INTRODUCTION
P seudophakic retinal detachment (RD) is a sight threatening condition accounting for 10% to 40% of total rhegmatogenous retinal detachment (RRD) cases[1-2],though it is a rare complication of cataract surgery with a reported incidence of 0.4% to 4.9%[3]. Risk factors may include intraoperative posterior capsular tear, vitreous loss or postoperative YAG laser capsulotomy[4]. Pneumatic retinopexy, scleral buckling (SB) and pars plana vitrectomy(PPV) are all recognized options for treatment[5]. SB is a time tested procedure that is considered the procedure of choice for certain cases such as myopic young patients with attached posterior hyaloid, retinal dialysis, shallow detachment with inferior breaks[6], atrophic holes in lattice and extensive lattice degeneration with abnormal peripheral vitreoretinal interface or multiple breaks along the vitreous base[7]. Chandelier assisted SB using different wide angle viewing (WAV) systems was recently described for management of RRD with encouraging results[8-13] but most of the cases enrolled in these studies were phakic eyes with only sporadically reported pseudophakic eyes.PPV is more commonly performed compared to conventional SB in repairing RRD in patients with pseudophakia[2].This is mainly due to poor visualization with the indirect ophthalmoscope in pseudophakic eyes caused by poor pupil dilation, residual cortical remnants, opacified capsule or optical aberrations induced by the intraocular lens (IOL)[14].Using a different method for intraoperative visualization in SB like chandelier illumination and WAV contact lens can enhance visualization. It is also important to note that PPV is the preferred technique for many surgeons nowadays for management of RRD either in phakic or pseudophakic eyes owing to the recent advances in vitrectomy machines, high speed cutters, small gauge instruments, endoillumination and WAV systems. Another contributing factor is the increased familiarity and experience with PPV technique compared to SB that is rather declining in popularity among surgeons[2].Performing SB using such familiar tools that are implemented in PPV may improve on this limitation as well.
In this study, we report on the use of chandelier assisted SB using WAV contact lens in 21 pseudophakic eyes to evaluate its anatomical success rate, functional visual outcome and possible complications.
SUBJECTS AND METHODS
Ethical Approval All patients signed a written informed consent for SB surgery. An Institutional Review Board approval was obtained and the study protocol was adherent to the tenets of Declaration of Helsinki.
Study Design and Participants A retrospective non comparative case series study included 21 consecutive eyes with primary pseudophakic RD in which the technique of chandelier assisted SB using WAV contact lens was performed. Procedures were done by two vitreo-retinal surgeons; Nossair AA and Ewais WA at a Tertiary Care Hospital during the period from May 2013 to July 2016.
Preoperative Evaluation Baseline characteristics such as age, sex, medical history and ocular history including duration of RD symptoms, date of cataract surgery and history of YAG laser capsulotomy in case of opened posterior capsule were recorded. Preoperative anterior segment examination,corrected distance visual acuity (CDVA) assessment and intraocular pressure (IOP) measurement were performed.Fundus examination was done using indirect ophthalmoscope and contact lens biomicroscopy. Preoperative refraction was obtained from the patient's latest prescription in case of detachments involving the macula where refraction measurement was not feasible. Cases with simple pseudophakic RD were included while exclusion criteria were the presence of grade C proliferative vitreo-retinopathy (PVR), macular hole or breaks posterior to the equator, giant retinal tear or breaks larger than 3 disc diameters, undetectable breaks and traumatic cases or retinal dialysis, as well as severely complicated cases of cataract surgery noted by the presence of vitreous strands in anterior chamber, absent posterior capsule,aphakia, anterior chamber IOL, cortical remnants or dropped nuclear fragments. Exclusion criteria also included poor visualization due to poorly dilated pupil, opaque media such as vitreous hemorrhage or capsular opacification and the presence of glaucoma, uveitis or history of intraocular surgery other than cataract extraction.
PVR was graded according to the updated Retina Society Classification[15].
The type, site, size and number of retinal breaks were recorded in addition to RD extent including quadrant and macular involvement. Small breaks were defined as less than 0.5 disc diameter in its longest meridian and breaks between 0.5 and 2 disc diameters were defined as medium sized, while breaks between 2 and 3 disc diameters were considered large breaks.Surgical Technique All operations were performed under general anesthesia (GA). Appropriate sterilization and surgical draping were applied. Hooking of the four recti and isolation by 4/0 silk suture after 360 conjunctival periotomy was followed by insertion of a 25-gauge trocar with valved cannula and introduction of a 25-gauge chandelier endo-illuminator(Alcon, Chandelier lighting system, Fort Worth, TX, USA).Chandelier light was inserted 180 degree away from retinal breaks. If this was not applicable due to breaks in multiple quadrants, it was inserted at 6 o'clock.
Self-stabilizing Volk WAV contact lens (Mini Quad; Volk,Mentor, OH, USA) was applied after coating the corneal surface with methylcellulose. Retinal breaks were localized under viewing of surgical microscope equipped with an inverter while applying scleral indentation followed by cryotherapy to retinal break edges. Indications for band use included retinal breaks in multiple quadrants; grade B PVR or extensive lattice degeneration. The endo-illuminator and contact lens were removed and scleral buckle was sutured using 5/0 ETHIBOND (Ethicon, USA). Buckle height and site were evaluated and adjusted if necessary after chandelier reintroduction and contact lens application. Anterior chamber paracentesis and air injection were done in all cases while external drainage of subretinal fluid was performed when needed. Finally, trocar-cannula was removed and scleral wound was sutured followed by conjunctival closure using 8/0 VICRYL suture (Ethicon, USA). Intraoperative complications were recorded.
Postoperative Evaluation Postoperative follow up included anterior segment examination, refraction, CDVA assessment,IOP measurement and fundus examination. Anatomical success and postoperative complications were evaluated. Primary anatomical success of the technique was defined as complete retinal reattachment after 6mo following a single intervention.
Data Analysis Statistical analysis was done using SPSS software version 16.0 (SPSS Inc., Chicago, IL, USA). Decimal notation of CDVA was converted to logMAR units. Dichotomous variables were expressed as numbers and percentages.Descriptive data analysis for independent variables was expressed as mean±standard deviation, median, mode and range. Independent sample t-test with unequal variance was performed to compare independent variables. Comparison between preoperative and postoperative spherical equivalent,CDVA and IOP was done using paired t-test. Pearson coefficient test was used to study correlation. The association between preoperative macular status and postoperative CDVA was assessed using linear regression. P value <0.05 was regarded statistically significant.
RESULTS
Baseline characteristics including demographic and preoperative data were described in Table 1.
Primary anatomical success was achieved in 19 eyes (90.48%).Two (9.52%) eyes developed retinal re-detachment due to PVR. These two eyes were associated with significantly increased number of retinal breaks (P<0.0001), more extensive
Table 1 Baseline patient characteristics mean±SD, n (%)
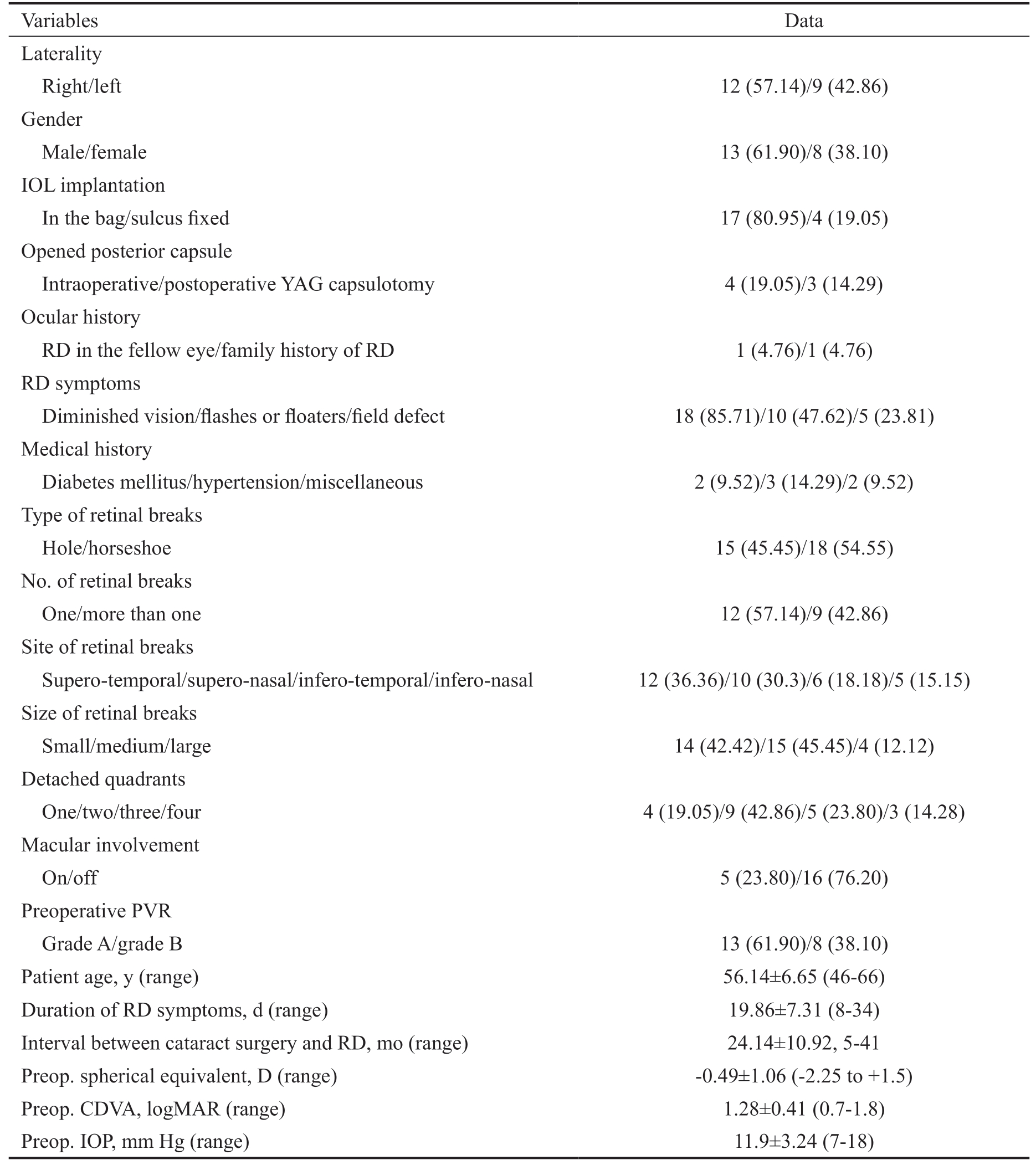
Variables Data Laterality Right/left 12 (57.14)/9 (42.86)Gender Male/female 13 (61.90)/8 (38.10)IOL implantation In the bag/sulcus fixed 17 (80.95)/4 (19.05)Opened posterior capsule Intraoperative/postoperative YAG capsulotomy 4 (19.05)/3 (14.29)Ocular history RD in the fellow eye/family history of RD 1 (4.76)/1 (4.76)RD symptoms Diminished vision/flashes or floaters/field defect 18 (85.71)/10 (47.62)/5 (23.81)Medical history Diabetes mellitus/hypertension/miscellaneous 2 (9.52)/3 (14.29)/2 (9.52)Type of retinal breaks Hole/horseshoe 15 (45.45)/18 (54.55)No. of retinal breaks One/more than one 12 (57.14)/9 (42.86)Site of retinal breaks Supero-temporal/supero-nasal/infero-temporal/infero-nasal 12 (36.36)/10 (30.3)/6 (18.18)/5 (15.15)Size of retinal breaks Small/medium/large 14 (42.42)/15 (45.45)/4 (12.12)Detached quadrants One/two/three/four 4 (19.05)/9 (42.86)/5 (23.80)/3 (14.28)Macular involvement On/off 5 (23.80)/16 (76.20)Preoperative PVR Grade A/grade B 13 (61.90)/8 (38.10)Patient age, y (range) 56.14±6.65 (46-66)Duration of RD symptoms, d (range) 19.86±7.31 (8-34)Interval between cataract surgery and RD, mo (range) 24.14±10.92, 5-41 Preop. spherical equivalent, D (range) -0.49±1.06 (-2.25 to +1.5)Preop. CDVA, logMAR (range) 1.28±0.41 (0.7-1.8)Preop. IOP, mm Hg (range) 11.9±3.24 (7-18)
RD (P<0.0001), poorer preoperative CDVA (P<0.001), and lower preoperative IOP (P<0.01). Other factors such as age(P=0.7) or duration of RD (P=0.3) did not show any statistical significance.
Segmental tire alone was used in 5 eyes (23.81%), and combined with encircling band in 7 eyes (33.33%). Radial sponge alone was used in 3 eyes (14.29%) and combined with encircling band in 6 eyes (28.57%). External drainage of subretinal fluid was performed in 8 eyes (38.10%). Vitreous prolapse at sclerotomy site occurred in 4 eyes (19.05%). One eye (4.76%) developed localized subretinal hemorrhage at the site of external drainage. No case of accidental needle perforation, IOL displacement, retinal incarceration or iatrogenic retinal tear was detected.
Early postoperative complications of the technique included choroidal detachment in one eye (4.76%) and high IOP(>26 mm Hg) in two eyes (9.52%) which was controlled by topical timolol maleate 0.5%. Late postoperative complications included epiretinal membrane formation in one eye (4.76%),PVR in three eyes (14.29%) and extraocular muscle imbalance in one eye (4.76%). A myopic shift of (1.49) diopter was noted in comparison to preoperative refraction. At final follow up 2 cases (9.52%) had chronic ocular discomfort that was controlled by artificial tears and topical non-steroidal antiinflammatory drugs (NSAIDS). No case of buckle extrusion,orbital cellulitis or endophthalmitis was observed.
Mean final CDVA was 0.7±0.3 logMAR units. The 28.6% and 47.6% had postoperative CDVA of 6/12 and 6/18 respectively.
Table 2 Descriptive statistics of postoperative outcomes

Parameters Mean (range) Standard deviation Median Mode Follow up period (mo) 24.09 (6-42) 10.78 26 37 Final postop. spherical equivalent (D) -1.98 (-3.5 to -0.5) 0.85 -2 -1.5 Final postop. CDVA (logMAR) 0.7 (0.3-1.3) 0.3 0.7 0.5 Final postop. IOP (mm Hg) 14.29 (9-19) 2.83 14 15
Macula on detachments were significantly associated with a better postoperative CDVA (P=0.004).
Descriptive statistics of postoperative data were included in Table 2.
DISCUSSION
PPV is a good option for man agement of pseudophakic RD but it is not free of draw backs. Indeed, vitrectomized pseudophakic eyes are more vulnerable to postoperative IOP elevation[16] and corneal endothelial cell loss[17]. There is also some evidence that a failed initial repair is accompanied by an aggressive form of PVR in vitrectomized eyes[18].Although performing PPV in pseudophakic eyes obviates the complication of crystalline lens injury and cataract progression,IOL displacement can still develop in case of opened posterior capsule or damaged zonules. Intraoperative air condensation behind the IOL during fluid air exchange or air migration into the anterior chamber may jeopardize clear surgical view as well. Furthermore, it is believed that vitrectomized eyes may respond differently to intravitreal drug injections such as antibiotics, steroids or anti VEGFs due to rapid drug clearance[19]. Therefore, avoiding PPV and preserving the vitreous can play an important therapeutic role if these injections are required. Avoiding PPV also decreases the rate of iatrogenic breaks and eliminates the use of vitreous substitutes and postoperative positioning. On the other hand, it is more convenient to place a buckle for peripheral breaks anterior to the equator which is a common encounter in pseudophakic RD.Placing a buckle helps in retinal reattachment by decreasing the magnitude and changing the direction of vitreous traction in addition to minimizing vitreous fluid flow through retinal breaks.
In 2012, Aras et al[8] introduced the technique of chandelier assisted SB using a torpedo light. They conducted the study on 16 patients including 4 patients with pseudophakia. Gogia et al[9], in 2014 described the results of 23 cases including 8 pseudophakic eyes. The later study reported preoperative undetectable breaks in 5 pseudophakic eyes but intraoperative localization of retinal breaks was achieved in all of them due to improved visualization by this technique. According to Gogia et al[9], initial retinal reattachment was observed in 22 out of 23 eyes with a success rate of 95.6%. The largest study on chandelier assisted SB till now was conducted on 79 eyes of
which three eyes only were pseudophakics. In the later study,the initial and final anatomical success rates were 92.4% and 100%, respectively[10]. All of the aforementioned studies used non-contact WAV systems.
The technique of chandelier assisted SB using WAV contact lens was described by Nam et al[12] in 2013 but unfortunately,no patient results were included in their study. Another group reported the use of WAV contact lens in 10 patients including 2 pseudophakic patients with a success rate of 90%[13]. A similar technique was applied in this study by using the Volk miniquad contact lens which avoided the peripheral image distortion that commonly occurs during indentation in non-contact WAV systems, as contact lens can decrease corneal reflections and aberrations[20]. In the current study, a panoramic view up to 130 degree ensured visualization of peripheral retinal breaks that otherwise could not have been easily detected by the indirect ophthalmoscope. Contact lens use also prevented corneal dryness and intraoperative epithelial defects.Moreover, the self-stabilizing design of the lens avoided ring suturing and allowed its repeated application and removal, as the chandelier and contact lens were removed during suturing of the buckle to avoid interference with visualization or motility of the globe.
It is worth mentioning that all cases were done under GA.In our routine practice we prefer GA to orbital blocks in SB surgery due to the prolonged, unpredictable and uncomfortable nature of the procedure[21] as incomplete akinesia from partial orbital blockade may increase both surgeon dissatisfaction[22]and patient discomfort.
Using the surgical microscope in SB procedure can prevent the relatively frequent musculoskeletal disorders among vitreoretinal surgeons[23] and decrease the surgical time by avoiding the repeated wearing and removal of the indirect ophthalmoscope[2]. More importantly, adjustable magnification can be used at any step while sharing the surgical view with trainees through the monitor or assistant microscope.
Anatomical success rate of conventional SB varies between 60% and 80% in eyes with pseudophakia. Failure is mainly caused by undetected anteriorly located small retinal tears and PVR[24]. As PPV was suggested to decrease the rate of re-detachment by more efficient detection of peripheral retinal lesions[25], some previous studies reported that PPV can provide higher initial[26] and final reattachment rates[27]in pseudophakic eyes compared to SB. On the other hand,contradictory observations were obtained from several studies that showed similar final vision[26-29], primary success[27-28] and final success rates[26] among both techniques. Interestingly,combining SB with PPV did not enhance visual or anatomical outcomes compared to PPV alone[29-31]. In spite of this controversy, SB remains a good option for management of simple pseudophakic RD[32].
In the current study, primary success rate was 90.48%. Retinal re-detachment was observed in 2 eyes due to PVR. PPV and silicone oil injection was successfully performed for these 2 eyes. Another case developed macular pucker. The patient was satisfied with his vision and refused additional intervention. A total of 3 eyes had postoperative PVR (14.29%). Large breaks and grade C-PVR are known predictors for PVR[33]. Untreated opened breaks and unnecessary excessive cryotherapy in case of poorly visualized breaks can also predispose to inflammation and PVR. In the current study, significant incidence of postoperative PVR was reported despite that cases with large breaks or grade C-PVR were excluded, and although accurate localization of retinal breaks and precise cryotherapy application were achieved in all patients. Nevertheless, the encountered cases of primary failure and PVR in the study were significantly related to more extensive RD, lower preoperative IOP, higher number of retinal breaks and poorer preoperative visual acuity.
Indeed, postoperative pain and inflammation are common after SB. While short term pain is much more common and severe, pain relief can be achieved by different treatment interventions[34]. In this study, a pain score like VAS or NRS was not applied during postoperative period but at final follow up we identified 2 cases (9.52%) with chronic ocular discomfort that was controlled by topical lubricants and NSAIDS.
Persistent postoperative diplopia following SB has a reported incidence of 3%-14% in retrospective studies[35]. In the current study, only one case (4.76%) developed postoperative diplopia which was managed by prism use. Older reports describing higher rates of extraocular muscle imbalance problems were mainly related to hydrogel material in old buckles which are no longer used. SB also induces myopic shift which tends to diminish by time until it stabilizes after 3mo. A final postoperative refractive myopic shift of 1.49 D was observed in our study. Similar results were detected in a randomized study comparing SB with PPV as the mean refractive change was 1.38 D following SB compared to 0.85 D following PPV[36].The significant refractive change in our study could be explained by two observations. First, combined encircling band with tire or sponge was used in (61.90%) of cases, and when additional buckle is used the myopic shift increases[37].Second, scleral buckle was placed extremely peripheral in several cases to address the anteriorly located retinal tears, and when a buckle position is closer to the cornea, the refractive change increases also[38].
However, this negative refractive effect of SB could be weighed against the potential advantages of SB over vitrectomy in pseudophakic eyes such as the lower incidence of iatrogenic breaks, postoperative IOP elevation[16], endothelial cell loss[17]and aggressive PVR formation in case of primary failure[18].SB also obviates complications like IOL displacement or air condensation and eliminates the need for vitreous substitutes or postoperative positioning. SB perfectly supports anterior retinal breaks and is also equally effective for both superior and inferior breaks.
CDVA of 6/12 or better following vitrectomy alone for pseudophakic RD was achieved in 44% to 72% of cases according to different studies[24]. In the current study,28.6% and 47.6% had postoperative CDVA of 6/12 and 6/18 respectively. Macula-on detachments were associated with better postoperative CDVA. Functional outcome was affected by the relatively high percentage of macula-involving detachments (76.2%). It is also important to note that data prior to cataract surgery including refraction were incomplete,hence incidence of myopia was not reported. The only objective method to isolate myopic eyes would have been B-scan ultrasound which was not part of management plan.However, we encountered several cases with myopic fundus appearance, myopic refraction of a fellow phakic eye or history of RD in the other eye. We called these cases “presumed myopic eyes” which might have contributed to the suboptimal functional outcome because high myopia can jeopardize visual recovery[39].
Although chandelier insertion converted SB from an extraocular to intraocular procedure, no case of IOL displacement,iatrogenic break, retinal incarceration or endophthalmitis was detected. This finding is consistent with most of other reports on chandelier assisted SB, except one study reporting one case of iatrogenic break[10] and a single case report of acute bacterial endophthalmitis[40]. To minimize vitreous prolapse through the chandelier sclerotomy, a valved cannula was used and the IOP was lowered by paracentesis or subretinal fluid drainage before trocar cannula removal. If vitreous prolapse occurred,it was cut by a scissor. Sclerotomy incision was sutured in all cases. It is worth mentioning that the classic description of SB as an extraocular procedure is mostly theoretical because it is not uncommon to perform anterior chamber paracentesis,subretinal fluid drainage or air injection in several cases. In the current study, external drainage of subretinal fluid was done in case of highly elevated detachments preventing cryotherapy to retinal breaks or high IOP resulting from high scleral indentation by buckling, in spite of paracentesis.
The use of chandelier definitely increases the cost of the procedure but this is largely out weighted by the privileged illumination obtained by this method. Another benefit of using chandelier in pseudophakics was the ability to place it 180 degrees away from retinal breaks. It was even possible to slightly tilt the chandelier to direct the illumination towards a desired location without the fear of injuring a crystalline or the need to change chandelier site.
To our knowledge, this is the first report of chandelier assisted SB in pseudophakic RD using WAV contact lens. In conclusion, the current study supports the use of this technique for management of selected cases of simple pseudophakic RD.The technique was reliable with a relatively high success rate and an acceptable rate of complications. Further studies may confirm our findings.
ACKNOWLEDGEMENTS
Conflicts of Interest: NossairAA, None; Ewais WA, None;Eissa SA, None.
1 Mahroo OA, Dybowski R, Wong R, Williamson TH. Characteristics of rhegmatogenous retinal detachment in pseudophakic and phakic eyes. Eye(Lond) 2012;26(8):1114-1121.
2 Narayanan R, Tyagi M, Hussein A, Chhablani J, Apte RS. Scleral buckling with wide-angled endoillumination as a surgical educational tool. Retina 2016;36(4):830-833.
3 Chen SN, Lian IeB, Wei YJ. Epidemiology and clinical characteristics of rhegmatogenous retinal detachment in Taiwan. Br J Ophthalmol 2016;100(9):1216-1220.
4 Lois N, Wong D. Pseudophakic retinal detachment. Surv Ophthalmol 2003;48(5):467-487.
5 Ross WH, Lavina A. Pneumatic retinopexy, scleral buckling,and vitrectomy surgery in the management of pseudophakic retinal detachments. Can J Ophthalmol 2008;43(1):65-72.
6 Seider MI, Nomides RE, Hahn P, Mruthyunjaya P, Mahmoud TH.Scleral buckling with chandelier illumination. J Ophthalmic Vis Res 2016;11(3):304-309.
7 Ho CL, Chen KJ, See LC. Selection of scleral buckling for primary retinal detachment. Ophthalmologica 2002;216(1):33-39.
8 Aras C, Ucar D, Koytak A, Yetik H. Scleral buckling with a non-contact wide-angle viewing system. Ophthalmologica 2012;227(2):107-110.
9 Gogia V, Venkatesh P, Gupta S, Kakkar A, Garg S. Endoilluminatorassisted scleral buckling: our results. Indian J Ophthalmol 2014;62(8):893-894.
10 Imai H, Tagami M, Azumi A. Scleral buckling for primary rhegmatogenous retinal detachment using noncontact wide-angle viewing system with a cannula-based 25 G chandelier endoilluminator. Clin Ophthalmol 2015;9:2103-2107.
11 Hu YT, Si SC, Xu K, Chen HJ, Han L, Wang X, Ma ZZ. Outcomes of scleral buckling using chandelier endoillumination. Acta Ophthalmol 2017;95(6):591-594.
12 Nam KY, Kim WJ, Jo YJ, Kim JY. Scleral buckling technique using a 25-gauge chandelier endoilluminator. Retina 2013;33(4):880-882.
13 Nagpal M, Bhardwaj S, Mehrotra N. Scleral buckling for rhegmatogenous retinal detachment using vitrectomy-based visualization systems and chandelier illumination. Asia Pac J Ophthalmol (Phila)2013;2(3):165-168.
14 Lincoff H, Kreissig I. Finding the retinal hole in the pseudophakic eye with detachment. Am J Ophthalmol 1994;117(4):442-446.
15 Machemer R, Aaberg TM, Freeman HM, Irvine AR, Lean JS, Michels RM. An updated classification of retinal detachment with proliferative vitreoretinopathy. Am J Ophthalmol 1991;112(2):159-165.
16 Toyokawa N, Kimura H, Matsumura M, Kuroda S. Incidence of lateonset ocular hypertension following uncomplicated pars plana vitrectomy in pseudophakic eyes. Am J Ophthalmol 2015;159(4):727-732.
17 Cinar E, Zengin MO, Kucukerdonmez C. Evaluation of corneal endothelial cell damage after vitreoretinal surgery: comparison of different endotamponades. Eye (Lond) 2015;29(5):670-674.
18 Ricker LJ, Kessels AG, de Jager W, Hendrikse F, Kijlstra A, la Heij EC. Prediction of proliferative vitreoretinopathy after retinal detachment surgery: potential of biomarker profiling. Am J Ophthalmol 2012;154(2):347-354.e2.
19 Christoforidis JB, Williams MM, Wang J, Jiang A, Pratt C, Abdel-Rasoul M, Hinkle GH, Knopp MV. Anatomic and pharmacokinetic properties of intravitreal bevacizumab and ranibizumab after vitrectomy and lensectomy. Retina 2013;33(5):946-952.
20 Oshima Y. Choices of wide-angle viewing systems for modern vitreoretinal surgery: a semi-quantitative evaluation of the visual angle field and imaging contrast. Retin Today 2012;5:37-42.
21 Newsom RS, Wainwright AC, Canning CR. Local anaesthesia for 1221 vitreoretinal procedures. Br J Ophthalmol 2001;85(2):225-227.
22 Calenda E, Olle P, Muraine M, Brasseur G. Peribulbar anesthesia and sub-Tenon injection for vitreoretinal surgery: 300 cases. Acta Ophthalmol Scand 2000;78(2):196-199.
23 Mehta S, Hubbard GB 3rd. Avoiding neck strain in vitreoretinal surgery: an ergonomic approach to indirect ophthalmoscopy and laser photocoagulation. Retina 2013;33(2):439-441.
24 Cankurtaran V, Citirik M, Simsek M, Tekin K, Teke MY. Anatomical and functional outcomes of scleral buckling versus primary vitrectomy in pseudophakic retinal detachment. Bosn J Basic Med Sci 2017;17(1):74-80.25 Pournaras CJ, Kapetanios AD. Primary vitrectomy for pseudophakic retinal detachment: a prospective non-randomized study. Eur J Ophthalmol 2003;13(3):298-306.
26 Brazitikos PD, Androudi S, Christen WG, Stangos NT. Primary pars plana vitrectomy versus scleral buckle surgery for the treatment of pseudophakic retinal detachment: a randomized clinical trial. Retina 2005;25(8):957-964.
27 Sun Q, Sun T, Xu Y, Yang XL, Xu X, Wang BS, Nishimura T,Heimann H. Primary vitrectomy versus scleral buckling for the treatment of rhegmatogenous retinal detachment: a meta-analysis of randomized controlled clinical trials. Curr Eye Res 2012;37(6):492-499.
28 Soni C, Hainsworth DP, Almony A. Surgical management of rhegmatogenous retinal detachment: a meta-analysis of randomized controlled trials. Ophthalmology 2013;120(7):1440-1447.
29 Moradian S, Ahmadieh H, Faghihi H, Ramezani A, Entezari M,Banaee T, Heidari E, Behboudi H, Yasseri M. Comparison of four surgical techniques for management of pseudophakic and aphakic retinal detachment: a multicenter clinical trial. Graefes Arch Clin Exp Ophthalmol 2016;254(9):1743-1751.
30 Walter P, Hellmich M, Baumgarten S, Schiller P, Limburg E,Agostini H, Pielen A, Helbig H, Lommatzsch A, Rössler G, Mazinani B,VIPER Study Group. Vitrectomy with and without encircling band for pseudophakic retinal detachment: VIPER Study Report No 2-main results.Br J Ophthalmol 2017;101(6):712-718.
31 Kessner R, Barak A. Pseudophakic rhegmatogenous retinal detachment:combined pars plana vitrectomy and scleral buckle versus pars plana vitrectomy alone. Graefes Arch Clin Exp Ophthalmol 2016;254(11):2183-2189.
32 Haritoglou C, Brandlhuber U, Kampik A, Priglinger SG. Anatomic success of scleral buckling for rhegmatogenous retinal detachment: a retrospective study of 524 cases. Ophthalmologica 2010;224(5):312-318.
33 Adelman RA, Parnes AJ, Michalewska Z, Ducournau D, European Vitreo-Retinal Society (EVRS) Retinal Detachment Study Group.Clinical variables associated with failure of retinal detachment repair: the European vitreo-retinal society retinal detachment study report number 4.Ophthalmology 2014;121(9):1715-1719.
34 Massicotte E, Hammamji K, Landry T, Häuser W, Fitzcharles MA.Postoperative pain management in vitreoretinal surgery for retinal detachment: a systematic review of randomized controlled trials. Journal of VitreoRetinal Diseases 2018;2(3):160-175.
35 Kasbekar SA, Wong V, Young J, Stappler T, Durnian JM.Strabismus following retinal detachment repair: a comparison between scleral buckling and vitrectomy procedures. Eye (Lond) 2011;25(9):1202-1206.
36 Sharma YR, Karunanithi S, Azad RV, Vohra R, Pal N, Singh DV,Chandra P. Functional and anatomic outcome of scleral buckling versus primary vitrectomy in pseudophakic retinal detachment. Acta Ophthalmol Scand 2005;83(3):293-297.
37 Nassaralla Junior JJ, do Amaral Nassaralla BR. Refractive changes after scleral buckling surgery. Arq Bras Oftalmol 2003;66(5):575-578.
38 Okada Y, Nakamura S, Kubo E, Oishi N, Takahashi Y, Akagi Y.Analysis of changes in corneal shape and refraction following scleral buckling surgery. Jpn J Ophthalmol 2000;44(2):132-138.
39 Salicone A, Smiddy WE, Venkatraman A, Feuer W. Visual recovery after scleral buckling procedure for retinal detachment. Ophthalmology 2006;113(10):1734-1742.
40 Sakono T, Otsuka H, Shiihara H, Yoshihara N, Sakamoto T. Acute bacterial endophthalmitis after scleral buckling surgery with chandelier endoillumination. Am J Ophthalmol Case Rep 2017;8:7-10.