Dear Editor,
I write to present one case report of a patient suffered the panophthalmitis caused by non-metallic foreign body with no etiologic agent and recovered quickly by phacoemulsification and vitrectomy with silicone oil tamponade.Ocular trauma remains a major cause of blindness, particularly in the working-age population. Intraocular foreign body(IOFB), frequently accompany penetrating ocular injuries and can lead to increased ocular morbidity[1]. IOFB can cause several ocular damages such as retinal break, branch retinal vein occlusion, choroidal neovascularization, siderosis bulbi,chalcosis and endophthalmitis[2-4]. The most important rule in treating patients with IOFB is that the primary goal of the intervention, while typically including foreign body removal,is comprehensive anatomical reconstruction of the injured eye so that the best possible visual outcome can be achieved[5]. To our knowledge, no previous cases of presumed iridocyclitis developed to chronic panophthalmitis caused by a small nonmetallic foreign body in the posterior segment have been reported. This study was approved by the research Ethics Committee of the Second Affiliated Hospital of Zhejiang University School of Medicine. Due to the retrospective nature of this study, the inform consent from individual patient was waived by IRB in this study.
A 60-year-old man complained for his eye redness and pain for the initial visit. He was diagnosed with iridocyclitis for the ciliary congestion and keratic precipitates. Then he took the pred forte and pranopulin prescribed by the doctor. Three weeks later, his eyesight dropped to 2/100. A ciliary-like foreign body was found in the vitreous cavity (Figure 1A).Conjunctiva and sclera congestion were seen clearly from slit lamp examination (Figure 2A). No retinal damages were seen from the fundus image (Figure 2B). Then he recalled he was hit by the branch one month ago. He was quickly referred to a retina specialist and made a reservation for magnetic resonance imaging (MRI). Though the MRI did not show any foreign bodies, the progression of the ocular damage was still seen.The sclera necrosis was disclosing and the vitreous body was blurry. Lots of small bright spots were showed in the vitreous body by B-scan, which consisted with necrotizing scleritis and panophthalmitis. Nothing could cause these damages except for the foreign body in the vitreous. So, we arranged the phacoemulsification and pars plana vitrectomy for him.In the operation, we found that the sclera was melting and the uvea pigment was evident (Figure 2C). Furthermore, the retinal vessels were occluded (Figure 2D). The cataract was extracted by phacoemulsification. Then anterior vitreous body before the foreign body was carefully removed. Then the IOFB was taken out from the sclerotomy site with internal limiting membrane forceps. It looked like broken eyelash and was 1.2 mm length (Figure 1C). After the turbid vitreous body was removed, silicone oil tamponade was done. The best corrected visual acuity (BCVA) of the patient improved to 6/10 one month after the surgery. There was no any active inflammation in the anterior segment (Figure 3A-3B). However, the pigment of the uvea was still seen on the sclera (Figure 3A). We could confirm the reperfusion of the retinal vessels from the fundus image and fluorescein angiography (Figure 3C-3D).
Panophthalmitis is a relatively rare but very serious progressive and devastating ocular infection usually leading to enucleation[6].Baccillus cereus is well known for inducing endophthalmitis following traumatic injury[7]. Also it is reported to cause panophthalmitis after double-penetrating ocular injury[8].
However, it was chronic panophthalmitis caused by a foreign body for our patient. He had not developed to panophthalmitis after hit by the non-metallic foreign body until one month later. It can not be acute bacterial pathogens. Interestingly,the bacterial cultures of the aqueous humor and vitreous were both negative. As reported, the most common bacteria were Staphylococcus and Streptococcus[9-10]. Streptococcus mitis can cause severe occlusive vasculitis[11]. Due to the blurry vitreous and occlusive retinal vasculitis of this patient, the pathogen might be the Streptococcus mitis. The possible pathophysiological mechanism of panophthalmitis with broken eyelash remains unclear. Since the patient suffered from the delayed leukocytoclastic retinal vasculitis, chronic nongranulomatous choroiditis and scleral necrosis. It might be an immune-mediated type III hypersensitivity reaction to the eyelash. Emergent pars plana vitrectomy and silicone oil tamponade seemed to stop the exacerbation. It seemed that panretinal photocoagulation was not necessary since reperfusion of the retinal vasculature could be seen one month after surgery from fluorescein angiography. The patient recovered very quickly.

Figure 1 Non-metallic foreign body in the posterior segment A: The fundus image of the patient one month after the hit by the branch. The arrow indicated the foreign body in the vitreous cavity. B: The foreign body during the surgery. The arrow indicated the foreign body in the vitreous cavity. C: The foreign body was about 1.2 mm length.

Figure 2 Images of ocular anterior segment and fundus A: The arrow showed the sclera necrosis before the surgery; B: The fundus image before surgery; C: The arrow showed that sclera necrosis was seen around the eyeball during the surgery; D: The arrow showed the retinal vessels were occluded during the surgery.
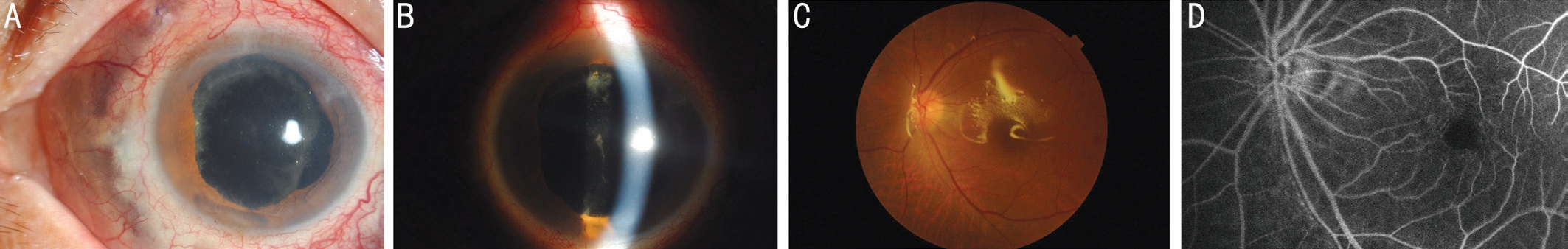
Figure 3 One month after phacovitrectomy with silicone oil tamponade A: Anterior segment image of the patient under diffused light. The necrotizing of the sclera ceased. The choroidal pigment was still seen from the sclera. B: Anterior segment image of the patient under slit light.The posterior capsule opacification was found clearly. C: The fundus image of the patient. All the vessels were infused with blood flow. D: The fluorescein angiography image of the fundus. Reperfusion of the retinal vessels was seen.
MRI is superior to computed tomography (CT) in detecting the smallest pieces of wood. However, it depends on the types and sizes of the foreign body. For this patient, there was no positive finding in MRI. We found it by fundoscopy with dilated pupil.Sometimes the fundamental examination worked when MRI and CT showed negative results. For the small IOFB, it was difficult to remove it completely without any damage. With internal limiting membrane forceps, we successfully took it out with its integrity.Non-metallic foreign body could induce masked iridocyclitis and chronic panophthalmitis. Emergent surgery could halt the deterioration and accelerate the rehabilitation process.
ACKNOWLEDGEMENTS
Authors’ contributions: Weng Y and Ma J performed the surgery and wrote the manuscript. Zhang L and Jin HY performed the literature review for similar topics. Fang XY revised the article. All authors have read and approved the final manuscript.
Foundations: Supported by Natural Science Foundation of China (No.81571819; No.81500766); the Natural Science Foundation of Zhejiang Province, China (No.LY14H120004).
Conflicts of Interest: Weng Y, None; Ma J, None; Zhang L,
None; Jin HY, None; Fang XY, None.
1 Obuchowska I, Sidorowicz A, Napora KJ, Mariak Z. Clinical characteristics of penetrating ocular injuries with intraocular foreign body.Part II. Diagnostics and treatment. Klin Oczna 2010;112(1-3):77-81.
2 Bypareddy R, Sagar P, Chawla R, Temkar S. Intraocular metallic foreign body causing branch retinal vein occlusion. BMJ Case Rep 2016;2016:bcr2016214745.
3 Fernández-López E, Desco-Esteban MC, Fandiño-López A, Hernández-Díaz M, Navea A. Choroidal neovascularization after intraocular foreign body. Clin Ophthalmol 2014;8:945-948.
4. Loporchio D, Mukkamala L, Gorukanti K, Zarbin M, Langer P, Bhagat N. Intraocular foreign bodies: a review. Surv Ophthalmol 2016;61(5):582-596.
5 Mester V, Kuhn F. Intraocular foreign bodies. Ophthalmol Clin North Am 2002;15(2):235-242.
6 Davenport R, Smith C. Panophthalmitis due to an organism of the Bacillus subtilis group. Br J Ophthalmol 1952;36(7):389-392.
7 David DB, Kirkby GR, Noble BA. Bacillus cereus endophthalmitis. Br J Ophthalmol 1994;78(7):577-580.
8 Zheng X, Kodama T, Ohashi Y. Eyeball luxation in Bacillus cereusinduced panophthalmitis following a double-penetrating ocular injury. Jpn J Ophthalmol 2008;52(5):419-421.
9 Assaad D, Wong D, Mikhail M, Tawfik S, Altomare F, Berger A,Chow D, Giavedoni L. Bacterial endophthalmitis: 10-year review of the culture and sensitivity patterns of bacterial isolates. Can J Ophthalmol 2015;50(6):433-437.
10 Leung EH, Kuriyan AE, Flynn HW Jr, Miller D, Huang LC. Persistently vitreous Culture-Positive exogenous bacterial endophthalmitis. Am J Ophthalmol 2016;165:16-22.
11 Baxter KR, Robinson JE, Ruby AJ. Occlusive vasculitis due to hyperacute Streptococcus mitis endophthalmitis after intravitreal ranibizumab. Retin Cases Brief Rep 2015;9(3):201-204.