Dear Editor,
I would like to report a case of late traumatic flap dislocation seven years after uncomplicated femtosecond laser-assisted laser in situ keratomileusis (Femto-LASIK).Postoperative laser-assisted laser in situ keratomileusis(LASIK) flap dislocation occurs in approximately 1%-2% of patients, and the greatest risk of non-traumatic flap shift occurs within the first post-operative day after the surgery, presumably as a result of a mechanical trauma[1-3]. However, late flap dislocation, defined as the one taking place more than 1wk after the procedure, is not frequent and has been reported in single case reports or small case series[4-11]. Although flaps are clinically secured in position within a few weeks of LASIK,the full duration of risk is unknown but, to the best of our knowledge, traumatic flap dislocation has been described up to 14y after refractive surgery using mechanical microkeratome[8].Femtosecond flaps represent a significant improvement in morphology and predictability with implications for safety, as the incidence of complications is lower than microkeratome flaps, but despite that, the dislocation of the flap could be a possible complication[12-15].
CASE PRESENTATION
A 21-year-old man had an uneventful Femto-LASIK in 2009 in both eyes. A 100 µm flap with a superior hinge was cut using the IntraLase FS 2 60 kHz Laser System (Abbot Medical Optics, USA), and the laser ablation treatment was performed with the Schwind Esiris excimer laser platform (SCHWIND eye-tech-solutions GmbH, Germany). The pre-LASIK manifest refraction was -2.25 in the right eye and -2.25/-0.50×75 in the left eye. The preoperative pachymetry was 518 µm and 509 µm and the excimer laser ablation was 82 µm and 93 µm,respectively. The patient had a totally normal postoperative evolution with an uncorrected visual acuity (UCVA) after surgery of 20/20 in both eyes.
Six years and 10mo after surgery, the patient had a fall in a rural environment and was accidentally struck in the left eye with an unknown object. Several hours later, he went to the nearest hospital emergency service complaining of pain,photophobia and blurred vision. Slit-lamp examination of the left eye disclosed bruising on the upper eyelid and a complete traumatic corneal flap dislocation with a UCVA of 20/200. The flap was not repositioned. A bandage contact lens was placed and local treatment was started with tobramycin and ofloxacin drops hourly and cyclopentolate hydrochloride drops 4 times a day. The patient was then referred to our clinic, where the Femto-LASIK surgery had been performed.
When he came to our attention, 36h after the trauma, the UCVA was counting fingers and slit-lamp examination revealed a complete flap dislocation with bare stroma exposure.The dislocated flap was crumpled, folded on itself, edematous and whitish and it was found to be held only by a small strand of residual tissue at three o’clock. There was an incised corneal wound outside the flap margin at ten o’clock and significant debris were imbedded in the stroma surface. The rest of the ophthalmic evaluation showed a 2+ conjunctival injection and mild anterior chamber hematic cell and flare without hyphema(Figure 1).
External ocular findings included superior eyelid ecchymosis and a 3 mm skin laceration (Figure 2).
The patient was immediately taken to the operating room where the flap was refloated, irrigated and flattened, with scraping and profuse irrigation with balanced salt solution(BSS) of the stromal bed and the underside of the flap.While repositioning the flap, the interface was irrigated with vancomycin and ceftazidime fortified solution (50 mg/mL). As the flap was fairly movable, it was further secured using 360°interrupted 10.0 nylon sutures to maintain apposition and avoid loss. A bandage contact lens was applied to protect the flap and the patient was dismissed with a regimen of vancomycin and ceftazidime fortified eye drops every 2h daily, dexamethasone 0.1% 5 times a day, and cyclopentolate hydrochloride 3 times a day. Before performing the surgery, a written informed consent was obtained from the patient and all the therapeutic interventions were performed following the Declaration of Helsinki principles.
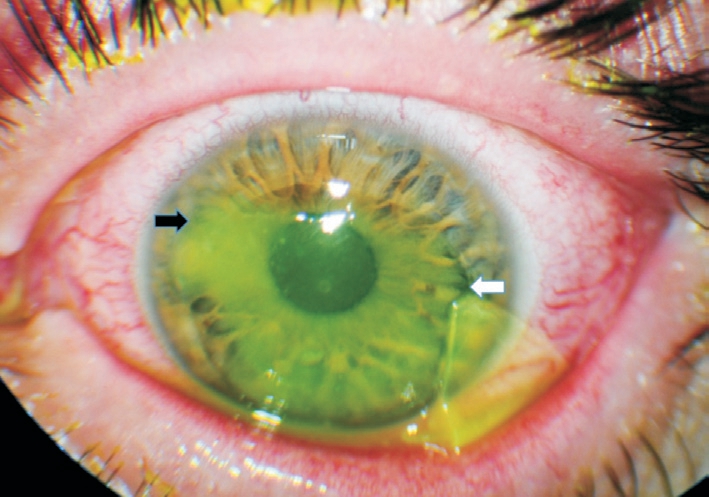
Figure 1 Colour photograph of the dislocated IntraLase flap in the left eye with fluorescein staining of the exposed stroma Note the small strand of residual tissue which held the flap at 3 o’clock(white arrow). The black arrow shows the localization of the incised corneal wound outside the flap margin at 10 o’clock.

Figure 2 Colour photograph of the external ocular findings The black arrow shows the skin laceration.
On postoperative day 1, the visual acuity of the left eye was fingers count. Under slit lamp microscopy the flap edges were well positioned and the interface was clean, but the corneal stroma was still edematous and superior folds were observed. Three days later (post trauma day 6), there was a clinical improvement of the edema and folds, with UCVA reaching 20/200. Vancomycin and ceftazidime fortified eye drops were reduced to 6 times a day and cyclopentolate hydrochloride twice a day, keeping the rest of the treatment the same. The bandage contact lens was replaced with a new one after one week and then replaced every 7d. On postoperative day 9, visual acuity remained 20/200, vancomycin and ceftazidime fortified eye drops were decreased to 4 times a day, cyclopentolate hydrochloride was discontinued and dexamethasone 0.1% was decreased to 3 times daily. Three weeks after the injury, the flap gained transparency, no folds were noticed and the UCVA improved to 20/125. Topical antibiotics were discontinued and dexamethasone 0.1% was reduced in a tapering dose. At one month follow up, the use of bandage contact lens was dismissed. On the postoperative week 10, UCVA was 20/63. Six corneal sutures were removed with the remainder progressively removed at the subsequent visits (Figure 3).
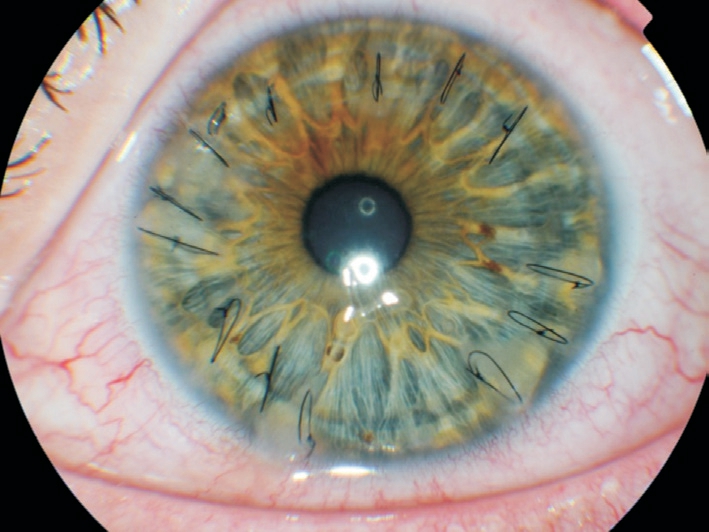
Figure 3 Colour photograph showing the sutures at postoperative week 10.
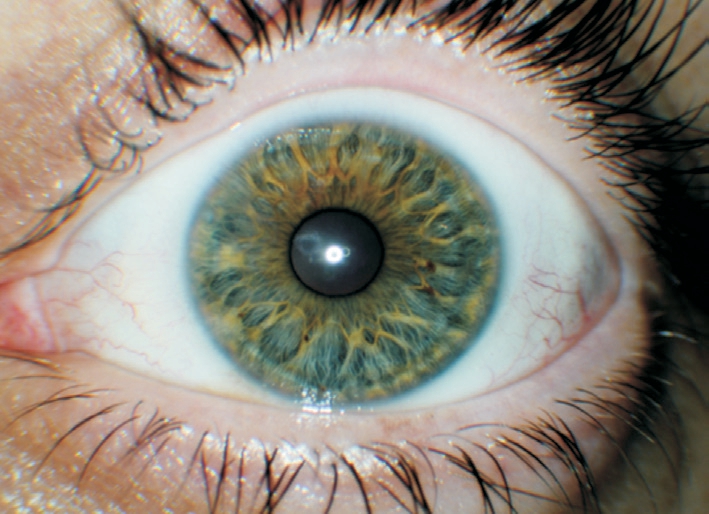
Figure 4 Colour photograph showing the appearance of the cornea at postoperative month 9.

Figure 5 Slit lamp view of the cornea showing radial peripheral opacities (arrows).
Three and a half months postoperatively, the UCVA was 20/50,with a refraction of +1.50/-3.25×175. At postoperative month 6, UCVA was 20/32, and the refraction was plano +0.00/-1.50×35. At the last examination 9mo postoperatively, the flap was perfectly centred with central transparency, slight peripheral lineal opacities, clear interface and no signs of epithelial ingrowth (Figures 4, 5).
The UCVA was 20/20 with a refraction of +0.00/-0.50×55.Corneal topography showed a regular central corneal profile with peripheral irregular elevation of the anterior surface in correspondence with an incised corneal scar outside the flap margin at ten o’clock (Figure 6).

Figure 6 Final corneal topography.
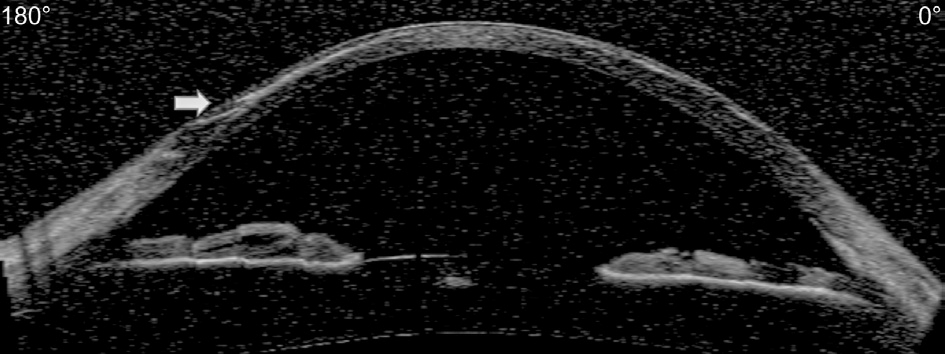
Figure 7 Anterior segment optical coherence tomography (Visante OCT) shows focal interface hyperreflectivity at the peripheral nasal margin of the flap, where the incised corneal wound was(arrow).
A linear interface hyper-reflectivity was also noted on anterior segment optical coherence tomography at the same location(Figure 7).
DISCUSSION
LASIK is characterized by the generation of a corneal flap that represents a potential plane of weakness in the cornea, where shearing forces can produce the displacement of the flap. The absence of scarring in the interface between flap and stromal bed is essential to obtain optical clarity postoperatively, but also permits an easy lifting of the flap if needed, because the healing occurs exclusively at the edge of the flap with minimal central extension[16-17]. If the resistance of the adhesion at the flap margin can be bridged, the whole flap can be easily lifted.The early displacement of the flap after LASIK (within 48h)is a well-known phenomenon and occurs in approximately 1%to 2% of cases[18]. Several case reports have been published on late (postoperative week 1 or later) presentation of traumatic flap dislocation with time from surgery to flap dislocation ranging from 10d to 14y[4,8]. Femto-LASIK flaps represent significant improvement in morphology and predictability versus microkeratome flaps, especially when related to safety.Displaced flaps have been reported both with mechanical microkeratomes and femtosecond lasers, but the incidence of this complication should theoretically be less with the use of femtosecond flaps due to the architecture of the side-cut angle.In addition, it has been demonstrated that femtosecond lasers produce a greater degree of stromal inflammation without any increase in apoptosis in the early postoperatively period that could lead to a stronger flap adhesion[19-20].
Flap dislocation or subluxation should be considered as an emergency. The immediate repositioning is critical to prevent possible complications such as fixed folds, epithelial ingrowth and optical aberrations[21]. The flap should be totally or partially lifted examining carefully the interface for the presence of foreign bodies, epithelial cells or any debris,using BSS to irrigate and refloat the flap. Epithelial ingrowth is usually managed with mechanical debridement and aggressive scraping before reposition of the flap. As previous reported by several authors, stretching the corneal flap[22-23]and additional denudation of the surface epithelium[8,22] are indicated to manage the presence of flap striae and to facilitate the re-approximation of flap edges. In the event that a flap is completely detached from its bed, the repositioning in the proper orientation could be quite complex, with improper reposition of the flap resulting in irregular astigmatism and optical aberrations. Suturing the flap to the corneal stroma may become necessary at times to secure the flap in place,even with the aid of fibrin glue, but is not mandatory[8,24]. In our case, we found it convenient to stabilize the flap with 10.0 nylon sutures because the flap was not only dislocated but also slightly traumatized and quite movable. The use of contact lens alone would not have been sufficient to stabilize the flap and to support the healing. Lastly, in the case of a lost flap,the epithelium is simply allowed to heal with unpredictable refractive outcomes[25].
The previous cases reported in the literature indicate that corneal flaps remain susceptible to traumatic dislocation as late as 14y after LASIK[8]. The case we reported in this letter indicates that even if flaps cut with the femtosecond laser are less prone to dislocate than blade-cut flap, corneal flaps remain susceptible to trauma as late as 7y after uneventful Femto-LASIK.
CONCLUSION
To the best of our knowledge, this case represents the longest documented interval from femtosecond laser-assisted LASIK surgery to traumatic flap dislocation and demonstrates that appropriate management can lead to an excellent visual outcome even in late-onset severely traumatized dislocated flaps. Flap dislocation should be regarded as an emergency.
The discussion of this potential complication should be included in the informed consent process. For patients who are predisposed to eye trauma, the refractive surgeon should recommend the use of protective eyewear indefinitely after lamellar corneal surgery or inform of alternative refractive surgical options like flap-less procedures such as photo refractive keratectomy or small incision lenticule extraction to correct their ametropia.
ACKNOWLEDGEMENTS
Conflicts of Interest: Alvarez MT, None; Montesel A, None;Bataille L, None.
1 Lin RT, Maloney RK. Flap complications associated with lamellar refractive surgery. Am J Ophthalmol 1999;127(2):129-136.
2 Stulting RD, Carr JD, Thompson KP, Waring GO 3rd, Wiley WM,Walker JG. Complications of laser in situ keratomileusis for the correction of myopia. Ophthalmology 1999;106(1):13-20.
3 Sugar A, Rapuano CJ, Culbertson WW, Huang D, Varley GA, Agapitos PJ, de Luise VP, Koch DD. Laser in situ keratomileusis for myopia and astigmatism: safety and efficacy: a report by the American Academy of Ophthalmology. Ophthalmology 2002;109(1):175-187.
4 Melki SA, Talamo JH, Demetriades AM, Jabbur NS, Essepian JP, O’Brien TP, Azar DT. Late traumatic dislocation of laser in situ keratomileusis corneal flaps. Ophthalmology 2000;107(12):2136-2139.
5 Jin GJ, Merkley KH. Laceration and partial dislocation of LASIK flaps 7 and 4 years postoperatively with 20/20 visual acuity after repair. J Refract Surg 2006;22(9):904-905.
6 Landau D, Levy J, Solomon A, Lifshitz T, Orucov F, Strassman E, Frucht-Pery J. Traumatic corneal flap dislocation one to six years after LASIK in nine eyes with a favorable outcome. J Refract Surg 2006;22(9):884-889.
7 Tsai TH, Peng KL, Lin CJ. Traumatic corneal flap displacement after laser in situ keratomileusis (LASIK). Int Med Case Rep J 2017;10:143-148.
8 Holt DG, Sikder S, Mifflin MD. Surgical management of traumatic LASIK flap dislocation with macrostriae and epithelial ingrowth 14 years postoperatively. J Cataract Refract Surg 2012;38(2):357-361.
9 Xiao JH, Jiang CH, Zhang MN, Jiang H, Li SY, Zhang Y. When case report became case series: 45 cases of late traumatic flap complications after laser-assisted in situ keratomileusis and review of Chinese literature.Br J Ophthalmol 2014;98(9):1282-1286.
10 Khoueir Z, Haddad NM, Saad A, Chelala E, Warrak E. Traumatic flap dislocation 10 years after LASIK. Case report and literature review. J Fr Ophtalmol 2013;36(1):82-86.
11 Galvis V, Tello A, Guerra AR, Rey JJ, Camacho PA. Risk factors and visual results in cases of LASIK flap repositioning due to folds or dislocation: case series and literature review. Int Ophthalmol 2014;34(1):19-26.
12 Farjo AA, Sugar A, Schallhorn SC, Majmudar PA, Tanzer DJ,Trattler WB, Cason JB, Donaldson KE, Kymionis GD. Femtosecond lasers for LASIK flap creation: a report by the American Academy of Ophthalmology. Ophthalmology 2013;120(3):e5-e20.
13 Santhiago MR, Kara-Junior N, Waring GO 4th. Microkeratome versus femtosecond flaps: accuracy and complications. Curr Opin Ophthalmol 2014;25(4):270-274.
14 Moshirfar M, Gardiner JP, Schliesser JA, Espandar L, Feiz V, Mifflin MD, Chang JC. Laser in situ keratomileusis flap complications using mechanical microkeratome versus femtosecond laser: retrospective comparison. J Cataract Refract Surg 2010;36(11):1925-1933.
15 dos Santos AM, Torricelli AA, Marino GK, Garcia R, Netto MV,Bechara SJ, Wilson SE. Femtosecond laser-assisted LASIK flap complications. J Refract Surg 2016;32(1):52-59.
16 Rumelt S, Cohen I, Skandarani P, Delarea Y, Ben Shaul Y, Rehany U. Ultrastructure of the lamellar corneal wound after laser in situ keratomileusis in human eye. J Cataract Refract Surg 2001;27(8):1323-1327.
17 Pérez-Santonja JJ, Linna TU, Tervo KM, Sakla HF, Alió y Sanz JL,Tervo TM. Corneal wound healing after laser in situ keratomileusis in rabbits. J Refract Surg 1998;14(6):602-609.
18 Clare G, Moore TC, Grills C, Leccisotti A, Moore JE, Schallhorn S. Early flap displacement after LASIK. Ophthalmology 2011;118(9):1760-1765.
19 Kim JY, Kim MJ, Kim TI, Choi HJ, Pak JH, Tchah H. A femtosecond laser creates a stronger flap than a mechanical microkeratome. Invest Ophthalmol Vis Sci 2006;47(2):599-604.
20 Javaloy J, Vidal MT, Abdelrahman AM, Artola A, Alió JL. Confocal microscopy comparison of intralase femtosecond laser and Moria M2 microkeratome in LASIK. J Refract Surg 2007;23(2):178-187.
21 Estopinal CB, Mian SI. LASIK flap: postoperative complications. Int Ophthalmol Clin 2016;56(2):67-81.
22 Tumbocon JA, Paul R, Slomovic A, Rootman DS. Late traumatic displacement of laser in situ keratomileusis flaps. Cornea 2003;22(1):66-69.
23 Pereira Cda R, Narvaez J, King JA, Seery LS, Gimbel HV. Late-onset traumatic dislocation with central tissue loss of laser in situ keratomileusis flap. Cornea 2006;25(9):1107-1110.
24 Yeh DL, Bushley DM, Kim T. Treatment of traumatic LASIK flap dislocation and epithelial ingrowth with fibrin glue. Am J Ophthalmol 2006;141(5):960-962.
25 Sridhar MS, Rapuano CJ, Cohen EJ. Accidental self-removal of a flap: a rare complication of laser in situ keratomileusis surgery. Am J Ophthalmol 2001;132(5):780-782.