
Citation:
Zhang JQ, Zou XY, Zheng DY,
Chen WR, Sun A, Luo LX. Effect of lens constants
optimization on the accuracy of intraocular lens power calculation formulas for
highly myopic eyes. Int
J Ophthalmol 2019;12(6):943-948
DOI:10.18240/ijo.2019.06.10
·Clinical Research·
Effect
of lens constants optimization on the accuracy of intraocular lens power
calculation formulas for highly myopic eyes
Jia-Qing Zhang, Xu-Yuan Zou, Dan-Ying Zheng, Wei-Rong
Chen, Ao Sun, Li-Xia Luo
State Key
Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-sen
University, Guangzhou 510060, Guangdong Province, China
Correspondence
to: Li-Xia Luo.
State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-sen
University, Guangzhou 510060, Guangdong Province, China.
luolixia@mail.sysu.edu.cn
Received:
Abstract
AIM: To evaluate the effect of different lens constant optimization methods
on the accuracy of intraocular lens (IOL) power calculation formulas for highly
myopic eyes.
METHODS: This study comprised 108 eyes of 94 consecutive
patients with axial length (AL) over
RESULTS: Optimized constants could significantly reduce the
MAE of SRK/T, Hoffer Q, and Holladay 1 formulas compared with manufacturer’s
lens constant, whereas the percentage of eyes with IOL prediction errors within
±0.25, ±0.50, and ±1.0 D had no statistically significant differences.
Optimized lens constant for long eyes alone showed non-significant refractive
advantages over the ULIB constant. Barrett Universal II formula and formulas
with AL adjustment showed significantly higher accuracy in highly myopic eyes (P<0.001).
CONCLUSION: Lens constant optimization for the subset of long eyes reduces the
refractive error only to a limited extent for highly myopic eyes.
KEYWORDS: high myopia; cataract; intraocular
lens power; lens constant optimization; prediction error
DOI:10.18240/ijo.2019.06.10
Citation: Zhang JQ, Zou XY, Zheng DY, Chen WR, Sun A, Luo LX. Effect of lens constants optimization on the accuracy of
intraocular lens power calculation formulas for highly myopic eyes. Int J Ophthalmol
2019;12(6):943-948
Outline
High myopia
has become a global public health issue with its notably increased prevalence,
especially in Asia[1]. Increasing number of
patients with cataracts have eyes with an axial length (AL) greater than
Some
approaches were proposed to reduce prediction error and improve visual quality
for highly myopic eyes, including targeting a moderate amount of myopia, using
new generation of formulas, optimizing lens constant, and adjusting the AL as
Wang-Koch recommended[4-5]. Lens
constant optimization and Wang-Koch AL adjustment are methods that can
effectively eliminate the systematic prediction error of IOL formulas. Whether
there is a need to optimize lens constant for atypical eyes is still
controversial[6]. Will optimizing lens constant
using data only from the subset of patients with long eyes further improve
refractive outcomes for highly myopic eyes, compared with that using data from
all eyes? We present a comparison of IOL power calculation formulas using
different lens constants in eyes with AL longer than
Ethical
Approval All procedures adhered to the tenets
of the Declaration of Helsinki of the World Medical Association. Ethical
approval was provided by the Ethics Committee of Zhongshan Ophthalmic Center
(2018KYPJ101). Informed consent was waived due to the retrospective nature of
the study.
Patient
Selection Data from consecutive patients
undergoing uneventful phacoemulsification cataract surgery and in-the-bag IOL
implantation of 1-piece hydrophilic acrylic IOLs (920H, Rayner, Hove, UK) by
the surgeons (Zheng DY and Chen WR) from September 2016 to March 2018 were
collected and reviewed. Inclusion criteria were restricted to eyes with AL
greater than
Data
Collection Patients’ basic information and
preoperative biometric data, including AL, anterior chamber depth (ACD),
keratometry values, data of surgery, and IOL power inserted, were extracted
from electronic medical records. The IOL power and stable postoperative
spherical equivalent (SE) were entered into the IOLMaster device, and a
built-in optimization program provided optimized lens constants. Lens constants
for long eyes were optimized following the steps described in the IOLMaster
manual in detail. The manufacturer’s constants were derived from the A-constant
and ACD-constant provided by the lens manufacturer[7-8]. User Group for Laser Interference Biometry (ULIB)
constants, optimized based on comprehensive data from multiple surgical
centers, were downloaded from the website (www.ocusoft.de/ulib/c1.html) on
April 29, 2018[9]. The SRK/T[10],
Hoffer Q[11], Holladay 1[12],
and Haigis[7] formulas using different lens
constants were evaluated. Results were compared with Barrett Universal II
formula[13], original Wang-Koch AL
adjustment method[4], and modified Wang-Koch AL
adjustment method[5]. The predicted postoperative
SEs were recalculated based on the actual IOL power implanted.
Evaluation
of Parameters The following results were
evaluated: 1) mean arithmetic SE prediction error (ME). ME is calculated as the
mean difference between the predicted and actual postoperative refractive SE. A
negative value significantly different from zero represents a more myopic
outcome than the predicted one, whereas a positive error indicates more
hyperopic results; 2) mean and median absolute SE prediction error (MAE and
MedAE), which are defined as the mean and median of the absolute differences
between formula-predicted values and actual refractive outcomes; 3) percentage
of eyes with IOL prediction error within ±0.25, ±0.50, and ±1.0 D of target
refraction. A formula that is associated with a higher percentage of prediction
errors within a certain range indicates greater accuracy.
Statistical
Analysis Kolmogorov-Smirnov test was used to
determine whether the data were normally distributed. The one-sample t-test
or Wilcoxon signed rank test was used to determine whether the mean arithmetic
error was significantly different from zero across the constants used.
Refractive outcomes obtained using manufacturer’s lens constant, ULIB constant,
and optimized constant for long eyes were compared. The nonparametric method,
Friedman test, was used to compare MAE performance among constants. The Cochran
Q test was performed to compare the percentages of eyes with IOL
prediction error within ±0.25, ±0.50, and ±1.0 D of target refraction.
Statistical analysis was performed using SPSS software (version 23.0; IBM,
Chicago, IL, USA). The Bonferroni correction was performed for multiple
comparisons. A P value of less than 0.05 was considered statistically
significant.
Figure 1
shows the flow chart of the study. A total of 108 eyes of 94 patients with AL
longer than
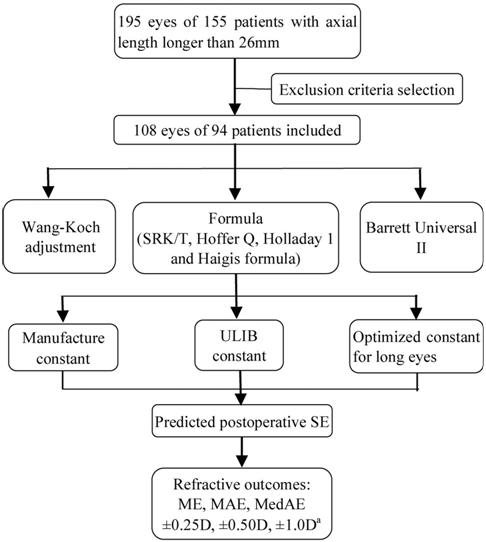
Figure 1
Flow diagram ULIB: User Group for Laser
Interference Biometry; SE: Spherical equivalent; ME: Mean arithmetic SE
prediction error; MAE: Mean absolute SE prediction error; MedAE: Median
absolute SE prediction error. aPercentage of refractions within
±0.25 D, ±0.50 D or ±1.0 D of prediction.
Table 1
Preoperative demographic characteristics of sample included
|
Parameters |
Mean±SD |
Range |
|
Age (y) |
57.46±12.56 |
22-77 |
|
AL (mm) |
29.15±2.31 |
26.06-36.37 |
|
SimK (D) |
43.85±1.62 |
40.32-49.24 |
|
ACD (mm) |
3.51±0.39 |
2.42-4.34 |
|
IOL power (D) |
7.94±5.35 |
-7-18.5 |
|
Corneal astigmatism (D) |
1.22±0.73 |
0.2-3.38 |
SD: Standard
deviation; SimK: Simulated keratometry; D: Diopter; ACD: Anterior chamber
depth; IOL: Intraocular lens.
Table 2 Lens
constants used for Rayner 920H in the study
|
Parameters |
Manufacture const |
ULIB const |
Optimized const for long eyes |
|
SRK/T A const |
118.0 |
118.3 |
119.7 |
|
Haigis |
|
|
|
|
a0 |
1.283 |
1.02 |
2.217 |
|
a1 |
0.4 |
0.4 |
0.4 |
|
a2 |
0.1 |
0.1 |
0.1 |
|
Hoffer Q pACD |
4.97 |
5.21 |
6.75 |
|
Holladay 1 SF |
1.22 |
1.41 |
2.96 |
Const: Lens
constant; ULIB: User Group for Laser Interference Biometry method.
Figure 2
shows the boxplots of MAE of formulas with different lens constant. Compared
with manufacturer’s lens constant, the ULIB constant significantly reduced the
MAE of SRK/T, Hoffer Q, and Holladay 1 formulas, and the optimized lens
constant for long eyes significantly reduced the MAE of Hoffer Q and Holladay 1
formulas. No statistically significant differences were observed between the
ULIB constant and optimized lens constant for long eyes. The MAE of Haigis
formula with ULIB constant was significantly higher than that for the other
constants (P<0.0001).
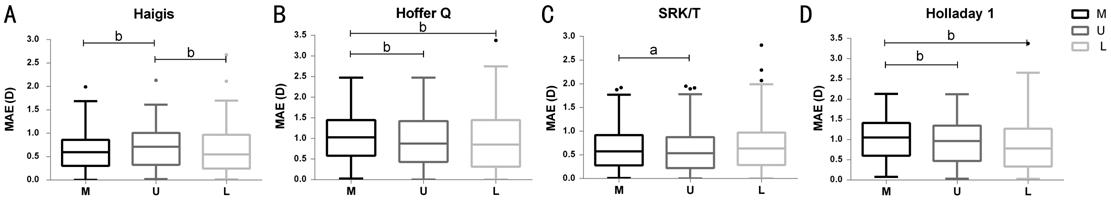
Figure 2
Boxplot of mean absolute prediction error with IOL calculation formulas MAE: Mean absolute SE prediction
error; M: Manufacturer’s lens constants; U: User Group for Laser Interference
Biometry method; L: Optimized lens constants for long eyes. aP<0.01;
bP<0.001.
Table 3
summarizes postoperative refractive error of IOL calculation formulas. Without
AL adjustments, formulas combined with manufacturer’s lens constant and ULIB
constant had a positive arithmetic mean error, different from zero with
statistically significance. There were no statistically significant differences
between percentages of eyes within certain prediction errors of formulas
combined with different constants without AL adjustments. Both the ME of
Barrett Universal II formula and formulas with original Wang-Koch AL adjustment
were equal to zero statistically. The ME of formulas with modified Wang-Koch AL
adjustment had a positive arithmetic mean error, statistically significantly
different from zero. Barrett Universal II formula and formulas adjusted with
both Wang-Koch methods had the significantly lower MAE and the higher
percentage of prediction error within certain range than formulas without AL
adjustment (P<0.001). No significant difference was found between
Barrett Universal II formula and formulas with original or modified Wang-Koch
AL adjustment in terms of MAE and percentages of eyes within certain prediction
errors.
Table 3
Postoperative refractive error of IOLs formulas
|
Formulas |
ME |
MAE |
SD |
MedAE |
Max Error |
±0.25 D (%)a |
±0.50 D (%)a |
±1.0 D (%)a |
|
Haigis (M) |
0.51b |
0.64 |
0.45 |
0.59 |
1.99 |
21.30 |
42.59 |
77.78 |
|
Haigis (U) |
0.64b |
0.71 |
0.44 |
0.71 |
2.13 |
22.22 |
34.26 |
75 |
|
Haigis (L) |
0 |
0.65 |
0.51 |
0.55 |
2.68 |
25.00 |
46.30 |
76.85 |
|
Hoffer Q (M) |
1.01b |
1.07 |
0.65 |
1.03 |
2.48 |
12.96 |
22.22 |
49.07 |
|
Hoffer Q (U) |
0.89b |
0.99 |
0.67 |
0.88 |
2.48 |
13.89 |
27.78 |
55.56 |
|
Hoffer Q (L) |
0 |
0.99 |
0.76 |
0.85 |
3.38 |
22.22 |
33.33 |
58.33 |
|
Holladay 1 (M) |
0.97b |
1.03 |
0.53 |
1.05 |
2.13 |
9.26 |
19.44 |
48.15 |
|
Holladay 1 (U) |
0.88b |
0.95 |
0.56 |
0.97 |
2.12 |
12.96 |
25.93 |
50.93 |
|
Holladay 1 (L) |
0 |
0.89 |
0.65 |
0.78 |
3.38 |
19.44 |
32.41 |
59.26 |
|
SRK/T (M) |
0.51b |
0.68 |
0.49 |
0.57 |
1.92 |
22.22 |
43.52 |
78.70 |
|
SRK/T (U) |
0.42b |
0.64 |
0.51 |
0.54 |
1.95 |
26.85 |
48.15 |
79.63 |
|
SRK/T (L) |
0 |
0.72 |
0.56 |
0.64 |
2.82 |
21.30 |
40.74 |
76.85 |
|
Holladay 1-AL |
-0.01 |
0.40 |
0.34 |
0.34 |
2.09 |
42.59 |
74.07 |
96.30 |
|
Holladay 1-AL2 |
0.14b |
0.36 |
0.29 |
0.34 |
1.58 |
43.88 |
75.51 |
96.94 |
|
SRK/T-AL |
-0.10 |
0.45 |
0.38 |
0.37 |
1.90 |
39.81 |
67.59 |
93.52 |
|
SRK/T-AL2 |
0.22b |
0.41 |
0.31 |
0.33 |
1.49 |
32.94 |
69.41 |
95.29 |
|
Barrett Universal II |
0.07 |
0.42 |
0.39 |
0.33 |
2.58 |
38.53 |
71.56 |
94.50 |
ME: Mean
refractive prediction error; MAE: Mean absolute refractive prediction error;
SD: Standard deviation of the refractive prediction error; MedAE: Median
refractive absolute error; Max error: Maximum refractive prediction error; M:
Manufacturer’s lens constants; U: User Group for Laser Interference Biometry
method; L: Optimized lens constants for long eyes; AL: Original Wang-Koch axial
length adjustments; Holladay 1-AL2: Holladay 1 with modified
Wang-Koch axial length adjustments which included 98 eyes with an axial length
greater than
This study
was designed and performed to investigate the effects of different lens
constants on the accuracy of IOL power calculation formulas in a given series
of highly myopic eyes, using a single IOL model.
Numerous
factors, such as different IOL types, biometry devices, and surgical technique,
can result in systematic prediction errors of IOL formulas. IOL constants like
A-constants are variables introduced to lens power calculation in order to
fine-tune the results. Constants given by lens manufacturers are meant for an
average measurement set-up and always considered as default. Lens constant
optimization is a mathematical method used to reduce the arithmetic mean error
to zero by adjusting the lens constants, thereby eliminating the systematic
myopic or hyperopic prediction error. The SRK/T, Hoffer Q, and Holladay 1
formulas belong to the 3rd generation 2-variable formulas, and their
IOL power prediction curve involves simply changing the position in combination
with different constants. The Haigis formula is the 4th generation
formula using three constants (a0, a1, and a2). The a0 constant sets the
position of the IOL power prediction curve. The a1 and a2 constants are related
to the preoperative ACD and AL, respectively. Therefore, the IOL power
prediction curve of the Haigis formula will change both the position and shape
if the lens constant is optimized based on large pooled data. That in normal
eyes the effectiveness of optimized lens constant is better than that of
manufacture lens constant has been supported by several studies and numerous
authors have recommended the use of the optimized lens constant[14-16]. The ULIB constants were
optimized based on a large number of preoperative and postoperative clinical
data in different surgical centers without differentiating AL. The ULIB
constants are published and freely available on the website and have been
frequently used worldwide.
Currently,
as patients have higher expectations in terms of postoperative visual quality,
there are still challenges remaining for more complex eyes, such as eyes that
had previously undergone refractive surgery[17],
those with an AL shorter than
Adjustment
for AL has been advocated to correct systemic errors in ultrasound biometry for
short and long eyes[20-21].
The Wang-Koch AL adjustment method was validated for use in
In our
study, formulas with AL adjustment reduced MAE and increased the percentage of
eyes with prediction error within a certain range significantly. The Holladay 1
formula with either original or modified Wang-Koch AL adjustment achieved favorable
postoperative refractive outcomes compared with the currently proposed
benchmark standards, with 73% and 96% of the postoperative cataract refractive
outcomes lying within ±0.5 D and ±1.0 D of the target, respectively[24]. Our study is the first to evaluate the accuracy of
modified AL adjustment method. Our results show that the modified version has a
lower MAE and a higher percentage of prediction error within ±0.5 D and ±1.0 D
than the original one, but with no statistical significance. However, the
modified version has a tendency towards hyperopia whereas the ME of original
version was nearly equal to zero. The original Wang-Koch AL adjustment alone
has almost eliminated the hyperopic error in IOL formula prediction for highly
myopic eyes for all formulas. Combining the Wang-Koch AL adjustment with
constant optimization for long eyes resulted in obvious overcorrection. The
predicted refractive outcomes in such combination were clearly toward myopia,
with decreased MAE and percentage within a certain range (data not shown).
Therefore, it is neither recommended nor necessary to combine these two
methods.
Based on
thick lens models and the paraxial ray tracing theory, considering the position
of principal planes when a low-power positive IOL changes to a negative one,
the Barrett Universal II formula was one of the most accurate formulas for long
eyes, as was showed in a recent meta-analysis[25].
Therefore, the Barrett Universal II formula has a unique advantage in extremely
long eyes that require a low dioptric power IOL. For surgeons’ convenience, the
calculation for Barrett Universal II formula is offered on the website for free[26] and it is not necessary to optimize the AL or the
constant. Our results show that Barrett Universal II formula demonstrates
similar accuracy to formulas with Wang-Koch AL adjustment, consistent with
previous researches[19,27].
Our study
has some limitations. First, the retrospective design itself is defective.
Therefore, we continuously included patients who met the inclusion criteria to
avoid a selection bias. Two independent researchers (Zhang JQ and Zou XY) input
data separately. A third researcher (Sun A) verified the accuracy of the data
to avoid mistakes in data transcription. Second, postoperative subjective refraction
was performed by multiple opticians. Interobserver variability may introduce
measurement errors. Uniform training in the hospital may minimize the impact of
this bias on the study. Finally, the optimization of the Haigis formula was
restricted by the small sample size. Only the a0 constant was optimized. The a1
and a2 constants were retained at the default value as they need data from more
than 250 subjects to be optimized. Studies with larger sample sizes are needed
to assess the accuracy of the Haigis formula with different constants.
Further
studies should address the effectiveness of constants optimized separately for
short eyes or eyes that had previously undergone refractive surgery. We can
also try to optimize IOL calculations for specific ALs, but doing so is far
more complicated than just adjusting IOL constant or AL in a linear way. More
variables should take into account, such as keratometry, ACD, preoperative
refraction, the size of capsular bag, etc. Some formulas, such as the
Hill-RBF[28] and Ladas Super formula[29], use a sophisticated computer-based statistical model
based on the large library data set in order to find relationships not
otherwise evident in theoretical approaches. These formulas will evolve over
time as more information is incorporated and will bring us further in the field
of lens power calculation.
In
conclusion, our results suggest that lens constant optimization based on long
eyes alone did not show additional benefits for highly myopic eyes than using
optimized constant based on all eyes. Both the original Wang-Koch AL adjustment
method and the Barrett Universal II formula have favorable postoperative
refraction outcome, while the modified Wang-Koch AL adjustment method has a
tendency towards hyperopia and a similar prediction accuracy.
Foundation: Supported by National Natural
Science Foundation of China (No.81770905). The funding organization had no role
in the design or conduct of this research.
Conflicts of
Interest: Zhang JQ,
None; Zou XY, None; Zheng DY, None; Chen WR, None; Sun
A, None; Luo LX, None.