INTRODUCTION
A ccurate intraocular lens (IOL) calculation is extremely important to achieve the desired refractive outcome,which is less predictable in cataract patients with high myopia[1]. Biometry measurements are necessary to accurately calculate the IOL power[2]. The IOL Master 500 (Carl Zeiss Meditec, Germany) is a fast optical biometer that is based on partial coherence interferometry (PCI), and has been used for several years to measure ocular parameters with high precision[3]. The OA-2000 (Tomey, Naoya, Japan) is newest optical biometry device that combines swept source optical coherence tomography (SS-OCT) and Placido disk topography[4]. It is fast, easy-to-use, and can measure seven ocular parameters including the axial length (AL), keratometry(K), anterior chamber depth (ACD), white-to-white (WTW)corneal diameter, lens thickness (LT), pupil size and central corneal thickness (CCT)[5-6].
Several studies have demonstrated good agreement between measurements obtained using the OA-2000 and the IOL Master 500 in subjects with normal AL[4,6]. To the authors’ knowledge,the use of the OA-2000 in cataract patients with high myopia has not been previously reported. Therefore, the objective of this study was to compare AL, K and ACD measurements,and the predicted outcomes of IOL power in cataract patients with high axial myopia obtained using the OA-2000 and IOL Master 500 instruments.
SUBJECTS AND METHODS
Ethical Approval The study conformed to the Declaration of Helsinki and was approved by the Research Ethics Committee.Cataract patients with high myopia examined between April 2018 to September 2018 at the Joint Shantou International Eye Center of Shantou University and the Chinese University of Hong Kong, Shantou, China were included in this study.All patients provided written informed consent ahead of participation.
Patient Examinations Patients with high myopia (AL≥26 mm) intending to undergo cataract surgery were invited to participate. Exclusion criteria included the following: 1)previous ocular surgery; 2) ocular diseases such as glaucoma,corneal disease, or significant retinal disease; 3) severe corneal or vitreous opacities; 4) intraoperative or postoperative complications.
Ocular biometry measurements were performed by two experienced examiners using OA-2000 and IOL Master 500.
The AL, ACD and K were compared. Mean values of both the flat and steep corneal curvatures were reported in diopters(D). To calculate IOL power, the SRK-T formula was used.Ultrasonic evaluation B scan was used to assess the presence of posterior staphyloma.Cataract surgery was performed with phacoemulsification through a 2.8-mm clear corneal incision using standard techniques under local anesthesia. The power of implanted IOLs was selected to target mild to moderate postoperative myopia. Postoperative manifest refraction was obtained 3wk after surgery or later. Mean absolute refractive error (MAE)was defined as the absolute value of the predicted error for each device obtained using the IOL power calculation formula.
Table 1 Comparison of OA-2000 and IOL Master 500 measurements mean±SD
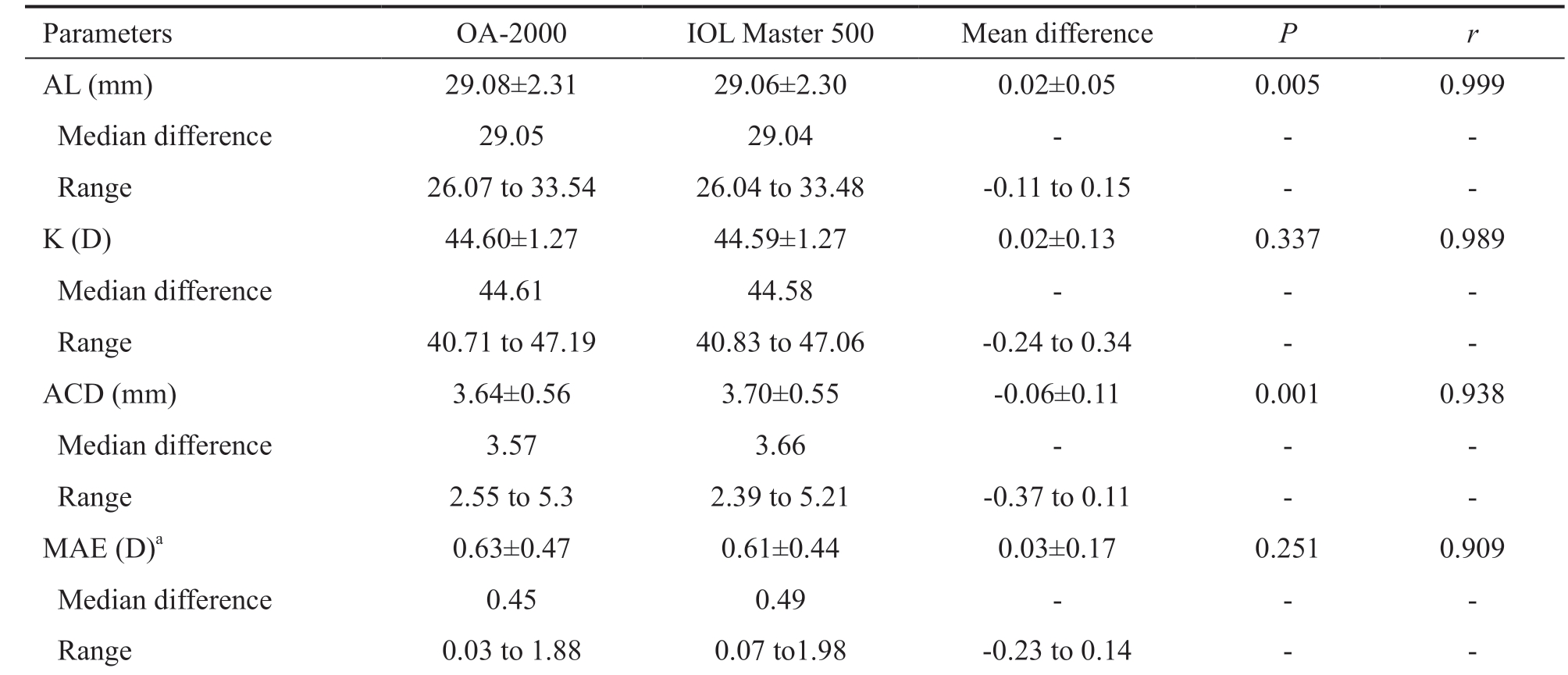
AL: Axial length; K: Keratometry; D: Diopters; ACD: Anterior chamber depth; MAE: Mean absolute error; IOL: Intraocular lens; r: Pearson’s correlation coefficient; aIOL power calculated using SRK-T.
Parameters OA-2000 IOL Master 500 Mean difference P r AL (mm) 29.08±2.31 29.06±2.30 0.02±0.05 0.005 0.999 Median difference 29.05 29.04 - - -Range 26.07 to 33.54 26.04 to 33.48 -0.11 to 0.15 - -K (D) 44.60±1.27 44.59±1.27 0.02±0.13 0.337 0.989 Median difference 44.61 44.58 - - -Range 40.71 to 47.19 40.83 to 47.06 -0.24 to 0.34 - -ACD (mm) 3.64±0.56 3.70±0.55 -0.06±0.11 0.001 0.938 Median difference 3.57 3.66 - - -Range 2.55 to 5.3 2.39 to 5.21 -0.37 to 0.11 - -MAE (D)a 0.63±0.47 0.61±0.44 0.03±0.17 0.251 0.909 Median difference 0.45 0.49 - - -Range 0.03 to 1.88 0.07 to1.98 -0.23 to 0.14 - -
Statistical Analysis Statistical analysis was performed using the SPSS software (version 21.0, IBM, USA). A value of P<0.05 was considered statistically significant. Data obtained from each instruments were compared using the paired t-test.Parson’s correlation was used to determine relationships between groups. The Bland-Altman limits of agreement(LoA) method was used to evaluate agreement between the measurements of the two biometers.
RESULTS
Out of 67 scanned eyes, the AL of 21 eyes with poor visual acuity and dense cataract could not be measured using IOL Master 500, however, 20 of those eyes could be measured using OA-2000. Therefore, the AL measurement failure rate was 31.34% with IOL Master 500 and 1.49% with OA-2000.
The 21 eyes were excluded from the study.
In total, 46 eyes of 36 patients (11 males and 25 females) with a mean age of 57.39±10.74y (range: 33 to 78y) were included.The mean spherical equivalent refraction was -13.40±6.52 D(range: -25 to -6.5 D) and 38 eyes (82.61%) exhibited posterior staphyloma. The mean IOL power was 6.65±5.81 D (range: -4 to 17.5 D). The implanted IOLs included Rayner 920H (n=31),Zeiss 509 (n=8), and L-312 IOLs (n=7).
Table 1 shows the AL, K, ACD and MAE of the two devices.Mean values of the AL, K and ACD were similar. Moreover,strong correlations were found between the AL (r=0.999), K(r=0.989), and ACD (r=0.938) measurements. For the OA-2000, the MAE of the IOL power using the SRK-T formula was 0.63±0.47 D (range: 0.03 to 1.88 D) and for the IOL Master 500, 0.61±0.44 D (range: 0.07 to 1.98 D). There was no significant difference (t=1.164, P=0.251), furthermore,excellent correlation was found (r=0.909).
Figure 1 shows the differences between AL, K, ACD and MAE using Bland-Altman graphs. Good agreements were again observed between the ocular parameter measurements obtained from the two devices.
DISCUSSION
IOL Master 500 applies PCI for AL measurements, later slit illumination for ACD measurements and automated keratometry with six points for corneal curvature estimation[7].It has been in use for several years with high precision and good resolution[7-9]. One limitation of the IOL Master 500 is the failure rate with dense cataract and poor fixation[10]. Previous studies have shown AL measurement failure rates as high as 36.07%[11] and 37.84%[12] using the IOL Master 500. The OA-2000 with longer wavelengths of 1060 nm for measuring the
AL, ACD, LT and CCT, is reduced scattering and attenuation from ocular opacities compared with shorter wavelengths IOL Master 500 of 780 nm semiconductor diode laser[6]. In this study, the AL measurement failure rate was 31.34% with IOL Master 500 and 1.49% with OA-2000. The penetration of the OA-2000 is much better than the IOL Master 500.
Accurate measurements of the AL, ACD and K are crucial to calculating the final IOL power and achieving optimal postoperative results in patients undergoing cataract surgery.Kongsap[7] compared the AL, ACD and K measurements of OA-2000 and IOL Master 500 in normal eyes and found good correlation. In the present study, we compared the AL, ACD,K values and MAE of the two devices in cataract patients with high axial myopia. We also found excellent correlations between the ocular parameters derived from the OA-2000 and the IOL Master 500. Furthermore, good agreement between measurements provided by the two devices were observed,with only small differences in mean values and narrow LoA(AL: -0.08 to 0.13 mm, K: -0.24 to 0.28 D, ACD: -0.28 to 0.15 mm, MAE: -0.29 to 0.36 D). For AL measurements and MAE,there were several cases showed extreme level of differences in Bland-Altman analysis, and all of these cases were presence of posterior staphyloma. Yang et al[13] also demonstrated that the presence of posterior staphyloma was an important factor affecting AL measurements. For myopic eyes with posterior staphyloma, the SS-OCT biometer was expected to be more precise because it allows the fixation status to be evaluated[13].For high myopic patients with cataract, selecting the SRK-T or Haigis formulas can reduce prediction errors[14]. In this study,the SRK-T formula was used. The MAE of the IOL Master 500 was slightly less than that of the OA-2000, however, the difference was not significant (0.61±0.44 D vs 0.63±0.47 D, t=1.164, P=0.251) and excellent correlation was found(r=0.909).
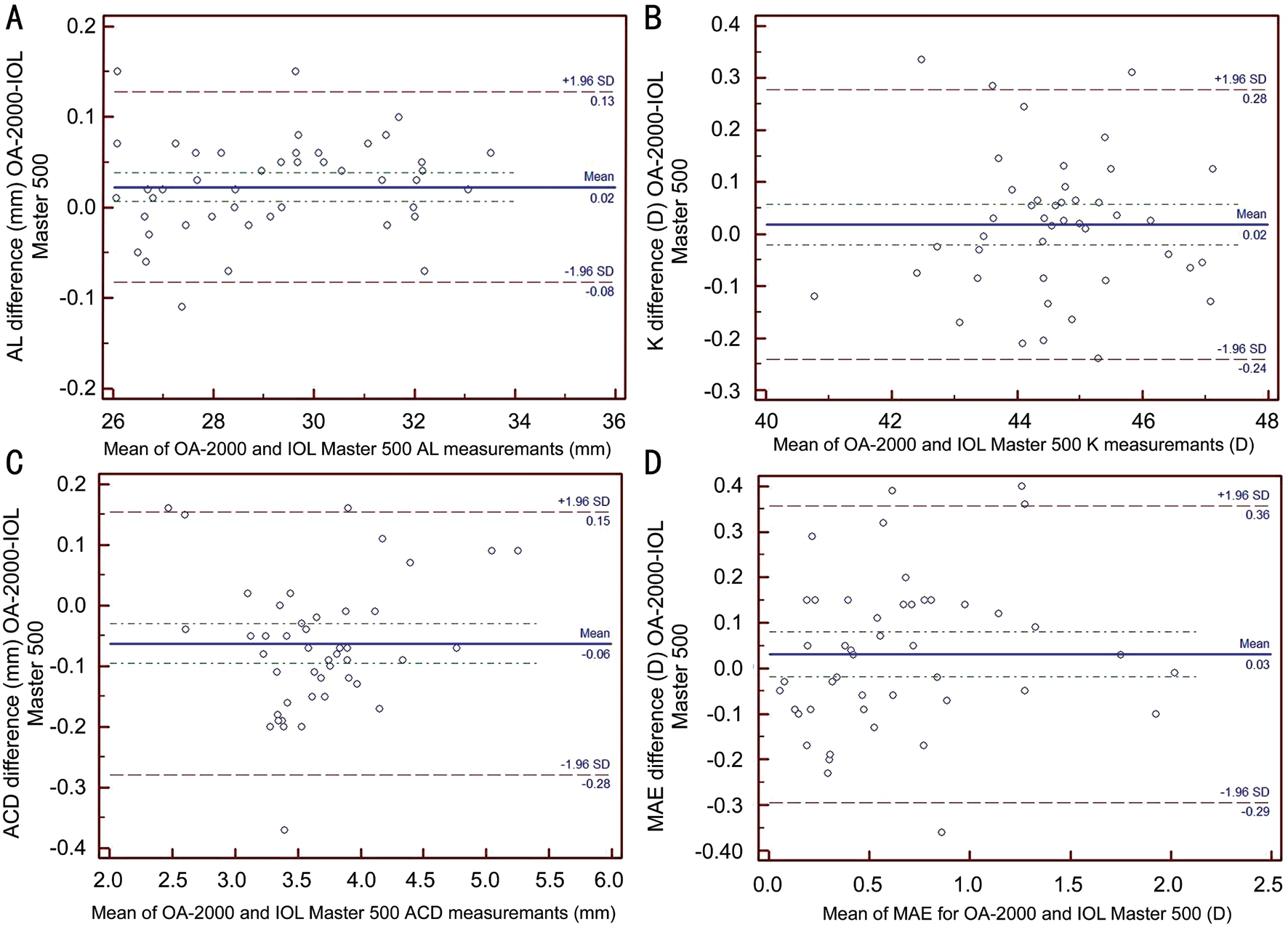
Figure 1 Bland-Altman plots comparing measurements of the OA-2000 and IOL Master 500 A: Axial length (AL); B: Keratometry(K); C: Anterior chamber depth (ACD); D: Mean absolute refractive error (MAE).
This study is not without limitations. First, variability of IOLs with different IOL constants could affect refractive errors.Second, we did not compare various IOL power calculation formulas. In such cases, fourth-generation formulas such as Barrett Universal II have been reported to improve IOL calculations[15].
In conclusion, the biometry measurements and predicted refraction of the OA-2000 biometer correlate well with the IOL Master 500 in cataract patients with high myopia. However,the OA-2000 was notably superior to the IOL Master 500 for AL measurement.
ACKNOWLEDGEMENTS
Foundations: Supported by Natural Science Foundation of Guangdong Province (No.2015A030310504); Guangdong Medical Science and Technology Research Fund (No.B2018142); The Shantou City Science and Technology Project,China (No.170829211930487).
Conflicts of Interest: Du YL, None; Wang G, None; Huang HC, None; Lin LY, None; Jin C, None; Liu LF, None; Liu XR, None; Zhang MZ, None.
1 Yokoi T, Moriyama M, Hayashi K, Shimada N, Ohno-Matsui K.Evaluation of refractive error after cataract surgery in highly myopic eyes.Int Ophthalmol 2013;33(4):343-348.
2 Jeong J, Song H, Lee JK, Chuck RS, Kwon JW. The effect of ocular biometric factors on the accuracy of various IOL power calculation formulas. BMC Ophthalmol 2017;17(1):62.
3 Drexler W, Findl O, Menapace R, Rainer G, Vass C, Hitzenberger CK, Fercher AF. Partial coherence interferometry: a novel approach to biometry in cataract surgery. Am J Ophthalmol 1998;126(4):524-534.
4 Wang W, Miao YX, Savini G, McAlinden C, Chen H, Hu Q, Wang Q,Huang J. Precision of a new ocular biometer in eyes with cataract using swept source optical coherence tomography combined with Placido-disk corneal topography. Sci Rep 2017;7(1):13736.
5 Goebels S, Pattmöller M, Eppig T, Cayless A, Seitz B, Langenbucher A.Comparison of 3 biometry devices in cataract patients. J Cataract Refract Surg 2015;41(11):2387-2393.
6 Reitblat O, Levy A, Kleinmann G, Assia EI. Accuracy of intraocular lens power calculation using three optical biometry measurement devices: the OA-2000, Lenstar-LS900 and IOLMaster-500. Eye (Lond)2018;32(7):1244-1252.
7 Kongsap P. Comparison of a new optical biometer and a standard biometer in cataract patients. Eye Vis (Lond) 2016;3:27.
8 Dong J, Zhang Y, Zhang H, Jia Z, Zhang S, Wang X. Comparison of axial length, anterior chamber depth and intraocular lens power between IOLMaster and ultrasound in normal, long and short eyes. PLoS One 2018;13(3):e0194273.
9 Rohrer K, Frueh BE, Wälti R, Clemetson IA, Tappeiner C, Goldblum D. Comparison and evaluation of ocular biometry using a new noncontact optical low-coherence reflectometer. Ophthalmology 2009;116(11):2087-2092.
10 Hill W, Angeles R, Otani T. Evaluation of a new IOLMaster algorithm to measure axial length. J Cataract Refract Surg 2008;34(6):920-924.
11 McAlinden C, Wang Q, Gao R, Zhao W, Yu A, Li Y, Guo Y, Huang J. Axial length measurement failure rates with biometers using sweptsource optical coherence tomography compared to partial-coherence interferometry and optical low-coherence interferometry. Am J Ophthalmol 2017;173:64-69.
12 McAlinden C, Wang Q, Pesudovs K, Yang X, Bao FJ Yu A, Lin S, Feng Y, Huang J. Axial length measurement failure rates with the IOLMaster and lenstar LS 900 in eyes with cataract. PLoS One 2015;10(6):e0128929.
13 Yang JY, Kim HK, Kim SS. Axial length measurements: Comparison of a new swept-source optical coherence tomography-based biometer and partial coherence interferometry in myopia. J Cataract Refract Surg 2017;43(3):328-332.
14 Zhu XJ, He WW, Du Y, Qian DJ, Dai JH, Lu Y. Intraocular lens power calculation for high myopic eyes with cataract: comparison of three formulas. Zhonghua Yan Ke Za Zhi 2017;53(4):260-265.
15 Melles RB, Holladay JT, Chang WJ. Accuracy of intraocular lens calculation formulas. Ophthalmology 2018;125(2):169-178.