INTRODUCTION
T he most common vision disorders in infants and young children include amblyopia, strabismus, and significant refractive error. Amblyopia affects approximately 1% to 5% of children worldwide[1-4] and is the leading cause of monocular vision loss in children[5-6]. Normal vision development in infancy is a critical stage for the future eyesight of children and adults. Any abnormality in the visual system during this early developmental and maturation phase can modify the normal development of the occipital cortex and cause permanent severe visual loss[7]. Both refractive error and strabismus can lead to amblyopia. Early detection and treatment are necessary in order to prevent permanent loss of vision[8].
There have been a few studies about the prevalence of amblyopia from different regions in China, e.g. a report from 5-15-year-old urban children in southern China(0.92%)[9]. The Refractive Error Study in Children (RESC)survey screened the children aged 5-15y in Shunyi District,northeast of Beijing (0.81%)[10]. The Anyang Childhood Eye Study (ACES) screened 1st and 7th-grade students in Anyang,central China (1.0% and 2.5%)[11]. Lu et al[12] reported the prevalence of amblyopia was 1.02% in 6-14 years old Tibetan primary school children. Pi et al[13] reported the amblyopia prevalence was 0.75% in 6-15 years old children in western China. However, except the most recent population-based cohort study conducted in preschool children aged 36-72mo in a metropolis in Eastern China[14], little information regarding the epidemiological aspects of vision problems in infants and young children was found in central south China, where a large Chinese population lived. China is the most populous country in the world and its economic development varied a lot across the country, the public health information and implication maybe varied depending on different areas and ethnicity.
The purpose of this cross-sectional study was to identify the prevalence of amblyopia in children aged 30 to 83mo in Hunan Province, central south China. This analysis is also part of the Hunan Childhood Eye Study (HCES). In order to compare the results easily, our protocol is similar to that used in the Baltimore Pediatric Eye Disease Study.
SUBJECTS AND METHODS
Ethical Approval This study was approved by the Committee on Hunan Subjects Research at the Yale University School of Medicine Hunan Investigation Committee, the Second Xiangya Hospital affiliated to Central South University Institutional Review Board (IRB), and the IRB of Hunan Province Health Hygiene (in China). Written informed consent was obtained from parents or legal representatives of all participating children.
Study Design The study is a population-based cross-sectional study performed in an urban area (Changsha, China) and a rural area (Zhangjiajie, China) of Hunan Province, central south of China. The definition of urban areas in China is interpreted as those areas where local governments of the county level or higher are located and are developed, people who live there are usually provided with more resource of education and health care, while the rural areas are governed by village authority and are developing and remain perceived as of a low standard and primitive. In Hunan, most Han Chinese live in urban area and Tujia is the biggest ethnic minority and primarily live in Zhangjiajie. The reason to perform the study in a rural and urban area was that both areas differed markedly in the level of education, access to medical care, mobility, ethnic and way of life. In the rural areas, eye care services and a referral system to ophthalmologists were usually not available. In the urban areas, people are easy to get a relatively high standard eye care and the cost of medical care in some communities was covered by the government. Cluster sampling was used to select subjects from both areas. This study was carried out in nine districts of both Changsha and Zhangjiajie. Five districts were located in Changsha and the other four districts were located in Zhangjiajie.
Recruitment Procedures In China, it is possible to identify households and enumerate children using official streets or village residence registers. We used the clustering method to identify potential families who would then be involved in the initial screening. All children between 30 and 83mo of age who have resided in the selected clusters for at least six months will be enumerated by name, age, and gender.
Invitation letters and information sheets were mailed or transferred by volunteers to parents or guardians who live in the selected clusters through the village districts and street districts. We also posted in every selected streets and villages.Both information sheet and posters explained the importance of the eye screening and procedures of the research. If the parents or guardians want their children participate in the vision screening, written informed consent was obtained from parents or legal representatives of all participating children. And then the children were recruited to be screened as described vision screening section.
Eye Examinations and Interview All children underwent a comprehensive eye examination, including monocular distance optotype visual acuity (VA) testing, evaluation of ocular alignment, anterior segment and dilated fundus evaluations,and measurement of refractive error under cycloplegic conditions[15].
VA was measured in children aged 30 to 83mo with Tumbling E chart at 5 m and near (33 cm) without correction and with correction if the child has glasses. If the children were unable to co-operate with the VA testing, they were provided with more time to learn, and a retest date was scheduled. Subnormal VA was defined after cycloplegic refraction with full correction when 1) VA was decreased in either eye (<20/50 for 30- to 47-month-old or <20/40 for ≥48-month-old); or 2) ≥2 lines of interocular difference (with ≤20/32 in the worse-seeing eye)was present. Children, who had persistent subnormal VA (as defined earlier) in either eye or with an amblyopia risk factor(defined later), were scheduled for return-visit VA retesting with the best correction and without cycloplegic refraction.This test was helpful to remove the potential artifact of testing
after dilation.
Ocular alignment was evaluated by utilizing the Hirschberg light reflex, cover test, and prism cover-uncover tests. Cover tests were performed by using fixation targets at both distance(6 m) and near (33 cm). The presence of strabismus, its characteristics (constant or intermittent), type (exotropia,esotropia, hyper/hypotropia, dissociated vertical deviation),
A-V strabismus and size (prism diopters) was also recorded.Spherical equivalent (SE) refraction was calculated as the numerical sum of the sphere and half of the cylinder. Myopia was defined as SE of - 0.50 D or less, hyperopia as SE ≥+2.00 D,astigmatism as cylinder power ≥1.00 D, and anisometropia as SE difference ≥1.00 D between the 2 eyes.
Parents were invited to complete a comprehensive questionnaire,including questions on the past or present history of amblyopia and strabismus, the type and duration of any treatment provided for amblyopia or strabismus, and the presence of any other past or present ocular problems.
Definition of Amblyopia Unilateral amblyopia was defined as a 2-line interocular difference in best-corrected VA with≤20/32 in the worse eye and with coexisting risk factor of 1) strabismus (upon examination or history of strabismus surgery); 2) anisometropia consistent with the eye with worse VA (≥1.00 D SE anisohyperopia, ≥3.00 D SE anisomyopia, or≥1.50 D anisoastigmatism); or 3) past or present obstruction of the visual axis (e.g. cataract, ptosis, corneal opacity). Bilateral amblyopia was defined as bilaterally decreased best-corrected VA (<20/50 for 30- to 47-month-old or <20/40 for ≥48-monthold) in the presence of bilateral ametropia (≥4.00 D SE hyperopia, ≤-6.00 D SE myopia, or ≥2.50 D astigmatism) or with evidence of visual axis obstruction of both eyes[16].
Statistical Analysis SPSS (Version 12, USA) was used for all statistical analyses. Prevalence of amblyopia and 95%confidence intervals (CI) were estimated. Prevalence rates for amblyopia were determined as the ratio of the number of individuals with amblyopia to the total number examined with stratification by age, gender, and ethnicity. The Chi-square test was utilized to compare proportions for categorical variables;the Fisher exact test was used to calculate P values for comparing amblyopia prevalence between the studies. Twosided P values <0.05 were considered statistically significant.
RESULTS
Study Cohort There were 8042 children enrolled and 7713 children were finally screened in both areas in Hunan Province in the present study. Figures 1 and 2 showed the enrollment procedures. In brief, in the rural area (Zhangjiajie, China),4327 children were enrolled, 4122 eligible children (95.26%)were screened. Totally 3900 (94.61%) children were testable among 4122 recruited children (Figure 1). In the urban area(Changsha, China), 3715 children enrolled, 3591 eligible children (96.66%) were screened. Totally 3456 (96.24%)children were testable among 3715 children (Figure 2). Finally,there were 7356 children included in both areas in the present study.
There are 515 children younger than 4 years old, and 432 children participated in the VA screening. We found half of those children are untestable with Tumbling E chart. In the rural area, 122 (50 girls and 72 boys) of 252 children were testable; in the urban area, 112 (71 girls and 41 boys) of 180 children were testable. The testability is 48.41% in rural area and 62.22% in urban area, there is a statistically significant difference (P=0.0045). For children aged 4 to 7 years old in the urban area, 3344 of 3411children were testable, the testability is 98.04%; while in the rural area, 3778 of 3870 children were testable (97.62%), and there is no significant difference(P=0.2289).
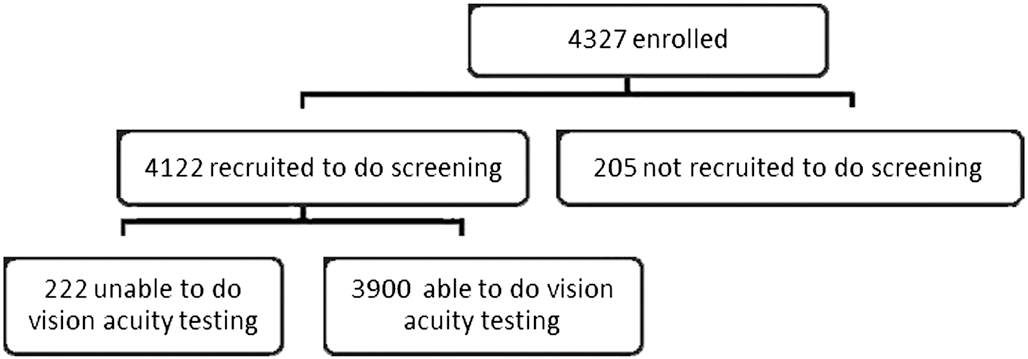
Figure 1 Enrollment of children in vision acuity screening and a complete eye examination in Zhangjiajie, China (rural area).
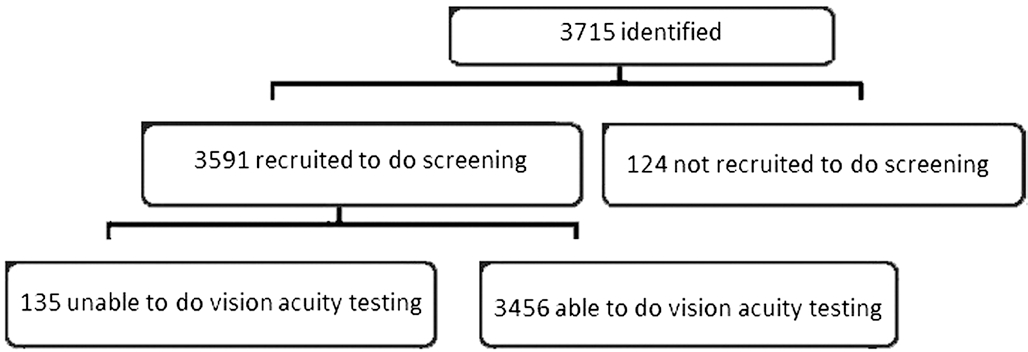
Figure 2 Enrollment of children in vision acuity screening and a complete eye examination in Changsha, China (urban area).
Table 1 Demographic characteristics of the study sample by area distribution n (%)

Parameters Rural (n=3900) Urban (n=3456) Total (n=7356)Age (mo)30-35 39 (1) 51 (1.48) 90 (1.22)36-47 83 (2.13) 61 (1.77) 144 (1.96)48-59 697 (17.87) 616 (17.82) 1313 (17.85)60-71 1206 (30.92) 904 (26.16) 2110 (28.68)72-84 1875 (48.08) 1824 (52.78) 3699 (50.29)Gender Male 2109 (54.08) 1726 (49.94) 3835 (52.13)Female 1791 (45.92) 1730 (50.06) 3521 (47.87)
Table 1 displays the demographic characteristics of the study sample by area. No statistical differences were found in age and gender distribution between the rural and urban area in Hunan.
Prevalence of Amblyopia Among 7356 children in this sample, 80 (1.09%, 95%CI: 0.86% to 1.35%) were identified as amblyopia. Table 2 indicates the number of children with and without amblyopia stratified by age, gender, and area. The 36-to 47-month age group had more amblyopic children (2.08%,3/144) compared with the other age groups, but there was no significant difference in the prevalence of amblyopia across the age groups (P=0.81). The prevalence of amblyopia is 1.08%in rural area and 1.10% in urban area. Neither significant difference was found in the prevalence of amblyopia by area(P=0.93) and gender (P=0.46).
Table 2 Prevalence of amblyopia by age, gender and area distribution
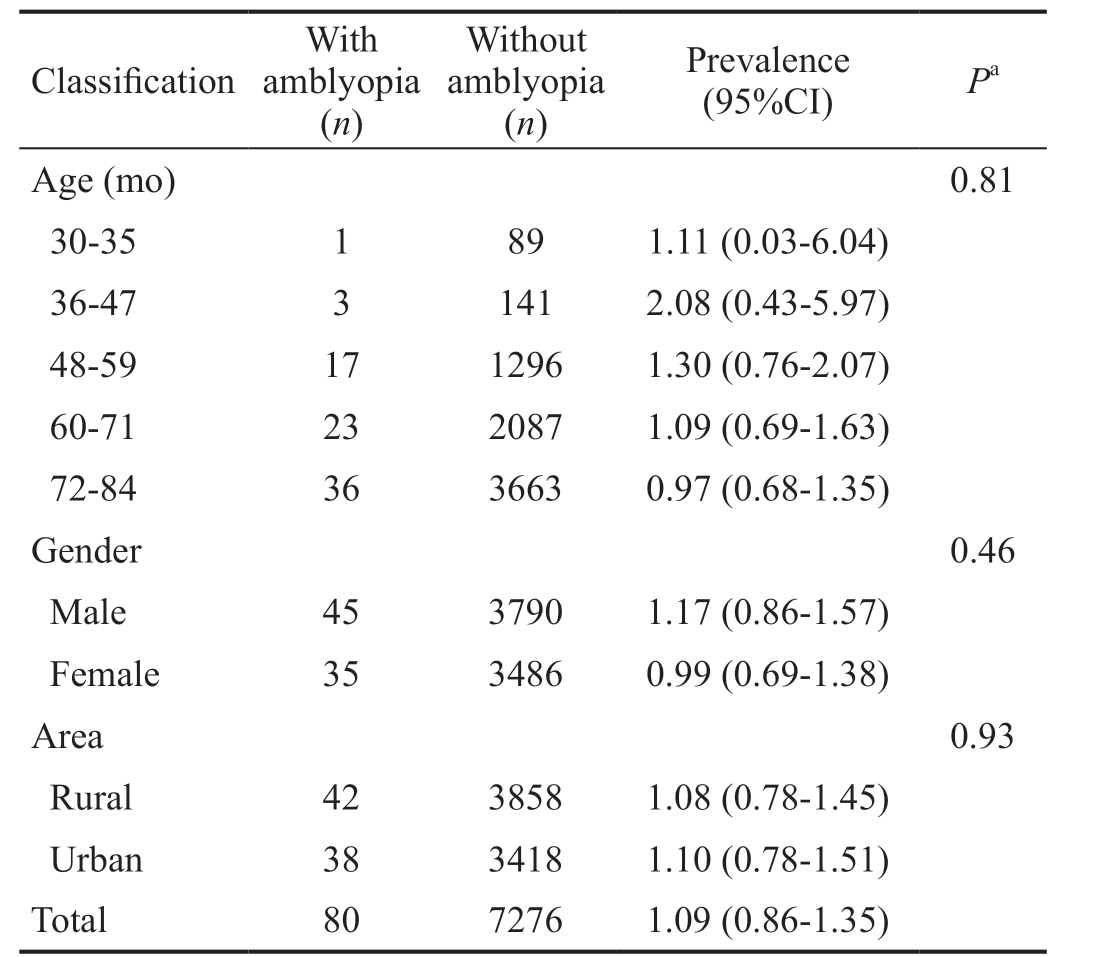
CI: Confidence interval. aP value comparing characteristics of children with amblyopia to children without amblyopia.
Classification With amblyopia(n)Without amblyopia(n)Prevalence(95%CI) Pa Age (mo) 0.81 30-35 1 89 1.11 (0.03-6.04)36-47 3 141 2.08 (0.43-5.97)48-59 17 1296 1.30 (0.76-2.07)60-71 23 2087 1.09 (0.69-1.63)72-84 36 3663 0.97 (0.68-1.35)Gender 0.46 Male 45 3790 1.17 (0.86-1.57)Female 35 3486 0.99 (0.69-1.38)Area 0.93 Rural 42 3858 1.08 (0.78-1.45)Urban 38 3418 1.10 (0.78-1.51)Total 80 7276 1.09 (0.86-1.35)
Table 3 summarizes the prevalence of unilateral and bilateral amblyopia of potential causes across the rural and urban areas. Unilateral amblyopia was diagnosed in 50 children(0.68%, 50/7356), and bilateral amblyopia was diagnosed in 30 children (0.41%, 30/7356). Of the 30 bilateral amblyopia,29 children were refractive amblyopia and one had deprivation amblyopia with bilateral congenital cataract. Anisometropia without strabismus was responsible for most amblyopia cases(40%, 32/80). The second is binocular refractive amblyopia(36%, 29/80). Table 4 shows the refractive components of the children with ametropic and anisometropic amblyopia.Of the 61 children, 53 children (86.89%) had astigmatism≥1.00 D, 5 children (8.20%) had hyperopia ≥+2.0 D and only 3 children (4.92%) had myopia ≤-0.5 D. Of the 53 children with astigmatism, around half of the children (47.17%) had hyperopia combined with astigmatism.
Strabismus amblyopia was present in 11 children (14%,11/80, 7 esotropia, 1 vertical deviation and 3 exotropia), visual deprivation was present in 8 children (10%, 8/80). Of the 8 children with visual deprivation, 1 is for congenital ptosis, 2 are for congenital cataract with nystagmus, 4 are for corneal macula and 1 is for traumatic cataract (Table 5).
Among the 80 amblyopic children, there were 7 children(16.67%) in the rural area and 14 (36.84%) children in the urban area, who had been diagnosed as amblyopia before our study. For the previous diagnosis, there was a statistically significant difference between both areas (P=0.04). Of these 21 children, 1 child in the rural area and 2 children in the urban area have reached normal VA after correcting their refractive error and patching.
Table 3 Prevalence of unilateral and bilateral amblyopia by potential causes n (%)
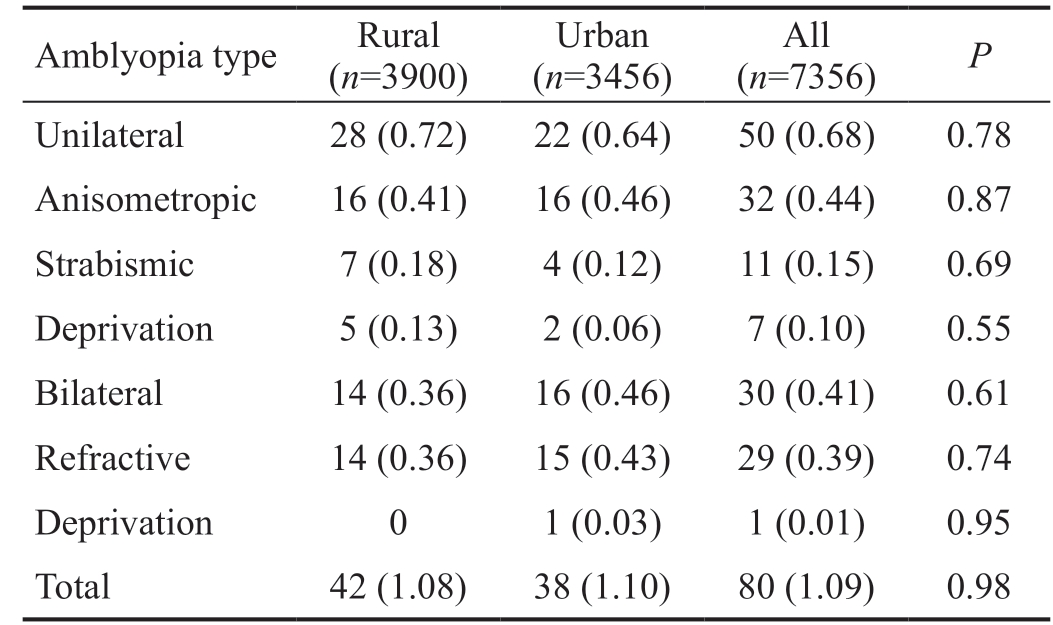
Amblyopia type Rural(n=3900)Urban(n=3456)All(n=7356) P Unilateral 28 (0.72) 22 (0.64) 50 (0.68) 0.78 Anisometropic 16 (0.41) 16 (0.46) 32 (0.44) 0.87 Strabismic 7 (0.18) 4 (0.12) 11 (0.15) 0.69 Deprivation 5 (0.13) 2 (0.06) 7 (0.10) 0.55 Bilateral 14 (0.36) 16 (0.46) 30 (0.41) 0.61 Refractive 14 (0.36) 15 (0.43) 29 (0.39) 0.74 Deprivation 0 1 (0.03) 1 (0.01) 0.95 Total 42 (1.08) 38 (1.10) 80 (1.09) 0.98
Table 4 Refractive composition of children with ametropic and anisometropic amblyopia n=61

SE: Spherical equivalence; D: Diopter.
Refractive error n (%) Range of SE (D)Myopia 3 (4.92) -8.0 to -5.5 Hyperopia 5 (8.20) +0.5 to 14.0 Astigmatism 13 (21.31) -1.75 to +2.0 Hyperopia+astigmatism 25 (40.98) +1.5 to +14.75 Myopia+astigmatism 15 (24.59) -0.5 to -6.25
Table 5 Causes of deprivation amblyopia in rural and urban area
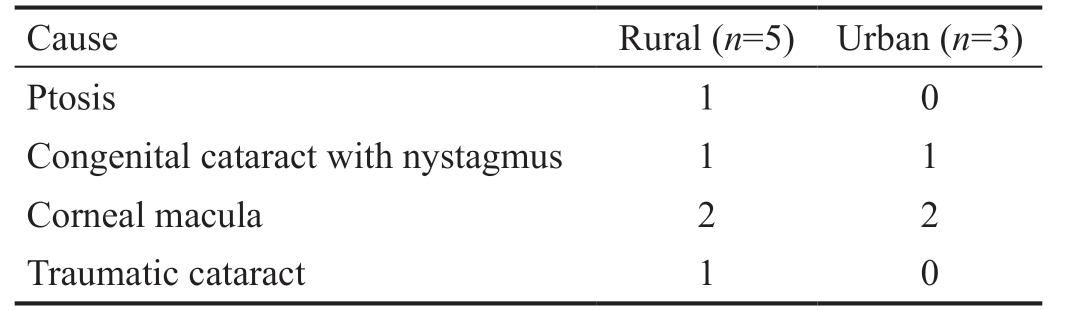
Cause Rural (n=5) Urban (n=3)Ptosis 1 0 Congenital cataract with nystagmus 1 1 Corneal macula 2 2 Traumatic cataract 1 0
DISCUSSION
The prevalence of amblyopia was 1.09% in this populationbased study of 7356 Chinese children aged 30mo through 83mo in central south China, Hunan Province. Our study reported relatively lower amblyopia prevalence compared with the Sydney Paediatric Eye Disease Study (SPEDS, 2.07%in Australian)[17], Multi-Ethnic Pediatric Eye Disease Study(MEPEDS, 1.63% in African-American, 2.79% in Hispanic/Latino, 1.76% in Asian and 2.00% in non-Hispanic white)[3] and the Baltimore Pediatric Eye Disease Study (BPEDS, 1.89%in white)[2], but comparable with the Strabismus, Amblyopia and Refractive Error in Singaporean Children Study (STARS,1.19% in Singaporean Chinese children)[4] and other studies in China, e.g. with 0.92% , 0.87% and 1.20% in Shunyi[10],Guangzhou[9] and Nanjing[14]. A likely explanation for this is ethnicity-related difference. The lower rate in Shunyi and Guangzhou may be related to the different criteria employed in the studies and not including the deprivation amblyopia. Our study also showed that the prevalence of amblyopia was 1.08%in the rural area and 1.10% in the urban area. There was no statistically significant difference between both areas (P=0.93).
The present study also indicated no statistically significant difference was found in a different age group, gender, and area distribution (Table 2). Although there was no significant difference in amblyopia prevalence across different age groups in the present sample, the prevalence was highest among the 36 to 47mo age group. This could be biased because of the smaller testable sample in the study. However, a cohort difference may exist because there were less screening and treatment of amblyopia provided to the younger generation in central south China, especially the rural area, compared to eastern China with good economy[14]. Therefore, our data indicate that most cases of amblyopia have developed and can be detected by 3 to 4y of age and also implies that preschool vision screening is necessary for detecting amblyopia[3].
Anisometropia without strabismus was responsible for most amblyopia cases (40%, 32/80) in our study. The second is binocular refractive amblyopia (36%, 29/80). Strabismus amblyopia was present in 11 children (14%, 11/80). Similarly,in Singapore, the most frequent causes of amblyopia were refractive error (85%) and strabismus (15%)[4]. Deprivation amblyopia affects 8 children in the present study, 5 in the rural area and 3 in the urban area. Trauma is an important cause that leads to vision loss, especially in the rural area. There are two children who suffered from corneal trauma and one child who suffered from traumatic cataract. Prevention is critical to avoiding pediatric ocular trauma. However, lack of parental supervision, especially in the rural area is the main social issue in China now and this partly explained why trauma is an important cause of the deprivation amblyopia in our study.Therefore, effective custody of children should be emphasized and improved in China, especially in rural area.
It was found that the number of bilateral amblyopia cases was almost equal to half of the unilateral amblyopia cases in the present study (Table 3). The prevalence of bilateral amblyopia in our study was 0.41%. This result is consistent with some other recent preschool studies (0.48% in Nanjing, Eastern China Study and 0.45% in MEPEDS, 0.36% in STARS)[3,14],but higher than that of BPEDS (0.06%)[2]. Bilateral amblyopia may have a greater impact on daily visual function than unilateral cases. Most of the bilateral cases were linked to high levels of refractive error. Our study suggests an urgent need for implementing an initial comprehensive vision screening service for preschoolers in central south China.
Among all types of refractive errors which lead to ametropic amblyopia and anisometropic amblyopia in the study,astigmatism is the main type of refractive error that leads to amblyopia (53, 86.89%). For astigmatism, hyperopia combined with astigmatism is the most important reason leading to amblyopia (25 children, 47.17%). These findings suggest that screening and correcting for significant astigmatism, especially for hyperopia combined with astigmatism, is very important for young children.
In the present study, 7 children (16.67%) in the rural area and 14 (36.84%) children in the urban area have been diagnosed as amblyopia before screening. One child in the rural area and two children in the urban area have reached normal VA after correcting the refractive error and patching. We still count them as the number of amblyopia. Otherwise the prevalence of amblyopia would be underestimated. These are the proof that early diagnosis and treatment are necessary to prevent permanent amblyopia.
The differences in socioeconomic status may result in differences in eye health awareness and access to eye health care. However, the prevalence of amblyopia in the rural area is comparable to that in the urban area in the present study.It is very interesting. Usually, people believe that different socioeconomic conditions, overall health, rates of prematurity will influence the rate, but we didn’t see the difference. In the study, we noticed the testability for the children younger than 4 years old in the rural area (48.41%) was much lower than that of the urban area (62.22%, P=0.0045). We assumed that socioeconomic status may result in this difference. Although it is unreliable for detecting decreased VA for children younger than 4 years old, lack of those data may decrease the estimate of the prevalence of amblyopia if those untestable children were more likely to have amblyopia than those who were testable. In addition, the definition of amblyopia in different research is diverse which will also lead to the bias of the prevalence.
There are a few limitations of our study. Firstly, we only did a comprehensive examination for those children with VA lower than 20/32, thus those with good vision who may be suffering from other eye diseases couldn’t be detected. Secondly,not all children identified can enter the data analysis for the prevalence of amblyopic because some of them couldn’t cooperate with the tests, which will underestimate the overall rate, especially for those children younger than 4 years old. In addition, we used Tumbling E which is cheap and convenient to test VA, but it seems more difficult for young children to understand and thus influence the testability.In sum, the prevalence of amblyopia in children aged 30 to 83mo in central south China was 1.09% (95%CI 0.86% to 1.35%). Although the prevalence of amblyopia in Hunan Province is low, it still influences around 35 000 children.Early screening may change those children’s life.
ACKNOWLEDGEMENTS
Foundations: Supported by chia funding of Yale-China Association, the National Natural Science Foundation of China (No.81570847); the Natural Science Foundation of Hunan Province (No.2016JJ4095); the Programs of Science-Technology Commission of Hunan Province(No.2015JC3036); Department of Science and Technology,Hunan (No. 2015TP2007).
Conflicts of Interest: Li YP, None; Zhou MW, None; Forster SH, None; Chen SY, None; Qi X, None; Zhang HM, None;Luo J, None.
1 Robaei D, Kifley A, Rose KA, Mitchell P. Impact of amblyopia on vision at age 12y: findings from a population-based study. Eye (Lond)2008;22(4):496-502.
2 Friedman DS, Repka MX, Katz J, Giordano L, Ibironke J, Hawse P,Tielsch JM. Prevalence of amblyopia and strabismus in white and African American children aged 6 through 71mo the Baltimore Pediatric Eye Disease Study. Ophthalmology 2009;116(11):2128-2134.e1-2.
3 Multi-ethnic Pediatric Eye Disease Study Group. Prevalence of amblyopia and strabismus in African American and Hispanic children ages 6 to 72mo the multi-ethnic pediatric eye disease study. Ophthalmology 2008;115(7):1229-1236.e1.
4 Chia A, Dirani M, Chan YH, Gazzard G, Au Eong KG, Selvaraj P,Ling Y, Quah BL, Young TL, Mitchell P, Varma R, Wong TY, Saw SM.Prevalence of amblyopia and strabismus in young Singaporean Chinese children. Invest Ophthalmol Vis Sci 2010;51(7):3411-3417.
5 Multi-Ethnic Pediatric Eye Disease Study (MEPEDS) Group.Prevalence and causes of visual impairment in African-American and Hispanic preschool children: the multi-ethnic pediatric eye disease study.Ophthalmology 2009;116(10):1990-2000.e1.
6 Robaei D, Huynh SC, Kifley A, Mitchell P. Correctable and non
correctable visual impairment in a population-based sample of 12-yearold Australian children. Am J Ophthalmol 2006;142(1):112-118.
7 Carlton J, Karnon J, Czoski-Murray C, Smith KJ, Marr J. The clinical effectiveness and cost-effectiveness of screening programmes for amblyopia and strabismus in children up to the age of 4-5y: a systematic review and economic evaluation. Health Technol Assess 2008;12(25):iii,xi-iii,194.
8 Solebo AL, Cumberland PM, Rahi JS. Whole-population vision screening in children aged 4-5y to detect amblyopia. Lancet 2015;385(9984):2308-2319.
9 He MG, Zeng JW, Liu YZ, Xu JJ, Pokharel GP, Ellwein LB. Refractive error and visual impairment in urban children in southern china. Invest Ophthalmol Vis Sci 2004;45(3):793-799.
10 Zhao J, Pan X, Sui R, Munoz SR, Sperduto RD, Ellwein LB.Refractive error study in children: results from Shunyi district, China. Am J Ophthalmol 2000;129(4):427-435.
11 Fu J, Li SM, Li SY, Li JL, Li H, Zhu BD, Yang Z, Li L, Wang NL.Prevalence, causes and associations of amblyopia in year 1 students in Central China. Graefes Arch Clin Exp Ophthalmol 2014;252(1):137-143.
12 Lu P, Chen XM, Zhang WF, Chen SJ, Shu L. Prevalence of ocular disease in Tibetan primary school children. Can J Ophthalmol 2008;43(1):95-99.
13 Pi LH, Chen L, Liu Q, Ke N, Fang J, Zhang S, Xiao J, Ye WJ, Xiong Y, Shi H, Zhou XY, Yin ZQ. Prevalence of eye diseases and causes of visual impairment in school-aged children in Western China. J Epidemiol 2012;22(1):37-44.
14 Chen XJ, Fu ZJ, Yu JJ, Ding H, Bai J, Chen J, Gong Y, Zhu H, Yu RB,Liu H. Prevalence of amblyopia and strabismus in Eastern China: results from screening of preschool children aged 36-72mo. Br J Ophthalmol 2016;100(4):515-519.
15 Borchert MS, Varma R, Cotter SA, Tarczy-Hornoch K, McKean-Cowdin R, Lin JH, Wen G, Azen SP, Torres M, Tielsch JM, Friedman DS,Repka MX, Katz J, Ibironke J, Giordano L, Multi-Ethnic Pediatric Eye Disease Study and the Baltimore Pediatric Eye Disease Study Groups.Risk factors for hyperopia and myopia in preschool children the multiethnic pediatric eye disease and Baltimore pediatric eye disease studies.Ophthalmology 2011;118(10):1966-1973.
16 McKean-Cowdin R, Cotter SA, Tarczy-Hornoch K, Wen G, Kim J,Borchert M, Varma R, Multi-Ethnic Pediatric Eye Disease Study Group.Prevalence of amblyopia or strabismus in Asian and non-Hispanic white preschool children: multi-ethnic pediatric eye disease study.Ophthalmology 2013;120(10):2117-2124.
17 Pai AS, Rose KA, Leone JF, Sharbini S, Burlutsky G, Varma R, Wong TY, Mitchell P. Amblyopia prevalence and risk factors in Australian preschool children. Ophthalmology 2012;119(1):138-144.