myopic refraction (including myopia and myopia combined with astigmatism) was the most common (7 cases, 7/11, 63.63%), with 9 cases >4.25 D (9/11,81.82%) and 4 cases >8.00 D (4/11, 36.36%; Table 5).
DISCUSSION
ROP is the leading cause of blindness in preschool children and a heavy burden on affected families and society. However,ROP is a disease that progresses after birth, and it can therefore be stopped before advancing to more severe stages. Individuals who undergo fundus screening and timely treatment have a good prognosis. Hence, it is the most important factor to check in early screening. Since 2005, the “Guidelines for the treatment of premature infants with oxygen and the prevention and treatment of retinopathy”, which is promulgated by the National Health Commission of China and published by the Chinese Medical Association[3], has actively promoted treating premature infants for and preventive treatments against ROP in China. Our ROP fundus screening covers more than 10y,and during this time, we have seen many changes, including advancements in the field from ignorance to knowledge,movement from only initial awareness to an improved awareness of the importance of screening, and a shift from practitioners asking parents of premature infants to come to see a doctor to parents taking the initiative to bring their premature infants to a screening. The screening machine involves indirect ophthalmoscopy and Retcam 3 wide-angle fundus photography. This is a process used in pediatrics, including ophthalmologists, obstetricians and pediatricians, to recognize ROP in China.
Even with developments in screening, it is not enough to focus only on retinal vascularization when premature infantsreach 40wk of corrected GA. Visual developmental processes are different between mature and premature children, who had premature birth, ROP or treatment for ROP, and early screening and treatment may achieve effective eyesight in premature infants. However, premature children need to improving the quality of their visual acuity by follow-up observation after birth, follow-up of visual development at later stage. So visual problems can be identified in time and actively treated. Implementing these practices would help these premature children to adapt to society and life in a healthier manner. Therefore, in this retrospective study, in addition to analyzing the incidence of ROP in children, we also focused on the refractive state in premature children to provide a reference for other doctors so that they can perform better clinical work.In this retrospective analysis, 562 premature infants were involved in the collection of examination and data. The average GA at birth was 31.6wk, and 308 cases (308/562,54.80%) were born at younger than 32wk of gestation. Only 5 cases were born at younger than 28wk of gestation. The youngest premature infant was born at a GA of 27wk+5d, and no younger infants received a fundus examination. The because of the coverage provided at the local pediatric rescue level,with parents taking smaller and more premature infants to other institutions. The average BW was 1645.5 g. The smallest infant was only 891 g, and the ROP in this infant was stage I in zone 2 and self-healed without treatment. From the above data,we determined that BW did not directly influence the incidence of ROP[6]. In this study, the incidence of ROP was 16.55%(93/562 cases), which is almost the same as that found in other cities in China[7-8]. The male/female gender ratio of premature infants who were screened for ROP in our hospital between 2007 and 2009 was 14/1[9], which is very high. In the following eight years, the male/female gender ratio of premature infants who underwent fundus screening gradually trended toward 2/1 but remained higher than both the male/female sex ratio at birth (106.67/100, from the National Population Census, the sixth census bulletin in 2010, on 23 July 2012). Therefore, we performed a gender-specific analysis of the incidence of ROP.In this study, the incidence of ROP was 16.14% (33/378 cases)in boys and 17.39% (32/184 cases) in girls, and this difference was not significant. However, all of the cases of serious ROP(stage IV and V) occurred in male infants. Gender was found to be a risk factor for ROP in a previous study, and more males than females suffer visual impairment resulting from ROP[10-12]. It is possible that the proportion of cases involving placenta previa, the premature birth rate, hypoxia and other factors might be higher or more common in male fetuses than in female fetuses. Moreover, the time required for the brain to
mature is longer and the development of the nervous system occurs more slowly in male infants than in female infants.Therefore, visual impairments that occur after birth are more serious in boys than in girls. Premature infants, especially boys, often experience brain function disorders[13].
Table 4 Type of refraction in premature infants n (%)

Refraction Total 0-2.00 D 2.00-4.00 D 4.25-6.00 D 6.25-8.00 D >8.00 D Non-ROP ROP Non-ROP ROP Non-ROP ROP Non-ROP ROP Non-ROP ROP Myopia 44 (7.93) 18 (40.91) 4 (9.09) 13 (29.55) 3 (6.82) 2 (4.55) 0 1 (2.27) 0 2 (4.55) 1 (2.27)Myopia with astigmatism 172 (30.99) 77 (44.77) 16 (9.30) 40 (23.26) 8 (4.65) 12 (6.98) 3 (1.74) 7 (4.07) 3 (1.74) 2 (1.16) 4 (2.33)Hyperopia 154 (27.75) 59 (38.31) 7 (4.55) 40 (25.97) 5 (3.25) 20 (12.99) 3 (1.95) 11 (7.14) 3 (1.95) 5 (3.25) 1 (0.65)Hyperopia with astigmatism 151 (27.21) 48 (31.79) 6 (3.93) 52 (34.44) 8 (5.30) 19 (12.58) 3 (1.99) 9 (5.96) 2 (1.32) 3 (1.99) 1 (0.66)Astigmatism 34 (6.13) 18 (52.94) 2 (5.88) 11 (32.35) 2 (5.88) 0 1 (2.94) 0 0 0 0 Total 555 (100) 220/469(46.91)35/86(40.70)156/469(33.26)26/86(30.23)53/469(11.30)10/86(11.63)28/469(5.97)8/86(9.30)12/469(2.56)7/86(8.14)χ2 - 1.1287 0.3027 0.0077 1.3303 6.8463 P-0.2881 0.5822 0.9299 0.2488 0.0089
Table 5 ROP with treat, refraction of premature infants
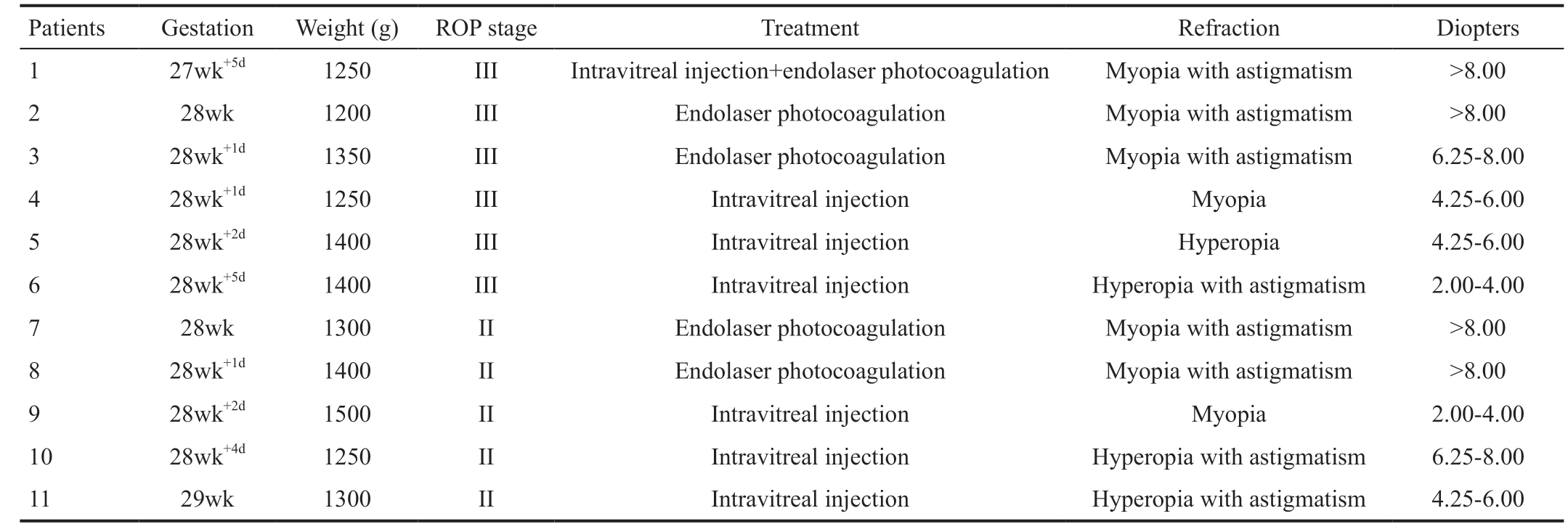
Patients Gestation Weight (g) ROP stage Treatment Refraction Diopters 1 27wk+5d 1250 III Intravitreal injection+endolaser photocoagulation Myopia with astigmatism >8.00 2 28wk 1200 III Endolaser photocoagulation Myopia with astigmatism >8.00 3 28wk+1d 1350 III Endolaser photocoagulation Myopia with astigmatism 6.25-8.00 4 28wk+1d 1250 III Intravitreal injection Myopia 4.25-6.00 5 28wk+2d 1400 III Intravitreal injection Hyperopia 4.25-6.00 6 28wk+5d 1400 III Intravitreal injection Hyperopia with astigmatism 2.00-4.00 7 28wk 1300 II Endolaser photocoagulation Myopia with astigmatism >8.00 8 28wk+1d 1400 II Endolaser photocoagulation Myopia with astigmatism >8.00 9 28wk+2d 1500 II Intravitreal injection Myopia 2.00-4.00 10 28wk+4d 1250 II Intravitreal injection Hyperopia with astigmatism 6.25-8.00 11 29wk 1300 II Intravitreal injection Hyperopia with astigmatism 4.25-6.00
In this retrospective study, to ensure accuracy, for the refraction results, we used only mydriatic results in which atropine sulfate eye ointment was applied after the premature infants were 1 year old. Which refractive media were used in children with ROP VI and V was not clear, and those refractive results were therefore not recorded. In a previous study[14-15],simple hyperopia was more common in mature infants than in premature infants, and astigmatism was more common in premature infants than in mature infants, especially severe astigmatism and mixed astigmatism. In this long-term retrospective study, myopia combined with astigmatism was more common in premature infants (172/555, 30.99%). In non-ROP premature children, hyperopic refractive states (including simple hyperopia and hyperopia combined astigmatism)occurred in 266/469 of the cases (56.72%). These results are in agreement with the development of refraction in children.However, in ROP infants, myopia refractive states (including myopia and myopia combined astigmatism) were more common, occurring in 42/86 cases (48.84%), while hyperopic refractive states (including hyperopia and hyperopia combined astigmatism) were less common than myopic refractive states, occurring in 39/86 of the cases (45.35%). These results were not in agreement with the development of refraction in children. The 0-2.00 D was the most common and was followed by 2.00-4.00 D. There were no differences between the ROP and non-ROP groups in the 0-8.00 D group. However,>8.00 D was significantly more common in the ROP group than in the non-ROP group. In the treated ROP infants, myopia refractive states (including myopia and myopia combined with astigmatism) were the most common, affecting up to 7 cases (7/11,63.63%), while 9 cases (9/11, 81.82%) were in the >4.25 D group, and 4 cases (4/11, 36.36%) were in the >8.00 D group.
Previous studies have shown that the refractive state of human newborns is hyperopic and exhibits a few regular astigmatisms.As the eyeball develops, hyperopia and astigmatism gradually decrease and develop into emmetropia. This process is called the “process of emmetropization”[16]. During this process, a static refraction of +2.00 D is a normal physiological refraction in 4-6 year old children and reflects the development process by which diopters change in children with normal visual acuity.The development of ocular refraction is broken in children with a preterm birth or ROP treated with a drug or laser or surgical treatment. In addition, premature infants always lack part of embryonic development, even when they do not exhibit severe ROP or require treatment simply because of their low body weight or other factors, such as anoxia, pregnancy complications, and intrauterine growth retardation[17]. A preterm birth can also cause refractive abnormalities in infancy that can extend to childhood, affecting the development of visual acuity. Deng et al[18] compared ocular morphology between premature infants without ROP and mature infants in six-month-old to 1-year-old children and found that the ocular axis was shorter, the anterior chamber was shallower, and the curvature of the cornea was higher in the preterm infants. Then,the hyperopia diopter was lower in premature infants than in mature infants, and these cases can easily develop into myopia and astigmatism. Even if the children do not have obvious ROP, it is still possible that the peripheral retina will exhibit small pathological changes, little traction, and early ischemia to optic nerve color changes[19]. Although a fundus examination cannot detect the changes that occur in later stages, it is still possible that there can be adverse effects on the refractive development of premature infants. In ROP children treated with laser therapy, 81.82% were >4.25 D (9/11 cases), and of these, 36.36% (4/11 cases) were >8.00 D. This proportion is far higher than that observed in >8.00 D premature infants without ROP (2.56%, 12/469 cases) and in preterm infants with ROP(8.14%, 7/86 cases; including auto reversion and treatment).Previous studies have shown that premature infants have high myopia, especially in zone 1 ROP, after laser photocoagulation retinal photocoagulation[20-21]. After laser photocoagulation retinal photocoagulation treatment for ROP, retinal scarring can appear, the eyeball axis becomes elongated, and myopia increases[19].
Therefore, by tracking changes in the fundus and diopters of premature infants for 10y, we found that myopia combined with astigmatism was common in premature infants with or without ROP (30.99%, 172/555 cases) and that myopic refraction(including myopia and myopia combined with astigmatism)was more common in premature infants with ROP (48.84%,42/86 cases). In the >8.00 D group, there were significantly more patients with ROP than without ROP. Myopic refraction(including myopia and myopia and astigmatism) was most common in children with ROP after treatment (63.63%,7/11 cases). Therefore, we can infer from these data that the refractive state is different between premature infants and mature infants who undergo emmetropization from hyperopia to emmetropia. In particular, in children with ROP, those with ROP treatment have a higher chance of developing myopia,astigmatism, and higher diopters. We used the process of refraction to determine the ocular characteristics of premature infants and found that it was conducive to performing special and targeted refractive tracing and vision correction in laterstage premature infants. Timely treatment helps these children achieve better visual function and quality of life.
ACKNOWLEDGEMENTS
Foundation: Supported by Health and Family Planning Commission of Jiangxi Province (No.20131080).
Conflicts of Interest: Deng Y, None; Yu CH, None; Ma YT,None; Yang Y, None; Peng XW, None; Liao YJ, None; Xiong WW, None; Wu JS, None; Mao HW, None; Yin XL, None.
1 Beligere N, Perumalswamy V, Tandon M, Mittal A, Floora J, Vijayakumar B, Miller MT. Retinopathy of prematurity and neurodevelopmental disabilities in premature infants. Semin Fetal Neonatal Med 2015;20(5):346-353.
2 Chang KM, Patel DK, Tajunisah I, Subrayan V. The trend of retinopathy of prematurity in Malaysia from 1992 to 2001 based on a nationwide blind schools study. Asia Pac J Public Health 2015;27(2):217-224.
3 Chinese Ophthalmological Society. Guidelines for the treatment of premature infants with oxygen and the prevention and treatment of retinopathy. Zhonghua Yan Ke Za Zhi 2005,41:375-376.
4 Chinese Ophthalmological Society. Screening Guidelines for Retinopathy of Prematurity in China (2014). Zhonghua Yan Ke Za Zhi 2014;50(12):933-935.
5 Fierson WM; American Academy of Pediatrics Section on Ophthalmology; American Academy of Ophthalmology; American Association for Pediatric Ophthalmology and Strabismus; American Association of Certified Orthoptists. Screening examination of premature infants for retinopathy of prematurity. Pediatrics 2013;131(1):189-195.
6 Ozdemir O, Tunay ZO, Acar DE, Acar U. Refractive errors and refractive development in premature infants. J Fr Ophtalmol 2015;38(10):934-940.7 Liu Q, Yin ZQ, Ke N, et al. Incidence of retinopathy of prematurity in southwestern China and analysis of risk factors. Med Sci Monit 2014;20:1442-1451.
8 Wu T, Zhang L, Tong Y, Qu Y, Xia B, Mu DZ. Retinopathy of prematurity among very low-birth-weight infants in China: incidence and perinatal risk factors. Invest Ophthalmol Vis Sci 2018;59(2):757-763.
9 Deng Yan, Yu C, Liao Y, Yang Y, Peng X, Yin X. Clinical analysis of retinopathy of prematurity. Practical Clinical Medicine 2009;10(5):90-92.10 Jacobson L, Hård AL, Horemuzova E, Hammarén H, Hellström A. Visual impairment is common in children born before 25 gestational weeks: boys are more vulnerable than girls. Acta Paediatr 2009;98(2):261-265.
11 Rozema JJ, Herscovici Z, Snir M, Axer-Siegel R. Analysing the ocular biometry of new-born infants. Ophthalmic Physiol Opt 2018;38(2):119-128.
12 Hellström A, Smith LE, Dammann O. Retinopathy of prematurity. The Lancet 2013;382(9902):1445-1457.
13 Skiöld B, Alexandrou G, Padilla N, Blennow M, Vollmer B, Adén U. Sex differences in outcome and associations with neonatal brain morphology in extremely preterm children. J Pediatr 2014;164(5):1012-1018.
14 Deng Y, Liao Y, Yang Y, Yu C, Peng X, Yin X. Refractive error's distribution and clinical characteristics of preterm and full-term children.Yan Ke Xue Bao 2010;25(2):93-95.
15 Uprety S, Morjaria P, Shrestha JB, Shrestha GS, Khanal S. Refractive status in nepalese pre-term and full-term infants early in life. Optom Vis Sci 2017;94(10):957-964.
16 Somer D, Karabulut E, Cinar FG, Altiparmak UE, Unlu N.Emmetropization, visual acuity, and strabismus outcomes among hyperopic infants followed with partial hyperopic corrections given in accordance with dynamic retinoscopy. Eye (Lond) 2014;28(10):1165-1173.
17 Yu SJ, Liu GH, Liu Y, Huang J, Han ML, Zhao BJ, Gai ZT. The evolution of refractive status in Chinese infants during the first year of life and its affected factors. Int J Ophthalmol 2017;10(8):1290-1294.
18 Deng Y, Yu C, Liao Y, Yang Y, Peng X, Yin X. Clinical analysis of color abnormality and outcome of optic disc in premature infants.
Guangdong Medical Journal 2009;30(11):1667-1668.
19 Lok JYC, Yip WWK, Luk ASW, Chin JKY, Lau HHW, Young AL.Visual outcome and refractive status in first 3 years of age in preterm infants suffered from laser-treated Type 1 retinopathy of prematurity(ROP): a 6-year retrospective review in a tertiary centre in Hong Kong.Int Ophthalmol 2018;38(1):163-169.
20 Yang CS, Wang AG, Shih YF, Hsu WM. Long-term biometric optic components of diode laser-treated threshold retinopathy of prematurity at 9 years of age. Acta Ophthalmol 2013;91(4):e276-e282.
21 Geloneck MM, Chuang AZ, Clark WL, Hunt MG, Norman AA,Packwood EA, Tawansy KA, Mintz-Hittner HA, BEAT-ROP Cooperative Group. Refractive outcomes following bevacizumab monotherapy compared with conventional laser treatment: a randomized clinical trial.JAMA Ophthalmol 2014;132(11):1327-1333.