INTRODUCTION
T oday, femtosecond laser (FSL) assisted laser in situ keratomileusis (LASIK) has been worldwide accepted as a popular treatment for refractive errors. The security,effectiveness, stability, and predictability of LASIK have been extensively validated[1-2]. Compared with the microkeratome,the creation of flap with FSL is more predictable[3]. But there are some specific FSL related complications, particularly some gas-related complications[4-5]. The opaque bubble layer(OBL), as a frequent one, can interfere with eye tracking of excimer laser machine. Some scholars render that OBL may lead to trifolium-like aberration and can make the sensitivity of visual contrast decrease in the early postoperative stage[6-7]. In small incision lenticule extraction (SMILE), there is a higher incidence of flap tear in eyes with extensive OBL [8]. The reduction of the OBL is one of the key points that FSL assisted refractive surgery needs to improve. The FS200 FSL machine especially designs a gas diffusing canal at the hinge of the corneal flap. Without considering the related factors that can generate gas, improving the patency of the gas diffusing canal can reduce the incidence of OBL.
As reported in literature, the 1.7 mm width canal reduced the incidence of OBL compared with the 1.3 mm width design[9].The oval-shaped flap with a larger hinge angle tended to result in lower OBL incidence[10]. The cone modification technique was also related to lower risk of OBL formation[11]. However,these studies had not excluded some confounding factors such as corneal hysteresis, viscosity, etc.
In clinical work, we find that the occurrence of OBL of FS200 FSL is closely related to the patency of gas diffusing canal, and the patency of gas diffusing canal is also closely related to its outlet location. The training specialist of FS200 FSL machine instructed that the outlet of gas diffusing canal must be located at 0.1 mm outside of the watermark between cornea and applanation cone. But we found that the location of watermark varied in great range because of different tightness between cornea and applanation cone. We also found that the incidence of OBL during laser assisted laser in situ keratomileusis (FSLASIK) was very low when the outlet of gas diffusing canal was located at the posterior border of the corneoscleral limbus.So, we use case (eye) control method to analyze the cause of OBL between the two fellow eyes of one patient.
In the study, we analyzed the data of FS-LASIK cases with unilateral OBL from January to June of 2017. The study compared the data between the OBL eyes and the fellow eyes of the same cases excluding the confounding factors such as corneal hysteresis, viscosity, etc.
SUBJECTS AND METHODS
Ethical Approval The study complied with the principles of the Declaration of Helsinki. All patients were informed of the refractive surgery risk and signed informed consent preoperatively.
Subjects The study consisted of 60 consecutive patients with unilateral OBL when they underwent FS-LASIK. Eyes were divided into OBL (the OBL eyes) and OBL-free groups (the fellow eyes) based on the occurrence of OBL. The OBL group included 27 right eyes (the first eyes) and 33 left eyes (the second eyes). The data of the two groups was in Table 1 in details.
Inclusion and Exclusion Criteria Inclusion criteria: above 18y of age; preoperative myopia had remained stable for more than 2y (the increase of myopia sphere equivalent per year was less than 0.5 diopter); stopped wearing contact lens for at least 3wk before surgery. The additional inclusion criteria:The central thickness difference between fellow eyes of one patient was less than 20 µm; the central curvature difference between fellow eyes of one patient was less than 1 diopter;the difference of intraocular pressure between fellow eyes of one patient was less than 5 mm Hg. The standard of exclusion was contraindication of laser refractive surgery: active eye diseases such as keratitis, cataracts, glaucoma, etc; suspected keratoconus or keratoconus indicated by the anterior segment analysis system (Oculyzer, Alcon Laboratories, Inc., Fort Worth, TX, USA). The excimer laser ablation of the eyes with retinal breaks, holes, or lattice degeneration was performed after 2wk of the photocoagulation of the lesions.
The presence of OBL and the location of outlet of gas diffusing canal had been evaluated according to the observation by the surgeon and the images preserved after the FSL emission.
Table 1 Data of the two groups

D: Diopter; SE: Spherical equivalent; IOP: Intraocular pressure; K:Keratometry; CCT: Central cornea thickness; OBL: Opaque bubble layer.
Items OBL eyes Eyes without OBL P SE (D) -5.05±1.92 -5.01±1.82 0.92 IOP (mm Hg) 15.91±3.15 16.04±2.98 0.81 Steep K (D) 43.42±1.27 43.48±1.36 0.80 Flat K (D) 42.21±1.17 42.12±1.21 0.69 CCT (µm) 554.50±25.24 553.80±24.62 0.88
Table 2 Predefined parameters of flap creation with femtosecond laser
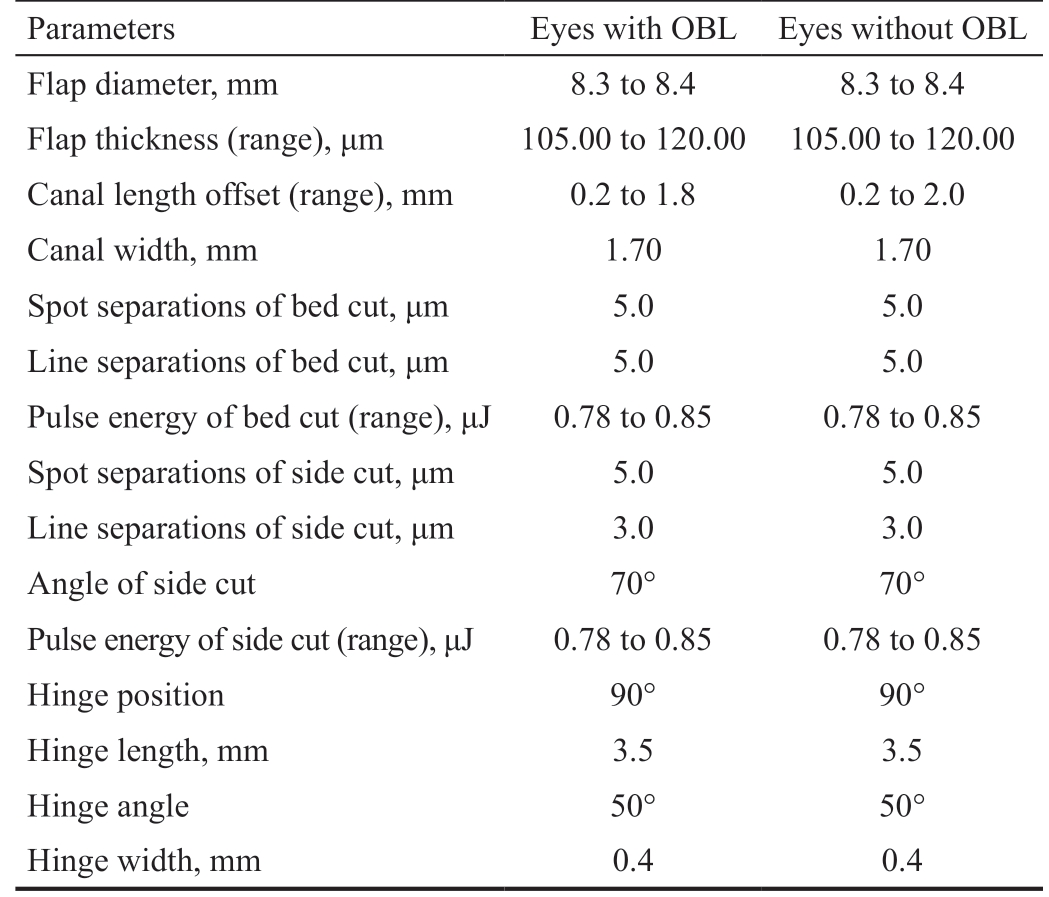
OBL: Opaque bubble layer.
Parameters Eyes with OBL Eyes without OBL Flap diameter, mm 8.3 to 8.4 8.3 to 8.4 Flap thickness (range), μm 105.00 to 120.00 105.00 to 120.00 Canal length offset (range), mm 0.2 to 1.8 0.2 to 2.0 Canal width, mm 1.70 1.70 Spot separations of bed cut, μm 5.0 5.0 Line separations of bed cut, μm 5.0 5.0 Pulse energy of bed cut (range), μJ 0.78 to 0.85 0.78 to 0.85 Spot separations of side cut, μm 5.0 5.0 Line separations of side cut, μm 3.0 3.0 Angle of side cut 70° 70°Pulse energy of side cut (range), μJ 0.78 to 0.85 0.78 to 0.85 Hinge position 90° 90°Hinge length, mm 3.5 3.5 Hinge angle 50° 50°Hinge width, mm 0.4 0.4
The examination before surgery included routine examination of eyeball, uncorrected vision acuity, corrected vision acuity,IOP, optometry, refraction, oculyzer and OPD scan II (NIDEK Co., Ltd. Aichi, Japan), etc.
Operation Process Surface anesthesia was performed using Oxybuprocaine Hydrochloride Eye Drops (Santen Pharmaceutical Co., Ltd, Osaka, Japan) and applied 2 times at the interval of 5min before surgery. After the eyelid was opened, a suction ring was placed on the surface of the eyeball when the cornea was moist. After the vacuum 1st was formed completely, the applanation cone was fitted to the suction ring.After the vacuum 2nd was formed completely, the surgeon set outlet location of gas diffusing canal according to the presetting regimes. Then the surgeon switched on the FS-200 femtosecond machine (Alcon Laboratories, Inc., Fort Worth, TX, USA ) to emit FSL pulses for about 7s. After FSL emission, the negative pressure released automatically and the flap images were preserved. The parameters during the creation of the flap were listed in Table 2 in details.
All patients' excimer laser ablations were performed using EC-5000 excimer laser machine (NIDEK Co., Ltd. Aichi,Japan) immediately after corneal flap creation. Postoperative regime: the patients were prescribed levofloxacin eye drops(Santen Pharmaceutical Co., Ltd, Osaka, Japan) 4 times daily for 1wk and fluorometholone eye drops (Santen Pharmaceutical Co., Ltd, Osaka, Japan) 4 times daily tapered for 4wk.
The patients revisited at the 1st day, the 1st, 2nd, 4th weeks and 2nd, 6th months after surgery for the measurement of visual acuity, intraocular pressure, refraction and high order aberration (OPD scan II).
The Definition of Opaque Bubble Layer and the Location of Outlet The incidence of OBL and the outlet location of gas diffusing canal were analyzed according to the surgeon's observation and preserved images. The hard type OBL showed denser, concentrated and bigger area, while the soft one was mild, dispersed and smaller.
Statistical Analysis The data were analyzed with paired case control method of clinical epidemiology. The OBL eyes were considered as case group while the fellow eyes were considered as paired control group. The statistical analysis between the 2 groups used SPSS19.0 software (International Business Machines Corporation, Armonk, New York, United States) by the conditional logistic regression analysis method.Continuous variables were expressed as means±standard deviations after confirming normality and homogeneity of the data distribution. The parameters were compared between OBL-affected eyes and fellow eyes using t-test. Otherwise,the nonparametric test method was used. Univariate and multivariate conditional logistic regression analyses[12] were performed to find predictive factors associated with OBL.Variables with P value less than 0.2 in the univariate regression outcome were incorporated in the multivariate regression analysis to obtain the final results. P value less than 0.05 was considered significant.
RESULTS
All patients' surgeries were completed without unusual events.The results of univariate and multivariate logistic regression analysis of parameter for prediction of OBL were showed in Table 3 in details.
The outlet location of gas diffusing canal [P<0.01, odds ratios(OR) 7.16, 95%CI 2.53-20.32] and the corneal astigmatism degree (P=0.013, OR 0.13, 95%CI 0.03-0.65) were significantly associated with the occurrence of OBL by multivariate logistic regression analysis.
The preoperative corneal astigmatism of 60 eyes in OBL group was 1.21+0.65, and the axial was 92.77+19.01. Among them, 5 eyes were against-the-rule astigmatism or oblique astigmatism and each of their degrees was no more than 0.5 D. The rest eyes were all with-the-rule astigmatism. The corneal astigmatism degree in OBL-free group was 1.36±0.73, and the axial was 88.72±16.00. Among them, 3 eyes were against-the-rule astigmatism or oblique astigmatism and each of their degrees was 0.5 D. The rest eyes were all with-the-rule astigmatism.

Figure 1 Different outlet locations of gas diffusing canal in the OBL eyes and the fellow eyes P<0.01.
Table 3 Results of univariate and multivariate logistic regression analysis of parameter for prediction of OBL
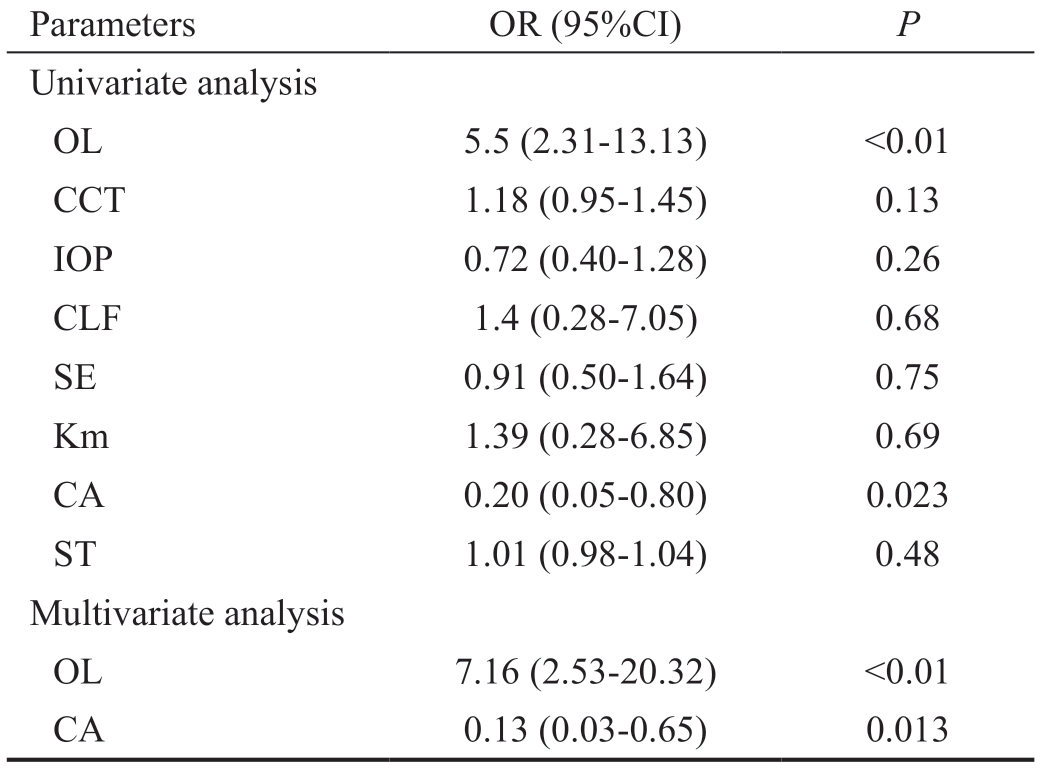
OL: Outlet location of gas diffusing canal; CCT: Central cornea thickness;IOP: Intraocular pressure; CLF: Canal length offset; SE: Spherical equivalent; Km: Mean keratometry; CA: Corneal astigmatism; ST:Suction time; OR: Odds ratios.
Parameters OR (95%CI) P Univariate analysis OL 5.5 (2.31-13.13) <0.01 CCT 1.18 (0.95-1.45) 0.13 IOP 0.72 (0.40-1.28) 0.26 CLF 1.4 (0.28-7.05) 0.68 SE 0.91 (0.50-1.64) 0.75 Km 1.39 (0.28-6.85) 0.69 CA 0.20 (0.05-0.80) 0.023 ST 1.01 (0.98-1.04) 0.48 Multivariate analysis OL 7.16 (2.53-20.32) <0.01 CA 0.13 (0.03-0.65) 0.013
The degree of astigmatism in the OBL group was less than that of OBL-free group, but the difference of the mean degree between two groups was not statistically significant (P>0.05).In OBL-affected eyes, only 15 of 60 eyes' outlet locations of gas diffusing canal were located at the posterior border of corneoscleral limbus while there were as many as 42 of 60 eyes' in the fellow eyes (Figure 1).
In 33 eyes of hard OBL, the 6 (18.18%), 5 (15.15%) and 22 (66.67%) of canal outlets located at the cornea, posterior border of the corneoscleral limbus or the sclera respectively. In 27 eyes of soft OBL, the 2 (7.40%), 10 (37.03%) and 15 (55.56%)of canal outlets located at the cornea, posterior border of the corneoscleral limbus or sclera respectively. Hard OBL was easy to occur when the canal outlet located at the cornea.When the canal outlet located at the posterior border of the corneoscleral limbus, slight soft OBL was more common.
The refraction, uncorrected visual acuity and high order aberration between 2 groups 2mo postoperatively were illustrated in Table 4 in detail. No parameter reached a statistically significant difference between the OBL eyes and the fellow eyes (P>0.05).
Table 5 compared the parameters between the hard OBL eyes and the soft OBL eyes.
Table 4 The refraction, uncorrected visual acuity and high order aberration between the 2 groups 2mo postoperatively
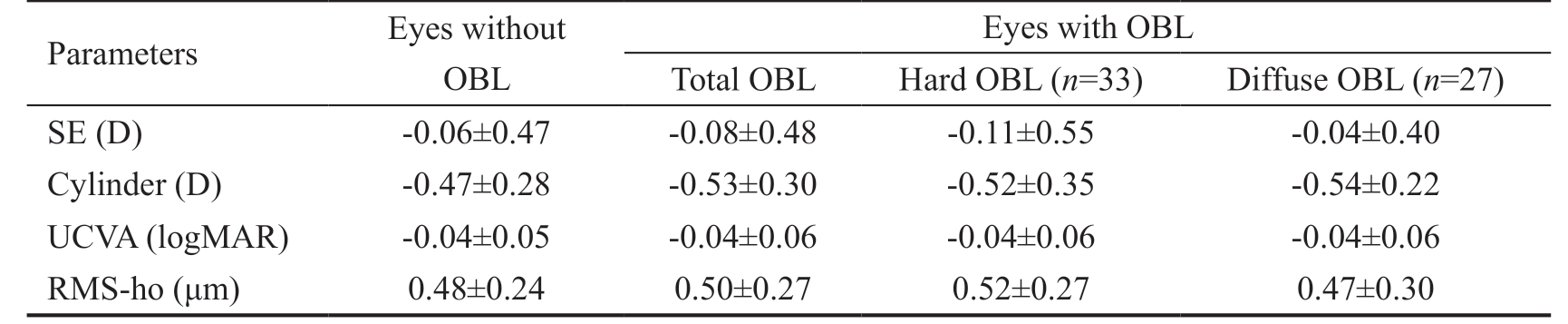
D: Diopter; SE: Spherical equivalent; UCVA: Uncorrected visual acuity; RMS-ho: Root mean square of high order aberration; OBL: Opaque bubble layer.
Parameters Eyes without OBL Eyes with OBL Total OBL Hard OBL (n=33) Diffuse OBL (n=27)SE (D) -0.06±0.47 -0.08±0.48 -0.11±0.55 -0.04±0.40 Cylinder (D) -0.47±0.28 -0.53±0.30 -0.52±0.35 -0.54±0.22 UCVA (logMAR) -0.04±0.05 -0.04±0.06 -0.04±0.06 -0.04±0.06 RMS-ho (μm) 0.48±0.24 0.50±0.27 0.52±0.27 0.47±0.30
DISCUSSION
OBL can occur in different kind of FSL machines. There are many factors such as characteristics of different FSL machines,parameters of laser energy, flap diameter[13], patients' central cornea thickness, corneal viscosity, hysteresis and curvature value that are related to OBL[14-16].
Aside from relevant factors that can generate OBL gas in FSL emission, it should be the key point to allow the generated gas to diffuse outside of stroma. LDV (Ziemer Ophthalmic Systems, Port, Switzerland), IntraLase (Abbott Medical Optics Inc, Santa Ana, CA, USA), Visumax (Carl Zeiss Meditec AG,Jena, Germany) and Wavelight FS200 (Alcon Laboratories,Inc, Fort Worth, TX, USA) FSL machines have already taken special methods to drain the gas that could lead to OBL. The gas produced by micro disrupture of FSL of LDV will overflow soon through the incision edge because of the model of first cutting of flap margin. However, due to the scanning mode of LDV, it is very difficult to dispose the complication of suction loss. The IntraLace machine makes a bag that could store gas to reduce the incidence of OBL. The Zeiss machine scans in the pattern from the corneal periphery to the center, allowing the gas to diffuse through the margin of cornea. The FS200 machine create a canal in the hinge of flap as the gas diffusing passage to reduce the incidence of OBL. Therefore, apart from the relevant factors generating gas, it is very important to allowthe OBL-related gas to diffuse smoothly. It is very important for the FS200 FSL machine to keep the canal open.
Table 5 Preoperative and intraoperative parameters of the eyes with hard OBL or soft OBL

SE: Spherical equivalent; IOP: Intraocular pressure; CCT: Central cornea thickness; OBL: Opaque bubble layer.
Parameters Soft OBL (n=27) Hard OBL (n=33) P Preoperative Mean age (y) 20.30±3.03 21.11±4.24 0.39 Female sex, n (%) 10 (30.3) 7 (25.9) 0.18 Mean SE (D) -5.06±1.94 -5.04±1.93 0.98 Mean steep K (D) 43.32±1.26 43.54±1.29 0.51 Mean flat K (D) 42.11±1.18 42.33±1.17 0.46 Mean IOP (mm Hg) 16.21±3.19 15.54±3.12 0.60 Mean CCT (μm) 554.67±22.55 554.30±28.63 0.96 Intraoperative Mean flap thickness (μm) 109.24±4.35 107.96±3.47 0.22 Mean canal length offset (mm) 0.69±0.29 0.70±0.35 0.91 Mean suction time (s) 41.94±10.90 47.04±24.15 0.32
The diopter, corneal curvature value, corneal thickness,viscosity and hysteresis of the same patient were comparative.The predesigned parameters of the corneal flap were also the same. However, we found that most of OBL occurred in only unilateral eye of one patient. The main difference between the fellow eyes of one patient is the presetting canal length offset value. We also found that the gas diffusing canal either too long or too short will affect its patency. Thereby designing an unobstructed canal is a key point to circumvent OBL as far as FS200 FSL machine is concerned. The training specialist of FS200 FSL machine instructed us to locate the outlet at 0.1 mm outside of the watermark between the cornea and applanation cone. However, the incidence of OBL was high as instructed by the training specialist. Moreover, we found that the location of watermark varied in a great range because of different tightness between cornea and applanation cone. So it's helpful to find a constant indication to set the canal length offset.
The corneoscleral limbus was translucent. So, the FSL can penetrate it and the gas diffusing canal kept unobstructed.When the outlet was located at the posterior border of the corneoscleral limbus, the incidence of OBL was significantly low (Figure 2).
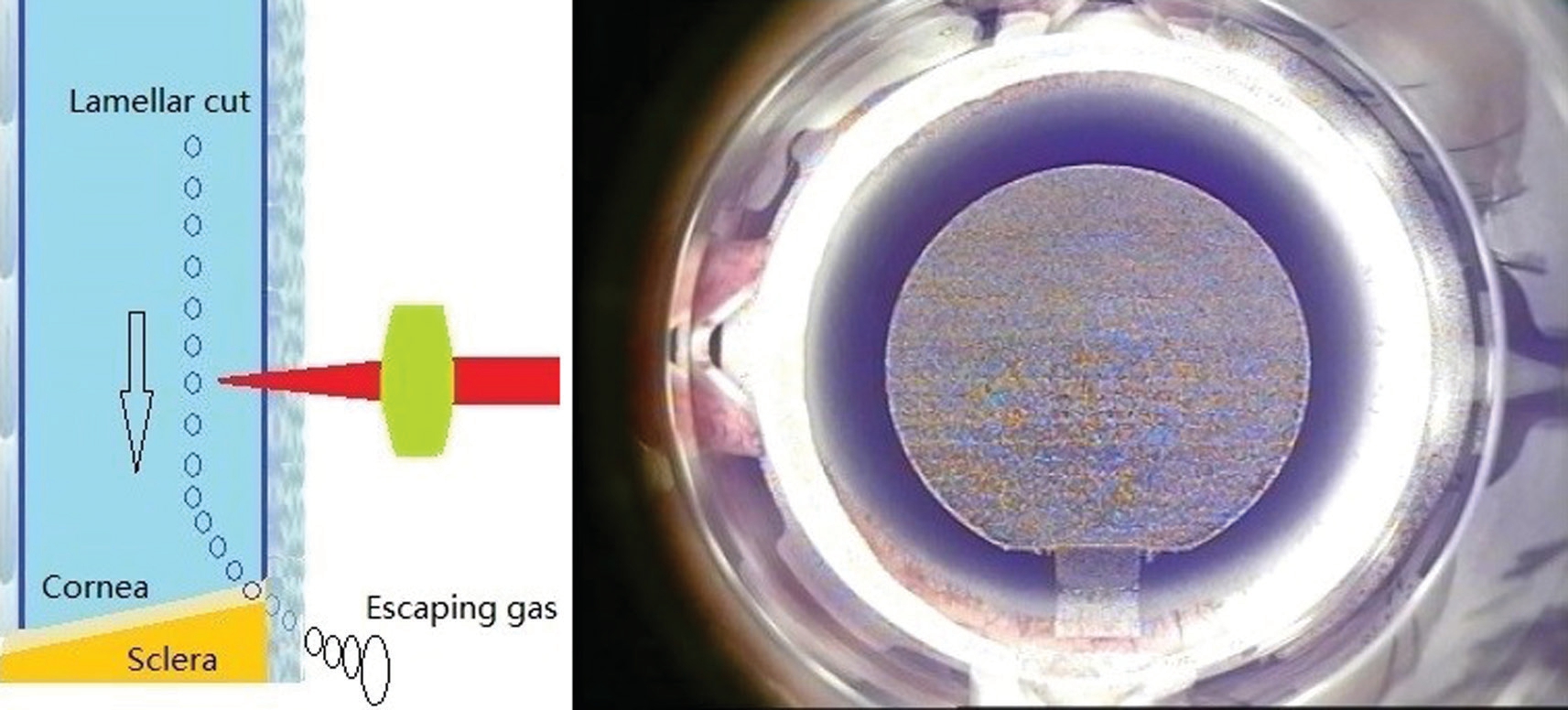
Figure 2 The outlet of gas diffusing canal located at the posterior border of the corneoscleral limbus: OBL didn’t occur.
The corneal curvature was steeper than the curvature of sclera.When the outlet was located at cornea, the canal undertook more large pressure and had lower probability of patency(Figure 3). Moreover, gas bubble breakthrough was easy to happen in these cases.
The FSL cannot penetrate the sclera due to its opaque characteristic.When the gas diffusing canal outlet was located at sclera, the outlet of gas diffusing canal did not open and the canal could not communicate with the atmosphere. Thus, the gas could not diffuse and led to OBL (Figure 4).
There is a fine balance between the proper location of the outlet as mentioned before. A fine venting outlet is unobstructed but not very fast. Because quick venting of gas can also lead to some detrimental impacts such as chattering and linear irregularity in the flap and the stromal bed.
In the study we also found that the degree of corneal astigmatism was negatively related to the incidence of OBL.Li et al[17] thought that the increase of ocular astigmatism could reduce the occurrence of OBL. We thought that the ocular astigmatism did not necessarily coincide with corneal astigmatism. So we regressively analyzed the incidence of OBL with corneal astigmatism. Univariate and multivariate regressions showed that the incidence of OBL decreased with the increase of corneal astigmatism degree, which was similar to that of Li et al[17].
Despite the difference of the mean astigmatism degree between two groups was not statistically significant, the corneal astigmatism degree of OBL-free group was greater than that of OBL group. The cornea with large astigmatism was difficult to be flattened, so the gas between the cornea flap and stroma bed could easily diffuse and did not lead to OBL.Most of the corneal astigmatisms in the two groups were withthe-rule astigmatisms, and the degrees of against-the-rule or oblique astigmatism in both groups were slight. Therefore, we speculate that the difference of OBL incidence between the two groups had little to do with the astigmatism axis.
The locations of canal outlet were also related to the types of OBL. When the canal outlet was located at cornea, because the canal was short, the gas produced by FSL cutting had no diffusion space. The gas accumulated in the corneal stromal bed and led to hard OBL. When the canal outlet was located at the sclera, despite was impassable, the canal could accommodate partial gas and slight soft OBL occurred. When the canal outlet was located at the posterior border of the corneoscleral limbus, soft OBL was more common because some canal were partial unobstructed and could diffuse some gas.At present, the published literature preliminarily considers that OBL doesn't influence the excimer laser ablation effect or postoperative uncorrected and corrected visual acuity[14]. But severe hard OBL can disturb eye tracking of excimer laser. Our results showed that the refractive status of the OBL eyes 2mo after surgery was more inclined to be negative, but it didn't reach statistical difference.
In summary, keeping the gas diffusing canal unobstructed is one of the key points to decrease the incidence of OBL in FS-LASIK using FS200 FSL machine. When the outlet of gas diffusing canal was located at the posterior border of the corneoscleral limbus, the high patency rate could be obtained,thus the incidence of OBL was low. Corneal astigmatism was also a independent protective factor for OBL formation.However OBL is the result of many factors, so reducing the incidence of OBL needs the development in the technological and clinical fields.
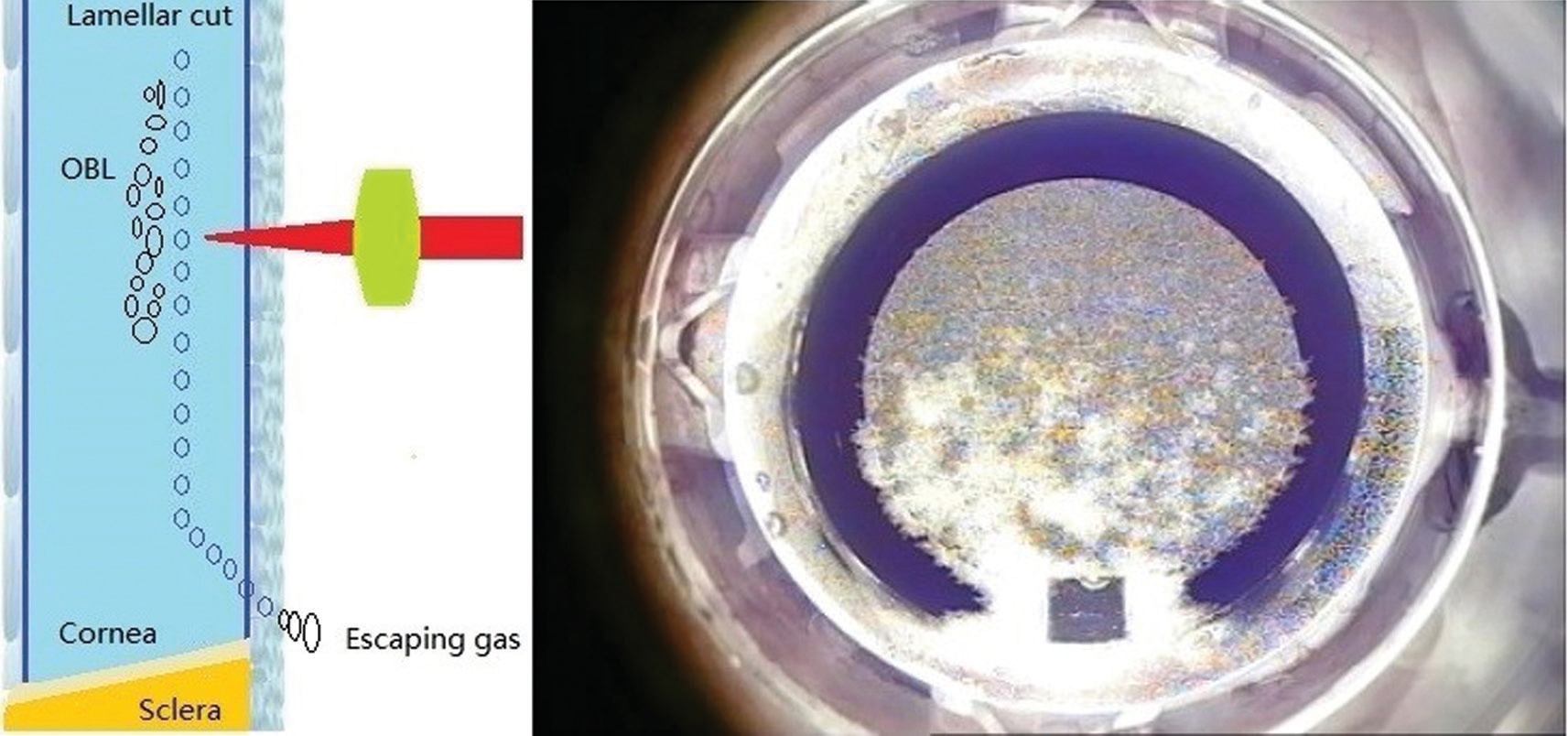
Figure 3 The outlet of gas diffusing canal located at cornea: OBL occurred.

Figure 4 The outlet of gas diffusing canal located at sclera: OBL occurred.
ACKNOWLEDGEMENTS
Foundations: Supported by the National Natural Science Fund of China in 2017 (No.81700867); the Wannan Medical College Training Fund Project of Key Scientific Research Project in 2017 (No.WK2017ZF05).
Conflicts of Interest: Wei CH, None; Dai QY, None; Mei LX, None; Ge Y, None; Zhang PF, None; Song E, None.
1 Slade S, Ignacio T, Spector S. Evaluation of a multifunctional femtosecond laser for the creation of laser in situ keratomileusis flaps. J Cataract Refract Surg 2018;44(3):280-286.
2 Hashmani S, Hashmani N, Rajani H, Ramesh P, Soomro JA,Hussain Shah SR, Kumar J, Mahmood Shah SM. Comparison of visual acuity, refractive outcomes, and satisfaction between LASIK performed with a microkeratome and a femto laser. Clin Ophthalmol 2017;11:1009-1014.
3 Xia LK, Yu J, Chai GR, Wang D, Li Y. Comparison of the femtosecond laser and mechanical microkeratome for flap cutting in LASIK. Int J Ophthalmol 2015;8(4):784-790.
4 Farjo AA, Sugar A, Schallhorn SC, Majmudar PA, Tanzer DJ,Trattler WB, Cason JB, Donaldson KE, Kymionis GD. Femtosecond lasers for LASIK flap creation: a report by the American Academy of Ophthalmology. Ophthalmology 2013;120(3):e5-e20.
5 Robert MC, Khreim N, Todani A, Melki SA. Anterior chamber gas bubble emergence pattern during femtosecond LASIK-flap creation. Br J Ophthalmol 2015;99(9):1201-1205.
6 Liu CH, Sun CC, Hui-Kang Ma D, Chien-Chieh Huang J, Liu CF, Chen HF, Hsiao CH. Opaque bubble layer: incidence, risk factors, and clinical relevance. J Cataract Refract Surg 2014;40(3):435-440.
7 Kaiserman I, Maresky HS, Bahar I, Rootman DS. Incidence, possible risk factors, and potential effects of an opaque bubble layer created by a femtosecond laser. J Cataract Refract Surg 2008;34(3):417-423.
8 Son G, Lee J, Jang C, Choi KY, Cho BJ, Lim TH. Possible risk factors and clinical effects of opaque bubble layer in small incision lenticule extraction (SMILE). J Refract Surg 2017;33(1):24-29.
9 Kanellopoulos AJ, Asimellis G. Essential opaque bubble layer elimination with novel LASIK flap settings in the FS200 Femtosecond Laser. Clin Ophthalmol 2013;7:765-770.
10 Lin HY, Fang YT, Chuang YJ, Yu HC, Pu C, Chou YJ, Chien CY,Lin PJ, Schallhorn SC, Sun CC. Influences of flap shape and hinge angle on opaque bubble layer formation in femtosecond laser-assisted LASIK surgery. J Refract Surg 2017;33(3):178-182.
11 Wu NL, Christenbury JG, Dishler JG, Bozkurt TK, Duel D, Zhang LJ,Hamilton DR. A technique to reduce incidence of opaque bubble layer formation during LASIK flap creation using the VisuMax femtosecond laser. J Refract Surg 2017;33(9):584-590.
12 Lee JR, Sung KR, Han S. Comparison of anterior segment parameters between the acute primary angle closure eye and the fellow eye. Invest Ophthalmol Vis Sci 2014;55(6):3646-3650.
13 Mastropasqua L, Calienno R, Lanzini M, Salgari N, De Vecchi S, Mastropasqua R, Nubile M. Opaque bubble layer incidence in Femtosecond laser-assisted LASIK: comparison among different flap design parameters. Int Ophthalmol 2017;37(3):635-641.
14 Courtin R, Saad A, Guilbert E, Grise-Dulac A, Gatinel D. Opaque bubble layer risk factors in femtosecond laser-assisted LASIK. J Refract Surg 2015;31(9):608-612.
15 Ma JN, Wang Y, Li LY, Zhang JM. Corneal thickness, residual stromal thickness, and its effect on opaque bubble layer in small-incision lenticule extraction. Int Ophthalmol 2018;38(5):2013-2020.
16 Jung HG, Kim J, Lim TH. Possible risk factors and clinical effects of an opaque bubble layer created with femtosecond laser-assisted laser in situ keratomileusis. J Cataract Refract Surg 2015;41(7):1393-1399.
17 Li LY, Schallhorn JM, Ma JN, Zhang L, Dou R, Wang Y. Risk factors for opaque bubble layer in small incision lenticule extraction (SMILE). J Refract Surg 2017;33(11):759-764.