INTRODUCTION
G laucoma is the second major causes of blindness according to the WHO estimates[1], with increasing intraocular pressure (IOP) and progressive damage of optic nerve which induced visual loss. According to the anterior chamber angle, glaucoma is divided into open angle and closed angle. The reasons for primary angle closure glaucoma(PACG) are varied, but the one that dominates is the extent of permanent peripheral anterior synechiae (PAS) closing asymptotically. The anterior chamber narrows progressively causing the pupillary block and then an increase in IOP.
Controlling the level of IOP is confirmed to reduce development of glaucoma. For treating angle-closure glaucoma (ACG), if the medication has little effort, the major surgical therapies attempt to widen the angle and increase the drainage of aqueous fluid by performing laser peripheral iridoplasty, antiglaucoma procedure such as trabeculectomy and bypass device implantation, as well as lens extraction. However, PAS may also reoccur even after the laser and filtering surgery and reduce the aqueous flow[2].
PACG with coexisting lens opacity are the leading causes of visual impairment for elders, which would affect female in Asian regions especially[3]. According to previous studies, the combination of cataract extraction and trabeculectomy results in a more significant decrease of IOP after the surgery, but there might be more postoperative complications[4]. Many studies indicated that phacoemulsification (phaco) alone with foldable intraocular lens (IOL) implantation is a conservative treatment in deepening the anterior chamber depth and reducing IOP[5-7]. Cataract surgery has been proved effective for controlling the IOP, due to the advanced surgery technics,clear lens extraction gradually became an alternative for treating PACG nowadays[8].
Goniosynechialysis (GSL) was first described as a procedure in 1984 by Campbell and Vela[9] and was performed with phaco in 1999[10], which became a potentially economic alternative for surgeons to decrease IOP instead of trabeculectomy. Several studies indicate that standard cataract surgery combined with GSL is a more effective and safe treatment in reducing IOP than routine cataract extraction alone[11-15]. However, a few trials found that the combination procedure has no advantage to control the IOP appropriately[16].
It is not clear how much the IOP controlling and medication decreasing effect can be contributed to the phaco alone or with GSL based on clinical evidence and follow-up data. This has been an important and controversial issue to compare which intervention for treating glaucoma and cataract is safer, more effective, and has more stable outcomes, fewer complications than the others. This analysis aims to address these problems based on published international cross randomized controlled trials (RCTs). To our knowledge, this is a Meta-analysis which firstly compares the phaco surgery alone and with GSL.
MATERIALS AND METHODS
This Meta-analysis was carried out by following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses(PRISMA) statement. The risk of bias was evaluated by the Cochrane Handbook for Systematic Reviews of Interventions.All seven included studies’ protocols were followed the tenets of the Declaration of Helsinki and were approved by their local ethics committees.
Literature Search Strategy We conducted a systemic literature search on September 17, 2018, by two authors independently in the PubMed, EMBASE, Cochrane Library, ClinicalTrials.gov from their inception to September 2018. The search strategy included the following terms: ‘phacoemulsification OR cataract extraction’,‘goniosynechialysis OR viscogonioplasty’, ‘angle-closure glaucoma’, ‘cataract’. All references were managed by EndNote X8 (Thomson Reuters, New York, NY). The searching work was updated before the statistical analysis performed in case of any latest relative reports published was missed.
We search the reference of every involved study to check the potential additional relative RCTs. We also examined the ongoing clinical trials registered on ClinicalTrials.gov, but none of them had posted results yet.
Study Selection The following inclusion criteria were considered when screening the studies: 1) The study must be RCTs; 2) The patients recruited in RCTs were adults diagnosed with PACG/ACG, PAS and coexisting lens opacity;
3) The patients meeting inclusion criteria randomized to phaco and IOL implantation group or combined with GSL group. Viscogonioplasty (VGP) which means no intraocular instruments, but only viscoelastic material was used to break the PAS during the operation was also included; 4) The main outcome of preoperative and postoperative IOP as well as the number of medications using must be reported; 5) The last follow-up time must be at least two months or longer.
The studies were excluded if they meet the following criteria:1) Retrospective cohort, prospective cohort studies or prospective case series; 2) The postoperative follow-up period was less than two months; 3) The sample size of each group was less than 10.
Data Collection and Quality Assessment A table of summary findings for the primary comparison was presented,which indicates the illustrated comparative risks. Two review authors independently assessed the included studies for their methodological quality. According to the Cochrane Handbook for Systematic Reviews of Interventions (Version 5.1.0), we consider the following domains: 1) Random sequence generation (selection bias): whether the sequence allocation was generated by random approaches; 2) Allocation concealment (selection bias): whether the allocation sequence was implemented without foreknowledge; 3) Blinding of participants and personnel (performance bias): who was blinded and whether the blinding methods affect the outcomes;4) Blinding of outcome assessment (detection bias): any blinding was used and whether it had effects on outcomes assessment; 5) Incomplete outcome data (attrition bias):whether all the predetermined outcomes were reported; 6)Selective reporting (reporting bias): whether all the main outcomes in protocol were reported clearly; 7) Other bias:source of funding and conflicts of interest. Each domain was graded as: low risk of bias, high risk of bias or unclear risk. If the methodology was not reported in the study, the domain was graded as ‘unclear risk’.
We collected the data of mean preoperative IOP measured by Goldmann applanation, mean postoperative IOP at 3, 6 and 12mo, changes of IOP at 12mo after the surgery compared with the baseline, the number of anti-glaucoma medication used after the surgery when needed at 6 and 12mo.
The quality of evidence for outcomes was assessed by two independent reviewers using the Grading of Recommendation Assessment, Development, and Evaluation (GRADE)approach. We considered the following reasons for upgrading or downgrading: the substantial statistical heterogeneity, risk of bias, confidence interval and numbers of subjects.
Statistical Analysis This Meta-analysis was performed using Review Manager version 5.3.5 (The Nordic Cochrane Center,Copenhagen, Denmark). Due to the small amount of studies included, the sensitivity analysis was not performed in this review. Considering all involved reports that met the inclusion criteria, none of them were assessed as high risk of bias on sequence generation and allocation concealment. Therefore,we extracted the available information and numerical results of the publishing text. No extra data was added to the analysis.
The main outcomes were continuous scale, including the mean values of IOP, the mean change of IOP, the number of antiglaucoma medication using postoperatively at different followup point. The mean values and the mean difference (MD) of the total studies were calculated. The fixed and randomized effect model was used depending on the heterogeneity. The heterogeneity was tested by calculating the I2, and the P-value.We considered the I2<50% or the P-value greater than 0.1 indicating the acceptable low heterogeneity and the fixed effect model was applied, otherwise the significant heterogeneity, the randomized model was used.
Publication Bias We did not have enough studies (n=7)to examine the funnel plots of these two interventions. We researched the consensus through discussion and retrieved if disagreement occurs.
RESULTS
Search Results We search several main electronic databases from their inception to September 2018, including 68 from PubMed, 92 from EMBASE, 22 from Qvid, 6 from Cochrane Library and 3 from ClinicalTrial.gov. We removed 58 duplicate reports manually. Two independent reviewers identified the titles and abstracts of 133 records and excluded 120 reports for reasons: 20 were case reports or case series; 7 were reviews or Meta-analysis; 3 were letters, editorial opinions or comments;20 were irrelevant topics; 31 were not RCTs and 39 of the study designs including other surgeries such as trabeculectomy,bypass device implantation etc. The remain 13 studies were screened full-text, and six of records were excluded for reasons as follows: 5 were not reporting the required outcomes or the follow-up time less than 1mo, and 1 was comparing the GSL surgery alone with the phaco-GSL surgery. The remaining seven randomized clinical studies met the inclusion criteria were finally included in this review[11-13,16-19]. The process of studies selection is presented in Figure 1.

Figure 1 Flow diagram of studies identified, included and excluded.
Study Characteristics Analysis of the 7 included RCTs, with a total of 321 participants (358 eyes) diagnosed with ACG and coexisting cataract, received a solo cataract procedure or a phaco-GSL surgery randomly. All participants recruited in these seven included studies underwent standard phaco through a clear corneal incision, and IOL implantation under general or peribulbar anesthesia. For subjects who were randomized to phaco-GSL surgery group, GSL was performed after the IOL implantation.
The intervention of three studies was VGP, which means injecting much viscoelastic material near the angle to break the PAS, carefully avoiding the damage of surrounding structures,without using any surgical instrument. The remaining three studies, operators performed GSL not only using viscoelastic,but a blunt cyclodialysis spatula was also used for pressing the spatula on the peripheral iris next to the point of angle adhesion and exposing the meshwork. At the end of surgery,the remaining viscoelastic was removed. Four studies used the direct gonioscopy lens during the operation for better visualizing in. The above work was repeated for surgeons to confirm that the most peripheral extent had been eliminated at the end of the operation.
The scale of the population varies from minimum 11 to maximum 50 participants in a group. The characteristic of the 7 studies was summarized in Table 1. Only 1 study[19]was published full-text in Chinese, but with English version abstract, the other articles were in English. Among these studies, 4 of them were conducted in Asia (China, Iran, Korea,and Singapore), remaining 2 were both conducted in the United Kingdom. All studies were conducted at one site, but one was a multicentral trial through Singapore[11]. Only one included study[18] reported the ethnicity of subjects, others did not give the details.
Table 1 Characteristics of included studies
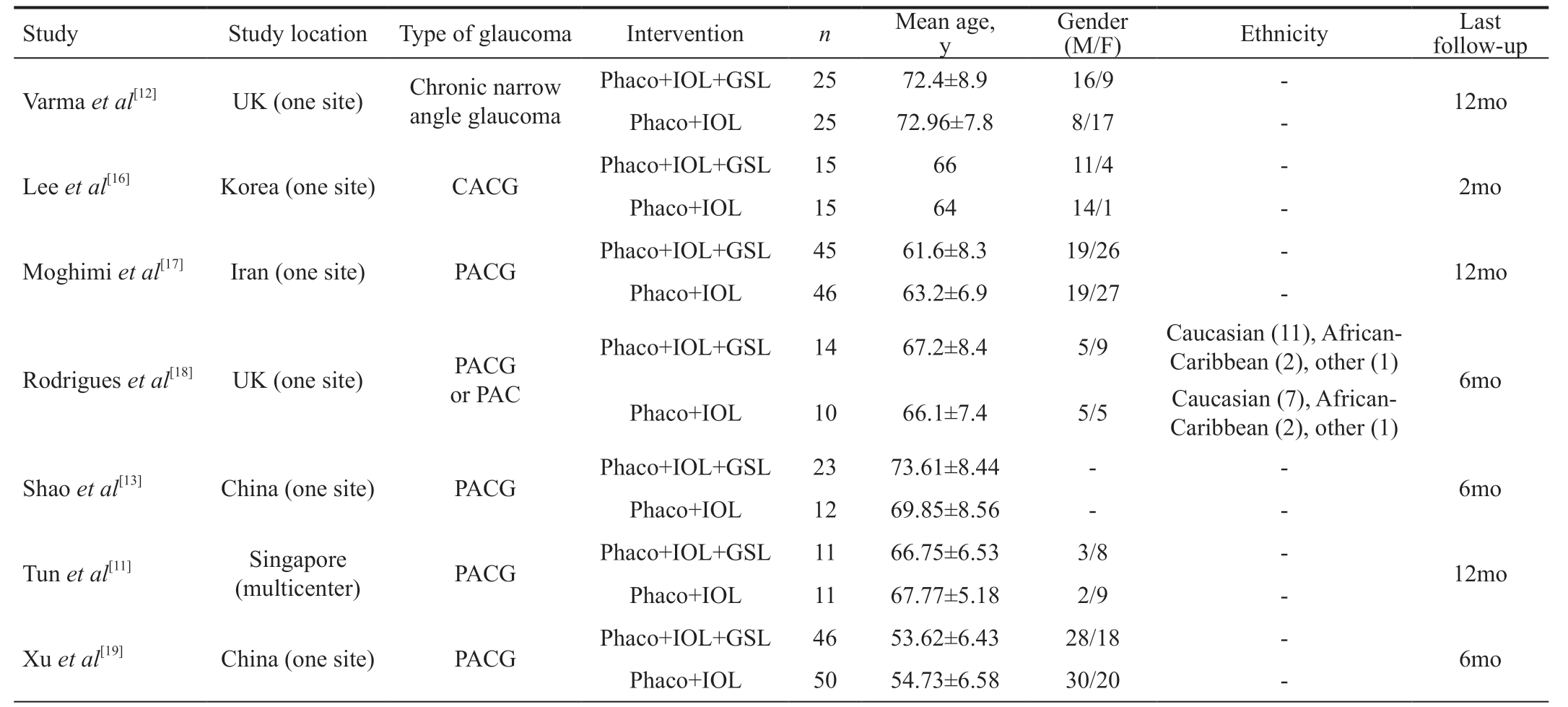
Study Study location Type of glaucoma Intervention n Mean age,y Gender(M/F) Ethnicity Last follow-up Phaco+IOL+GSL 25 72.4±8.9 16/9 - 12mo Phaco+IOL 25 72.96±7.8 8/17 -Lee et al[16] Korea (one site) CACG Phaco+IOL+GSL 15 66 11/4 - 2mo Phaco+IOL 15 64 14/1 -Moghimi et al[17] Iran (one site) PACG Phaco+IOL+GSL 45 61.6±8.3 19/26 - 12mo Phaco+IOL 46 63.2±6.9 19/27 -Varma et al[12] UK (one site) Chronic narrow angle glaucoma Phaco+IOL+GSL 14 67.2±8.4 5/9 Caucasian (11), African-Caribbean (2), other (1) 6mo Phaco+IOL 10 66.1±7.4 5/5 Caucasian (7), African-Caribbean (2), other (1)Shao et al[13] China (one site) PACG Phaco+IOL+GSL 23 73.61±8.44 - - 6mo Phaco+IOL 12 69.85±8.56 - -Tun et al[11] Singapore Rodrigues et al[18] UK (one site) PACG or PAC(multicenter) PACG Phaco+IOL+GSL 11 66.75±6.53 3/8 - 12mo Phaco+IOL 11 67.77±5.18 2/9 -Xu et al[19] China (one site) PACG Phaco+IOL+GSL 46 53.62±6.43 28/18 - 6mo Phaco+IOL 50 54.73±6.58 30/20 -
CACG: Chronic angle-closure glaucoma; PACG: Primary angle-closure glaucoma; PAC: Primary angle-closure; Phaco: Phacoemulsification;IOL: Intraocular lens; GSL: Goniosynechialysis.
Table 2 Comparison of data before the surgery and at the last follow-up time point

aVarma et al[12] reported the percentage of patients whose IOP were controlled without medication, instead of the specific numbers of antiglaucoma medications. The gonioscopic examination were performed before and after the surgery, but the value of the parameters was not available in the study; bShao et al[13] used the anterior segment optical coherence tomography (AS-OCT) device to record the image of anterior chamber angle of different angles, and measured the parameters of AOD, TISA, ARA as well as SSA; cXu et al[19] reported the visual acuity, IOP,visual fields and the central anterior chamber depth before and after the surgery.
Postoperative PAS extant at the last follow-up Varma et al[12]Study Intervention n Last follow-up Preoperative IOP Postoperative IOP at the last follow-up Preoperative number of medications Postoperative number of medications at the last follow-up Preoperative PAS extant Phaco+IOL+GSL 25 12mo 29.68±8.73 16.2±3.55 Not reporteda Not reported Phaco+IOL 25 30.12±7.03 13.7±2.89 Lee et al[16] Phaco+IOL+GSL 15 2mo 15.87±4.02 11.33±2.50 2.07±1.58 0.87±0.92 209.00±114.30 95.00±82.53 Phaco+IOL 15 13.53±2.80 11.20±2.54 1.73±1.33 1.20±0.86 181.33±90.62 62.67±69.23 Moghimi et al[17]Phaco+IOL+GSL 45 12mo 23.3±7.3 14.5±2.5 1.7±1.1 0.4±0.8 245.7±91.3 121.9±88.3 Phaco+IOL 46 22.3±6.3 14.0±3.7 1.2±1.1 0.1±0.3 218.7±105.4 148.6±95.6 Rodrigues et al[18]Phaco+IOL+GSL 14 6mo 27.4±7.2 14.8±2.7 0.923±0.86 0.384±0.18 249.2±83.4 110.8±53.9 Phaco+IOL 10 19.6±5.5 14.2±3.1 0.900±1.20 0.600±0.84 190.0±54.1 168.8±131.2 Shao et al[13] Phaco+IOL+GSL 23 6mo 22.12±5.98 13.65±2.46 2.957±1.15 0 Not reportedb Phaco+IOL 12 23.45±7.99 16.40±5.58 2.950±1.00 0.650±1.09 Tun et al[11]Phaco+IOL+GSL 11 12mo 21.82±5.81 14.36±2.98 1.45±0.93 0.09±0.3 6.27±2.76(Clock hour)2.55±2.46(Clock hour)Phaco+IOL 11 18.73±6.54 16.91±5.72 2.09±1.04 0.55±1.04 5.27±2.46(Clock hour)4.73±2.83(Clock hour)Xu et al[19] Phaco+IOL+GSL 46 6mo 22.07±3.31 14.38±2.56 Not reportedc Not reported Phaco+IOL 50 22.13±3.25 17.47±2.84
Table 2 summarized the main outcomes before and the last visit after the surgery. Two studies did not give the specific data of antiglaucoma medication numbers but one of them reported the IOP well-controlled rate without medication use (52% in Phaco-GSL group versus 36% in the phaco group). Comparing of the extant of PAS in quantity could help understand the effect of surgical procedure, three studies reported the value of PAS in degree and one recorded it as the number of clock hour, one showed the other parameters of anterior chamber angle: angle opening distance (AOD), trabecular-iris space area (TISA), angle recess area (ARA) as well as scleral spur angle (SSA). The follow-up periods ranging from 2 to 12mo.Because of differences in observation outcomes measurements and varies follow-up times, not every trial was involved into many of the outcomes analyzed in this review.
The unit of analysis was almost one eye of one participant.Three studies included both eyes of one patient[12,17,19]. We included the data of both eyes in this review, but the specific random sequence generations of eyes or patients were not reported clearly. Each risk of bias for included studies was summarized according to authors’ judgement and discussion(Figure 2).
Main Outcomes The primary objectives of this Meta-analysis including IOP measured by Goldmann applanation at baseline or after the surgery (Figure 3), postoperative numbers of antiglaucoma medications (Figure 4), and complications occurred intraoperatively and postoperatively.
The involved studies showed that the mean value of IOP at 3 (four studies, one study follow-up at 2mo after surgery was included), 6, 12mo postoperative were not significantly different between the groups. Only two studies reported the change in IOP compared with baseline, the outcome showed no significant differences in IOP decrease between the two interventions.
Although 3 studies showed no significant difference in the number of medications using to reduce IOP at 3mo postoperatively, 2 studies reported that the participants using fewer anti-glaucoma medications at 12mo postoperative in the phaco-GSL surgery group than in the cataract surgery alone group.
The quality of the evidence (Table 3) was graded from very low to moderate. We downgraded for the following reasons:substantial statistical heterogeneity, the risk of bias assessed as unclear or high, wide confidence interval and small numbers of participants.
Seven involved studies reported a few complications:intraoperative hyphema was the most common events, other complications included postoperative inflammation, fibrin reaction, PAS recurrence, IOP spike, macular edema. One patient had a posterior capsule rupture during the cataract extraction and requiring an anterior vitrectomy. None of the included studies reported the serious complications during the surgery and follow-up periods.
According to the GRADE Wording Group of evidence, High certainty means that the true effect lies close to that of the estimate of effect with high confidence. Moderate certainty means the true effect is likely to be close to the estimate of the effect with moderate confidence, there is a possibility that it is substantially different. Low certainty means the confidence in the effect estimate is limited, the true effect may be substantially different from the estimate of the effect. Very low certainty means with little confidence in the effect estimate,the true effect is likely to be substantially different from the estimate of effect.
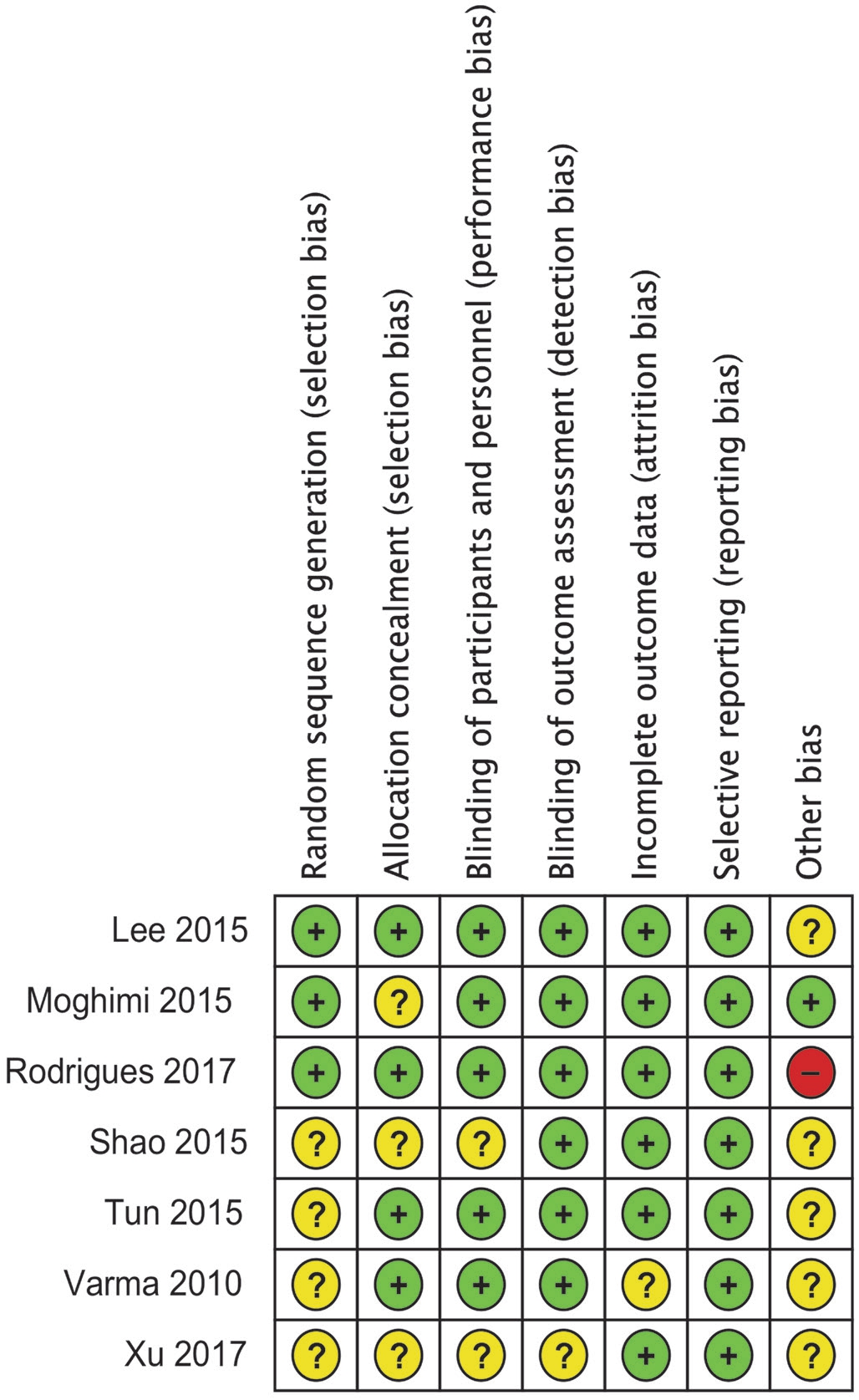
Figure 2 Risk of bias summary.
DISCUSSION
This review included seven RCTs of 358 eyes with glaucoma and coexisting cataract. All studies found a certain effect for reducing the IOP of both standard phaco alone and the combination of phaco and GSL, but it showed the different outcomes of the comparison. We did not find a significant difference between the values of IOP at 3, 6 or 12mo. Although the phaco-GSL surgery group seemed to lower more IOP than the cataract surgery group, 2 trials found no significant difference between the two groups the change of IOP from baseline to 12mo after the surgery.
The total analysis in this study provided low-quality evidence of significant difference in efficacy and safety of phaco with GSL. Five of them reported respectively a better IOPlowering effect of phaco-GSL surgery and 2 of them found no additional benefits of GSL. Some patients in both groups needed to use medications to help better control the IOP postoperatively. The numbers of drug using at 6mo were reported in 3 studies. One study[13] found that the phaco-GSL surgery lead to a significant effect of decreasing the number of medications, all 23 patients in phaco-GSL surgery group was in no need of using eye drops, which make the data of this study not estimable in our analysis. For the other 2 studies, the forest plot showed significant heterogeneity between them.
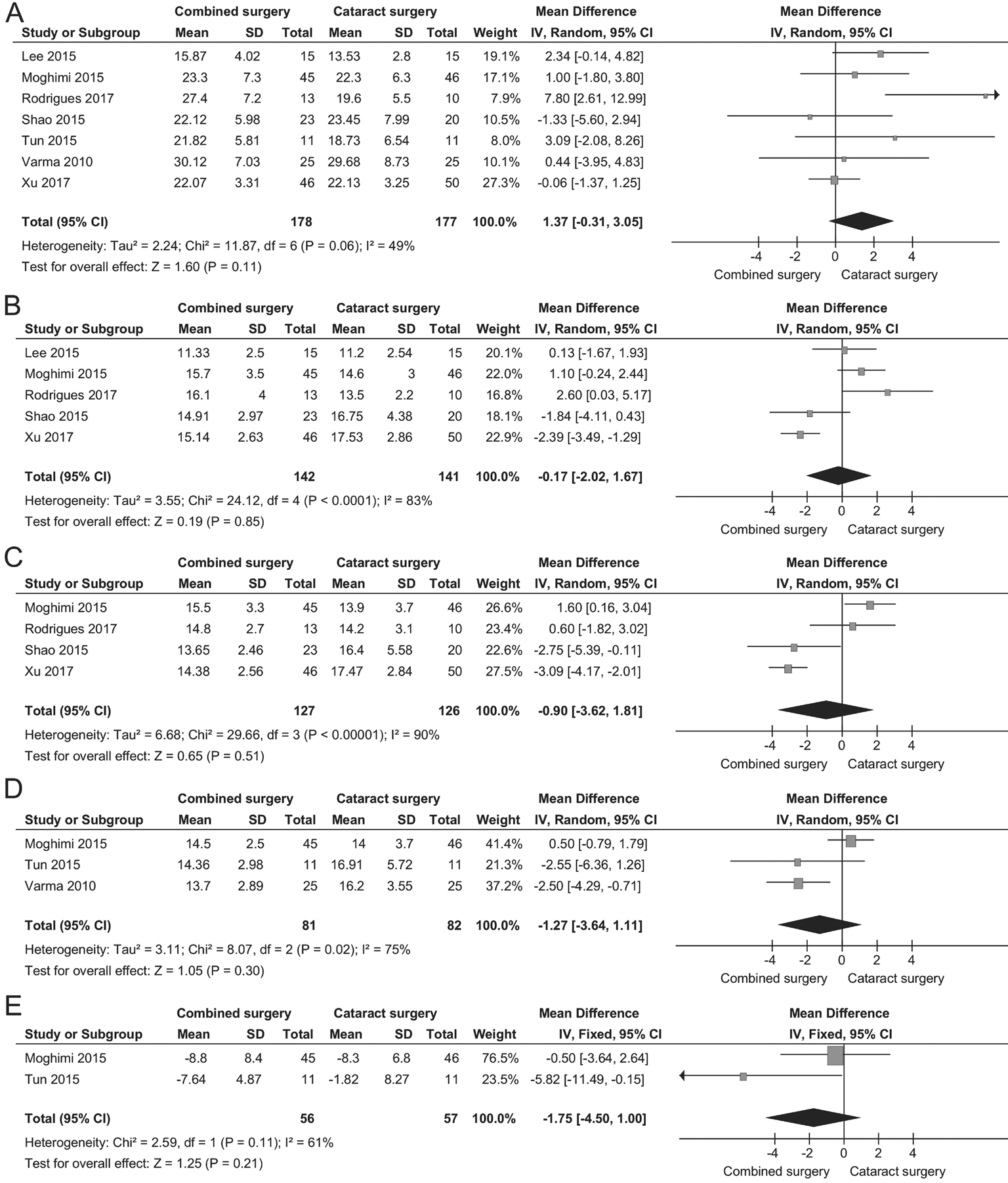
Figure 3 The mean value of IOP before and after the surgery at different follow-up time A: Before the surgery; B: 3mo postoperatively; C:6mo postoperatively; D: 12mo postoperatively; E: The mean postoperative change in IOP at 12mo.
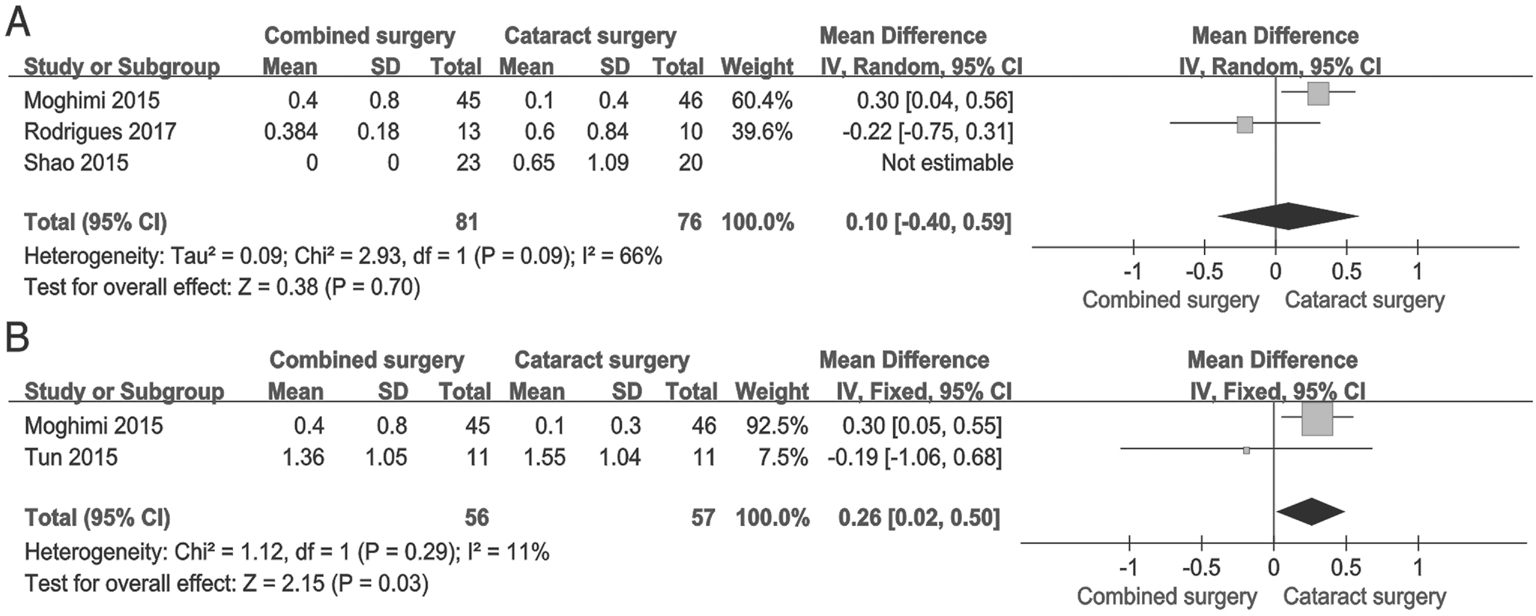
Figure 4 The number of medications after the surgery at different follow-up time A: 6mo postoperatively; B: 12mo postoperatively.
The cause of these difference results may be the variability of surgical techniques, the ethnicity of participants, and the small number of subjects. Despite certain outcome of decreasing the IOP has been achieved in researches, lots of factors are still unknown and its exact mechanism was not clearly demonstrated. It has been reported that the cataract extraction has significant IOP-lowering effect. A large multicentral RCT conducted cross five countries provided high quality of evidence that the clear-lens extraction is a cost-effective intervention for PACG and primary angle-closure with high IOP[8]. Extraction of the lens increases the peripheral anterior chamber depth and widens the anterior chamber angle, which may contribute to the facility of aqueous outflow, and avoid the high risk of complication occurrence after the trabeculectomy.Several previous studies, including retrospective and prospective researches, have also proved the phaco combined with GSL was an effective option to decrease the IOP for ACG[15,20-23]. However, it is still to be considered which procedure plays the most important role in IOP reduction: lens extraction,GSL or its combination.
Table 3 Summary of findings for the main comparison using the GRADE approach
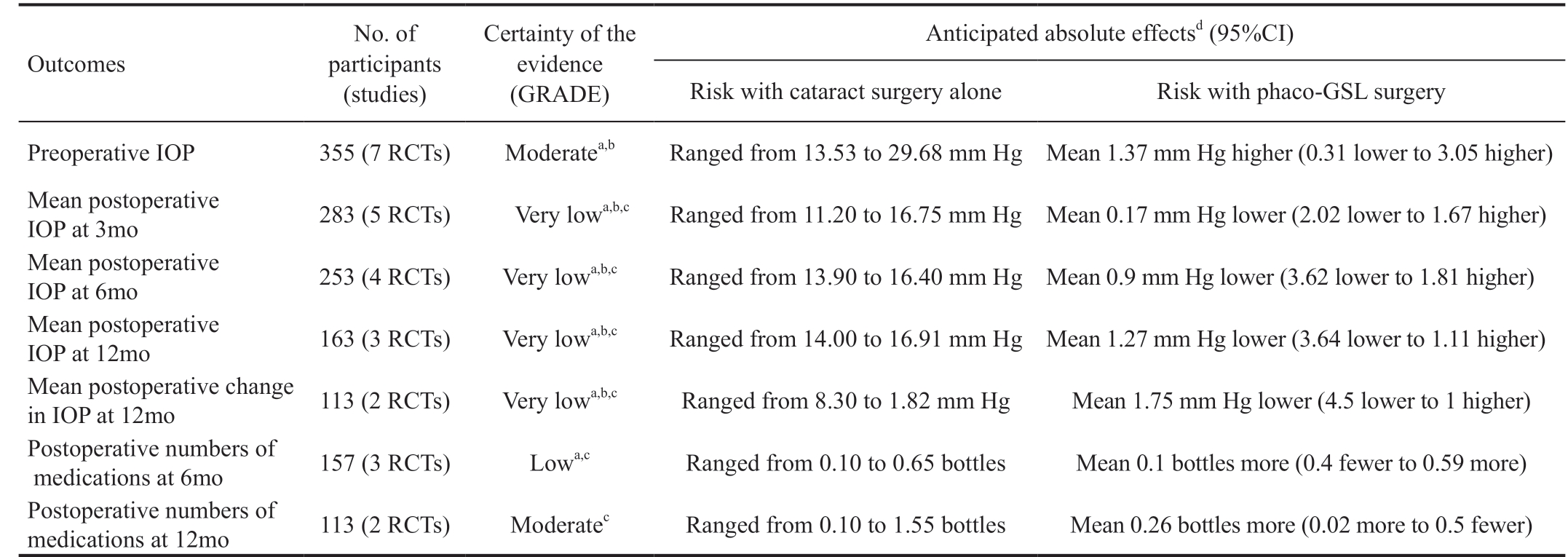
CI: Confidence interval; MD: Mean difference. aSubstantial statistical heterogeneity; bRisk of bias assessed unclear; cWide confidence interval and small numbers of participants; dThe risk in the intervention group (and its 95%CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95%CI).
No. of participants(studies)Outcomes Certainty of the evidence(GRADE)Anticipated absolute effectsd (95%CI)Risk with cataract surgery alone Risk with phaco-GSL surgery Preoperative IOP 355 (7 RCTs) Moderatea,b Ranged from 13.53 to 29.68 mm Hg Mean 1.37 mm Hg higher (0.31 lower to 3.05 higher)Mean postoperative IOP at 3mo 283 (5 RCTs) Very lowa,b,c Ranged from 11.20 to 16.75 mm Hg Mean 0.17 mm Hg lower (2.02 lower to 1.67 higher)Mean postoperative IOP at 6mo 253 (4 RCTs) Very lowa,b,c Ranged from 13.90 to 16.40 mm Hg Mean 0.9 mm Hg lower (3.62 lower to 1.81 higher)Mean postoperative IOP at 12mo 163 (3 RCTs) Very lowa,b,c Ranged from 14.00 to 16.91 mm Hg Mean 1.27 mm Hg lower (3.64 lower to 1.11 higher)Mean postoperative change in IOP at 12mo 113 (2 RCTs) Very lowa,b,c Ranged from 8.30 to 1.82 mm Hg Mean 1.75 mm Hg lower (4.5 lower to 1 higher)Postoperative numbers of medications at 6mo 157 (3 RCTs) Lowa,c Ranged from 0.10 to 0.65 bottles Mean 0.1 bottles more (0.4 fewer to 0.59 more)Postoperative numbers of medications at 12mo 113 (2 RCTs) Moderatec Ranged from 0.10 to 1.55 bottles Mean 0.26 bottles more (0.02 more to 0.5 fewer)
It must be pointed out that the intervention of phaco alone may also have the same effect of deepen the anterior chamber.Injecting viscoelastic and irrigation of the balanced salt solution (BSS) produce pressure during the surgery and lead to the result similar to GSL. On the other hands, these results may suggest that the closed angle is not merely the source of IOP increasing, but the dysfunction of the trabecular meshwork due to the continuous synechiae. The extent and duration of PAS before the surgery have effect on the success of surgery.Therefore, reducing the extent the PAS may not exactly reopen the anterior chamber angle, or will not help eliminating the block of aqueous outflow drainage pathway.
This analysis does have several limitations, including the difference of preoperative IOP and two kinds of surgical procedure (GSL and VGP). The preoperative IOP is an essential influencing factor of IOP decrease after the surgery.One study[18] showed the significant difference of the preoperative IOP between two groups which contribute to a higher heterogeneity of the total analysis.
Breaking the PAS by injecting viscoelastic materials without instrument was set to be performed in the intervention groups in three of these included studies. Ong et al[24] compared the peripheral anterior synechialysis by using either a spatula or viscoelastic in patients with PACG and reported that the participants achieved lower IOP, less medication use and less adverse events by undergoing VGP. We try to group all the studies according to the type of intervention surgeries, but there is no significant effect in decreasing the heterogeneity.Therefore, the subgroup analysis was not performed in this Meta-analysis.
The other limitation is that the extent of postoperative PAS was not reported in every study and was measured by different methods including anterior segment optical coherence tomography (AS-OCT), swept-source optical coherence tomography (SS-OCT) or gonioscopy in various time points, it could not directly compare the values of the anterior chamber structure in details at different follow-up time after surgery. Instead of reporting the change of PAS degree,one study[18] measured the facility of aqueous outflow after the interventions and showed that the phaco-GSL procedure significantly increased the tonographic aqueous outflow (TOF)and reduced the IOP as well as the number of medications.It may contribute to providing evidence of which procedure could decrease IOP effectively or postpone the rate of PAS recurrence.
Overall, the available data reported in all seven included studies were inconsistency, there are no satisfactory and certainty to conclude which procedure is more effective and safer than the other. This is the first Meta-analysis that investigates the comparison of phaco alone and phaco-GSL surgery. Further trials should design a standard protocol prospectively that listed out the sequence generation, allocation concealment,blinding methods and outcome assessment criteria in details, in order to minimize the bias and upgrade the certainty of evidence.Especially, the preoperative and postoperative anterior chamber angle parameters, such as extent of PAS degree, the aqueous outflow facility and extra data should be measured and compared in detail in further studies.
ACKNOWLEDGEMENTS
Conflicts of Interest: Wang N, None; Jia SB, None.
1 Foster A, Resnikoff S. The impact of Vision 2020 on global blindness.Eye (Lond) 2005;19(10):1133-1135.
2 Marchini G, Chemello F, Berzaghi D, Zampieri A. New findings in the diagnosis and treatment of primary angle-closure glaucoma. Prog Brain Res 2015;221:191-212.
3 Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol 2006;90(3):262-267.
4 Tanna AP, Rademaker AW, de Moraes CG, Godfrey DG, Sarkisian SR Jr, Vold SD, Ritch R. Collagen matrix vs mitomycin-C in trabeculectomy and combined phacoemulsification and trabeculectomy: a randomized controlled trial. BMC Ophthalmol 2016;16(1):217.
5 Poley BJ, Lindstrom RL, Samuelson TW. Long-term effects of phacoemulsification with intraocular lens implantation in normotensive and ocular hypertensive eyes. J Cataract Refract Surg 2008;34(5):735-742.
6 Sengupta S, Venkatesh R, Krishnamurthy P, Nath M, Mashruwala A, Ramulu PY, Robin AL, Lee P. Intraocular pressure reduction after phacoemulsification versus manual small-incision cataract surgery: a randomized controlled trial. Ophthalmology 2016;123(8):1695-1703.
7 Riva I, Katsanos A, Oddone F, Quaranta L. The effect of phacoemulsification on intraocular pressure in eyes with hyperfiltration following trabeculectomy: a prospective study. Adv Ther 2018;35(1):116-123.8 Azuara-Blanco A, Burr J, Ramsay C, Cooper D, Foster PJ, Friedman DS, Scotland G, Javanbakht M, Cochrane C, Norrie J; EAGLE Study Group. Effectiveness of early lens extraction for the treatment of primary angle-closure glaucoma (EAGLE): a randomised controlled trial. Lancet 2016;388(10052):1389-1397.
9 Campbell DG, Vela A. Modern goniosynechialysis for the treatment of synechial angle-closure glaucoma. Ophthalmology 1984;91(9):1052-1060.
10 Teekhasaenee C, Ritch R. Combined phacoemulsification and goniosynechialysis for uncontrolled chronic angle-closure glaucoma after acute angle-closure glaucoma. Ophthalmology 1999;106(4):669-674;discussion 674-675.
11 Tun TA, Baskaran M, Perera SA, Htoon HM, Aung T, Husain R.Swept-source optical coherence tomography assessment of iris-trabecular contact after phacoemulsification with or without goniosynechialysis in eyes with primary angle closure glaucoma. Br J Ophthalmol 2015;99(7):927-931.
12 Varma D, Adams W, Bunce C, Phelan P, Fraser S. Viscogonioplasty in narrow angle glaucoma: a randomized controlled trial. Clin Ophthalmol 2010;4:1475-1479.
13 Shao T, Hong J, Xu J, Le Q, Wang J, Qian S. Anterior chamber angle assessment by anterior-segment optical coherence tomography after phacoemulsification with or without goniosynechialysis in patients with primary angle closure glaucoma. J Glaucoma 2015;24(9):647-655.
14 Eslami Y, Latifi G, Moghimi S, Ghaffari R, Fakhraie G, Zarei R, Jabbarvand M, Mohammadi M, Lin S. Effect of adjunctive viscogonioplasty on drainage angle status in cataract surgery: a randomized clinical trial. Clin Exp Ophthalmol 2013;41(4):368-378.
15 Harasymowycz PJ, Papamatheakis DG, Ahmed I, Assalian A, Lesk M, Al-Zafiri Y, Kranemann C, Hutnik C. Phacoemulsification and goniosynechialysis in the management of unresponsive primary angle closure. J Glaucoma 2005;14(3):186-189.
16 Lee CK, Rho SS, Sung GJ, Kim NR, Yang JY, Lee NE, Hong SM, Kim CY. Effect of goniosynechialysis during phacoemulsification on IOP in patients with medically well-controlled chronic angle-closure glaucoma. J Glaucoma 2015;24(6):405-409.
17 Moghimi S, Latifi G, ZandVakil N, Mohammadi M, Khatibi N,Soltani-Moghadam R, Lin S. Phacoemulsification versus combined phacoemulsification and viscogonioplasty in primary angle-closure glaucoma: a randomized clinical trial. J Glaucoma 2015;24(8):575-582.
18 Rodrigues IA, Alaghband P, Beltran Agullo L, Galvis E, Jones S,Husain R, Lim KS. Aqueous outflow facility after phacoemulsification with or without goniosynechialysis in primary angle closure: a randomised controlled study. Br J Ophthalmol 2017;101(7):879-885.
19 Xu XS, Wan XH, Jiang LJ, Sun DC. Clinical study of phacoemulsification and intraocular lens implantation combined with goniosynechialysis in the treatment of primary chronic angle closure glaucoma. International Eye Science 2017;17(12):2289-2291.
20 Zhang GQ, Zhong SG. Efficacy of phacoemulsification combined with goniosynechialysis in treating primary angle-closure glaucoma with agerelated cataract. International Eye Science 2018;18(3):495-497.
21 White AJ, Orros JM, Healey PR. Outcomes of combined lens extraction and goniosynechialysis in angle closure. Clin Exp Ophthalmol 2013;41(8):746-752.
22 Kameda T, Inoue T, Inatani M, Tanihara H; Japanese Phaco-Goniosynechialysis Multicenter Study Group. Long-term efficacy of goniosynechialysis combined with phacoemulsification for primary angle closure. Graefes Arch Clin Exp Ophthalmol 2013;251(3):825-830.
23 Lai JS, Tham CC, Lam DS. The efficacy and safety of combined phacoemulsification, intraocular lens implantation, and limited goniosynechialysis, followed by diode laser peripheral iridoplasty, in the treatment of cataract and chronic angle-closure glaucoma. J Glaucoma 2001;10(4):309-315.
24 Ong EL, Ng J, Yong V, Yip L, Wong HT, Hee O, Thomas A,Sangtam T, Cheng J. Efficacy and safety of phacoemulsification with goniosynechialysis compared to phacoemulsification with viscosynechialysis in primary angle closure glaucoma-12 month results.Clin Exp Ophthalmol 2016;44(Suppl 1):51.