
Citation: Subasi S,
Yuksel N, Karabas VL, Yilmaz Tugan B. Late in-the-bag spontaneous IOL
dislocation: risk factors and surgical outcomes. Int J Ophthalmol 2019;12(6):954-960
DOI:10.18240/ijo.2019.06.12
·Clinical Research·
Late in-the-bag spontaneous IOL dislocation: risk factors
and surgical outcomes
Sevgi
Subasi1, Nursen Yuksel1, V. Levent Karabas1,
Busra Yilmaz Tugan2
1Department
of Ophthalmology, Medical School, Kocaeli University, Kocaeli 41380, Turkey
2Department of Ophthalmology, Patnos
State Hospital, Ağri 04500, Turkey
Correspondence to: Sevgi Subasi. Department of
Ophthalmology, Medical School, Kocaeli University, Kocaeli 41380, Turkey.
sevgiozel_5@hotmail.com
Received:
Abstract
AIM: To evaluate the possible
predisposing risk factors for late in-the-bag spontaneous IOL dislocations and
to study the early surgical and visual outcomes of repositioning and exchange
surgeries.
METHODS: Medical and surgical records of
39 eyes of 39 patients who underwent IOL repositioning or exchange surgery for
dislocation between 2010 and 2018 were reviewed. Possible predisposing risk
factors and some characteristics of late in-the-bag spontaneous IOL
dislocations; outcomes of IOL repositioning and exchange surgeries, including
visual acuity, refractive status before and after surgery and postoperative
complications were evaluated.
RESULTS: The predisposing factors for
late in-the-bag spontaneous IOL dislocations were pseudoexfoliation [PEX; 12/39
(30.8%)], previous vitreoretinal surgery [7/39 (17.9%)], axial myopia [3/39
(7.7%)], both PEX and axial myopia [1/39 (2.6%)], both previous vitreoretinal
surgery and axial myopia [2/39 (5.1%)] and uveitis [1/39 (2.6%)]. The mean
interval between cataract and dislocation surgery was 7.23y, greater in PEX
positive group (8.63y). The mean best corrected visual acuity (BCVA) improved
significantly after dislocation surgery (P<0.001) and also improved
significantly after exchange surgery (P=0.001). The mean value of
spherical equivalant decreased significantly after dislocation surgery (P=0.011),
whereas corneal astigmatism increased but this difference was not significant
after dislocation surgery and exchange surgery (P=0.191, P=0.074,
respectively).
CONCLUSION: The most prevelant risk factors
for late in-the-bag spontaneous IOL dislocations are PEX, previous
vitreoretinal surgery and axial myopia. In the management of IOL dislocations,
exchange surgery with small corneal incision seemed effective with improved
BCVA and safety with low postoperative complications.
KEYWORDS: IOL
dislocation; risk factors; IOL repositioning; IOL exchange
DOI:10.18240/ijo.2019.06.12
Citation: Subasi S, Yuksel N, Karabas VL, Yilmaz Tugan B. Late
in-the-bag spontaneous IOL dislocation: risk factors and surgical outcomes. Int
J Ophthalmol 2019;12(6):954-960
Outline
One of the most serious complications of uneventful cataract surgeries is
late in-the-bag intraocular lens (IOL) dislocations. Dislocation of the
IOL-capsule complex was first described in 1993[1] and has been
reported with an increasing frequency in recent years[2]. Late
spontaneous IOL dislocation within the capsular bag (more than 3mo after
surgery) occurs several years after cataract surgery and depends upon slowly
progressive dehiscence of the zonules[3-4]. Possible
predisposing factors suggested for late in-the-bag dislocations are
pseudoexfoliation (PEX), previous vitreoretinal surgery, axial myopia, uveitis,
retinitis pigmentosa and connective tissue disorders[5-9].
If the dislocation causes visual symptoms or some complications,
repositioning or exchange of the IOL is required. The optimal management for
late in-the-bag IOL dislocation is still being questioned. Different surgical
procedures such as repositioning of the existing IOL by fixating it to scleral
wall or to the iris or exchanging the capsule-IOL complex with a new IOL are performed[2].
The purpose of the study were to clarify the possible predisposing factors for
late spontaneous in-the-bag IOL dislocations and to evaluate the early outcomes
of surgical methods.
Ethical Approval The study was
approved by the Ethics Committee of the Kocaeli University and conformed to the
guidelines of the Declaration of Helsinki. An informed consent was obtained
from all individual participants included in the study.
Subjects This retrospective study was
conducted with medical and surgical records of all the subjects who required
surgical management because of spontaneous dislocation of posterior chamber
IOLs within the capsular bag after cataract surgery. During January 2010 and July 2018, a
total of 39 eyes of 39
patients were included in the study if spontaneous IOL dislocation was
diagnosed 3mo or later
after uneventful cataract surgery with endocapsular IOL implantation.
Indications for dislocation surgery were visual symptoms or rapid and
distinct dislocation. Follow up after dislocation surgery of at least 1mo was
required. Subjects of IOL dislocation from ocular trauma were excluded. Main
exclusion criteria were out-of-the bag IOL dislocations and dislocations that
occured after complicated cataract surgery in the first 3mo.
The data included age, sex, side, at the time of cataract surgery,
predisposing factors for dislocation, interval between cataract surgery and
dislocation, the type of the surgical procedure to manage IOL dislocation,
axial length, grade, type and place of IOL dislocation, follow-up time,
preoperative and postoperative logarithm of the minimal angle of resolution
(logMAR) uncorrected visual acuity (UCVA) and best corrected visual acuity
(BCVA), intraocular pressure (IOP), spherical equivalant, corneal
astigmatism, refractive astigmatism and postoperative complications were
rewieved. The refractive
states (spherical equivalant, corneal and refractive astigmatism) were examined
objectively using an autorefractometer and keratometer (NIDEK ARK
Dislocation grade was identified as small, moderate or total. If the IOL is
centered but a gap is present between the pupillary margin and the IOL and
related with diplopia and pseudophakodonesis that was defined as small. In
moderate dislocation, IOL is decentered and observed in the pupillary area
which related with reduction in patient’s vision. In total dislocation, the IOL
is not visible in pupillary area[10]. The place of
IOL dislocation (inferior, superior or vitreous cavity) was evaluated after
mydriasis.
Surgical Procedures The dislocation
surgeries were performed by two
experienced surgeons (an anterior segment surgeon and a posterior segment
surgeon) in one center. The same protocol was followed during the surgeries,
all posterior approaches were performed by the same posterior segment surgeon.
The choice of surgery type was the surgeon’s preference. Especially exchange
surgery was applied to patients who had opacification on optics, inflammatory
accumulation, and usually monoblock lenses that were damaged in their haptics. All
surgeries were performed using peribulbar anesthesia. We choosed the anterior
approach with scleral sutures, iris sutures or exchange tecnique if the IOL is
dislocated along the iris plane only and some piece of the optic is visible in
the pupil. If the IOL
dislocated posteriorly in the vitreous cavity or laterally from the posterior
chamber to the vitreous, we choosed posterior approach with pars plana
vitrectomy. In anterior approach, when there is vitreus strands prolapsed
around or in front of the IOL, we performed anterior vitrectomy. Then, the
original IOL’s dislocated haptic was repositioned to peripheral iris with iris
sutures in posterior chamber. IOL reposition with scleral sutures was performed
using an ab externo scleral fixation technique with temporary
haptic externalization for the
placement of scleral fixation suture[11].
In the exchange surgery, the dislocated IOL was pulled up into the anterior
chamber (AC) through side
ports using a forceps. When the IOL was dislocated into the vitreous cavity,
pars plana vitrectomy (PPV) was performed and IOL lifted up into the AC using
an internal limitan membrane forceps. IOL was cut in the AC with IOL cutting
microscissors and removed from approximately a 3 or
Statistical Analysis All statistical
analyses were performed using IBM SPSS for Windows version 20.0 (IBM Corp.,
Armonk, NY, USA).
Kolmogorov-Smirnov tests were used to test the normality of data distribution.
Continuous variables were expressed as mean±standard deviation (SD), median (25th-75th
percentiles), and categorical variables were expressed as counts (percentages).
Comparisons of normally distributed continuous variables between the groups
were performed using the Student’s t-test. Comparisons of nonnormally distributed
continuous variables between the groups were performed using the Mann Whitney U
test.
Comparisons of normally distributed continuous paired variables between the
times were performed using the paired samples t-test and nonnormally distributed continuous
variables between the times were performed using the Wilcoxon t-test.
Comparisons of cathegorical variables between the groups were performed using
the Fisher’s exact Chi-square test, Yates’ Chi-square test and Monte Carlo
Chi-square test. A two-sided P value <0.05 was considered
statistically significant.
Thirty-nine eyes of 39 patients fulfilled the criteria of spontaneous late
dislocated in-the-bag IOL were included in the study. There were 26 (66.7%)
males and 13 (33.3%) females. The mean age at cataract surgery was 62.77±14.62y (range,
23 to 87y) and the mean
age at the time of dislocation was 70.05±13.09y (range,
39 to 89y). The interval
between the uneventful cataract surgery and the spontaneous dislocation was
7.23±4.69y (range, 1 to 23y). The
distrubition of the interval between the cataract and the dislocation surgery
is shown in Figure 1 and Table 1.
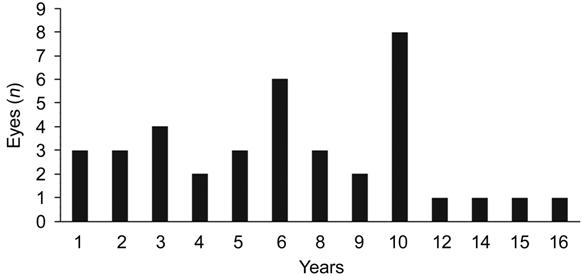
Figure 1 Years between cataract surgery and
IOL dislocation.
Table 1 Characteristics of all
patients and main predisposing factors mean±SD
|
Characteristics |
Total (n=39) |
Pseudoexfoliation
(n=13) |
Previous
vitreoretinal surgery (n=9) |
Axial myopia
(n=6) |
P |
|
Age at cataract surgery, y |
62.77±14.62 |
70.38±5.22 |
54.67±17.07 |
52.83±21.27 |
|
|
Age at IOL dislocation, y |
70.05±13.09 |
79±4.65 |
60.22±14.99 |
63±15.84 |
< |
|
Interval, y |
7.23±4.69 |
8.62±2.72 |
5.56±4.79 |
9.83±6.91 |
|
|
Sex, n (%) |
|
|
|
|
|
|
Male |
26 (66.7) |
10 (76.9) |
5 (55.6) |
3 (50) |
|
|
Female |
13 (33.3) |
3 (23.2) |
4 (44.4) |
3 (50) |
|
|
Side, n (%) |
|
|
|
|
|
|
Right |
21 (53.8) |
7 (53.8) |
4 (44.4) |
4 (66.7) |
|
|
Left |
18 (46.2) |
6 (46.2) |
5 (55.6) |
2 (33.3) |
|
|
Axial length, mm |
24.36±1.41 |
23.59±1.11 |
25.24±1.52 |
26.87±0.83 |
|
aComparison between with pseudoexfoliation and without pseudoexfoliation; bComparison
between with previous
vitreoretinal surgery and without previous
vitreoretinal surgery; cComparison
between with axial myopia
and without axial myopia.
Possible main predisposing factors of the 39 eyes that experienced
in-the-bag dislocation were PEX, in 12 eyes (30.8%); previous vitreoretinal
surgery in 7 (17.9%); axial myopia
in 3 (7.7%); both PEX and axial myopia together, in 1 (2.6%); both previous
vitreoretinal surgery and axial myopia together in 2 (5.1%) and uveitis in 1
(2.6%). There were no
identifiable predisposing factors in 13 eyes (33.3%). The reasons of
previous vitreoretinal surgery include rhegmatogenous retinal deteachment (n=6),
epiretinal membrane (n=1), maculer hole (n=1) and hemorrhagic
retinal deteachment related with age related macular degeneration (n=1).
Characteristic data of all patients and main predisposing factors were listed in
Table 1.
The mean preoperative IOP of the eyes with IOL dislocation was 17.85±
Table 2 Pre- and
postoperative evaluations of all patients and main predisposing factors
|
Parameters |
Total (n=39) |
Pseudoexfoliation
(n=13) |
Previous
vitreoretinal surgery (n=9) |
Axial myopia (n=6) |
|
IOP, mean±SD, mm Hg |
|
|
|
|
|
Preoperative |
17.85±7.98 |
17.92±7.63 |
17.92±7.63 |
20.17±8.90 |
|
Postoperative |
14.13±2.38 |
14.38±2.29 |
14.38±2.29 |
14.67±2.33 |
|
Postoperative IOP management, n
(%) |
|
|
|
|
|
Medical treatment |
8 (88.9) |
3 (75) |
1 (100) |
2 (100) |
|
Trabeculectomy |
1 (11.1) |
1 (25) |
0 |
0 |
|
Grade of IOL dislocation, n (%) |
|
|
|
|
|
Small |
5 (12.8) |
1 (7.7) |
0 |
0 |
|
Moderate |
28 (71.8) |
11 (84.6) |
8 (88.9) |
5 (83.3) |
|
Total |
6 (15.4) |
1 (7.7) |
1(11.1) |
1 (16.7) |
|
Place of IOL dislocation, n (%) |
|
|
|
|
|
At IOL plane, inferior |
38 (97.4) |
13 (100) |
9 (100) |
6 (100) |
|
At IOL plane, superior |
0 |
0 |
0 |
0 |
|
Vitreous cavity |
1 (2.6) |
0 |
0 |
0 |
|
Ocular comorbidity, n (%) |
|
|
|
|
|
Glaucoma |
6 (15.4) |
5 (38.5) |
0 |
0 |
|
AMD |
4 (10.3) |
1 (7.7) |
1 (11.1) |
0 |
|
Epiretinal membrane |
3 (7.7) |
1 (7.7) |
1 (11.1) |
1 (16.7) |
|
Macular hole |
1 (2.6) |
0 |
1 (11.1) |
0 |
|
Retinal deteachment surgery |
6 (15.3) |
0 |
6 (66.6) |
1 (16.7) |
|
None |
19 (48.7) |
6 (46.2) |
0 |
4 (66.7) |
|
Predisposing factors, n (%) |
|
|
|
|
|
PEX |
12 (30.8) |
12 (92.3) |
- |
- |
|
Previous vitreoretinal surgery |
7 (17.9) |
- |
7 (77.8) |
- |
|
Axial myopia (≥ |
3 (7.7) |
- |
- |
3 (50) |
|
PEX+axial myopia |
1 (2.6) |
1 (7.7) |
- |
1 (16.7) |
|
Previous vitreoretinal
surgery+axial myopia |
2 (5.1) |
- |
2 (22.2) |
2 (33.3) |
|
Uveitis |
1 (2.6) |
- |
- |
- |
|
None |
13 (33.3) |
- |
- |
- |
IOP: Intraocular
pressure; AMD: Age-related
macular degeneration; PEX: Pseudoexfoliation.
The dislocated IOL was replaced by an anterior approach with or without
anterior vitrectomy in 35 cases (89.7%) and a posterior approach with pars
plana vitrectomy in 4 cases (10.3%). The IOL was repositioned in the posterior
chamber with scleral sutures in 15 (35.8%),
with iris sutures in 2 (5.1%) and
exchanged in 18 (46.2%) cases
with anterior approach. The IOL was repositioned in the posterior chamber with
scleral sutures in 3 (7.7%) and
exchanged in 1 (2.6%) cases
with posterior approach with pars plana vitrectomy (Table 3).
Table 3
Surgical types of cases with in-the-bag dislocated IOL n (%)
|
Type of surgery |
Cases |
|
Anterior approach with or
without anterior vitrectomy |
|
|
IOL repositioning with scleral
sutures |
15 (35.8) |
|
IOL repositioning with iris
sutures |
2 (5.1) |
|
IOL exchanged |
18 (46.2) |
|
Posterior approach with pars
plana vitrectomy |
|
|
IOL repositioning with scleral
sutures |
3 (7.7) |
|
IOL repositioning with iris
sutures |
0 |
|
IOL exchanged |
1 (2.6) |
The visual outcomes of all patients and surgical types are presented in
Table 4. Overal, the mean logMAR BCVA had improved significantly from
preoperative 0.63 to postoperative 0.42 (P<0.001). The mean value of
spherical equivalant decreased (P=0.011), corneal
astigmatism increased, but the increase was not significant (P=0.191)
and refractive astigmatism did not change after surgery (P=1.000). In addition,
the mean logMAR BCVA had
improved significantly from preoperative 0.64 to postoperative 0.21 (P=0.001)
in exchange surgery group. The spherical equivalant was decreased and corneal
astigmatism was increased after IOL exchange surgery but they were not
significantly different (P=0.109, 0.074, respectively). Seventy four
percent of the total eyes (29/39) attained gain of more than 1 line after
dislocation surgery with 70% (14/20)
in the repositioning surgery group and 78.9% (15/19) in
exchange surgery group.
Table 4 Pre- and
postoperative visual outcomes of all patients and surgery types
n (%)
|
Parameters |
Total (n=39) |
Repositioning
surgery (n=20) |
Exchange
surgery (n=19) |
P |
|||
|
Preoperative |
Postoperative |
Preoperative |
Postoperative |
Preoperative |
Postoperative |
||
|
UCVA, mean±SD |
0.89±0.59 |
0.68±0.53 |
0.91±0.56 |
0.86±0.61 |
0.87±0.62 |
0.50±0.36 |
|
|
0.1 or beter |
0 |
2 (5.1) |
0 |
0 |
0 |
2 (10.5) |
|
|
0.2-0.4 |
11 (28.2) |
15 (38.5) |
5 (25) |
6 (30) |
6 (31.6) |
9 (47.4) |
|
|
0.5-0.9 |
7 (17.9) |
10 (25.6) |
2 (10) |
5 (25) |
5 (26.3) |
5 (26.3) |
|
|
1 or worse |
21 (53.8) |
12 (30.8) |
13 (65) |
9 (45) |
8 (42.1) |
3 (15.8) |
|
|
BCVA, mean±SD |
0.63±0.57 |
0.42±0.55 |
0.62±0.50 |
0.62±0.68 |
0.64±0.64 |
0.21±0.24 |
< |
|
0.1 or beter |
7 (17.9) |
16 (41) |
1 (5) |
5 (25) |
6 (31.6) |
11 (57.9) |
|
|
0.2-0.4 |
13 (33.3) |
13 (33.3) |
9 (45) |
7 (35) |
4 (21.1) |
6 (31.6) |
|
|
0.5-0.9 |
5 (12.8) |
6 (15.4) |
2 (10) |
4 (20) |
3 (15.8) |
2 (10.5) |
|
|
1 or worse |
14 (35.9) |
4 (10.3) |
8 (40) |
4 (20) |
6 (31.6) |
0 |
|
|
Spherical equivalant, median (25th-75th
percentiles) |
7.0 (1.37-11) |
1.50 (1.50-2.50) |
2.00 (1.0-11.0) |
1.50 (1.50-2.75) |
8.0 (3.0-11.0) |
1.50 (1.50-2.0) |
|
|
Corneal astigmatism, median (25th-75th
percentiles) |
1.90 (1.19-2.89) |
2.50 (1.50-3.50) |
2.75 (1.31-3.73) |
2.50 (2.00-3.00) |
1.45 (0.97-2.22) |
2.25 (0.81-3.50) |
|
|
Refractive astigmatism, median (25th-75th
percentiles) |
2.00 (2.00-2.00) |
2.00 (1.00-2.00) |
2.00 (2.00-2.00) |
2.00 (2.00-3.00) |
2.50 (0.50-3.75) |
1.50 (1.00-2.00) |
|
|
Lines change of BCVA |
|
|
|
|
|||
|
Loss 1-2 lines |
3 (7.7) |
3 (15) |
0 |
||||
|
Same |
7 (17.9) |
3 (15) |
4 (21.1) |
||||
|
Gain more than 1 line |
29 (74.4) |
14 (70) |
15 (78.9) |
||||
|
Cause of BCVA 0.4 or worse |
16 (41.02) |
11 (55) |
5 (26.31) |
- |
|||
|
Glaucoma |
7 |
4 |
3 |
||||
|
AMD |
2 |
2 |
0 |
||||
|
Epiretinal membrane |
2 |
0 |
2 |
||||
|
Endophthalmitis |
1 |
1 |
0 |
||||
|
Previous retinal deteachment surgery |
1 |
1 |
0 |
||||
|
Corneal decompansation |
2 |
2 |
0 |
||||
|
Vitreous hemorrhage |
1 |
1 |
0 |
||||
UCVA: Uncorrected
visual acuity; BCVA: Best corrected
visual acuity; IOP: Intraocular
pressure; AMD: Age-related
macular degeneration. aComparison
between pre- and
postoperative values in total group; bComparison between pre-
and postoperative values in repositioning surgery group; cComparison
between pre- and
postoperative values in exchange surgery group.
The overal complication rate after the dislocation surgery was 35.9%. The
postoperative complications were glaucoma (5 eyes, 12.8%; one of them
had PEX glaucoma previously;
two of them were miyopic dislocation), vitreous hemorrhage (1 eye, 2.6%; this patient
was operated previously because of retinal deteachment), corneal decompansation
(2 eyes, 5.1%; one of them
was treated intravitreal dexamethasone implantation previously because of retinal
pathology which moved to anterior segment and caused corneal decompansation; other one was a
nonregulated diabetic patient who was vitrectomized because of macular hole
previously), tilted IOL (1 eye, 2.6%; previously PEX glaucoma), endophthalmitis (1 eye, 2.6%; PEX), both
glaucoma and cystoid macular edema (2 eyes, 5.1%; one of them
had PEX glaucoma previously, other one was miyopic dislocation), both glaucoma
and retinal deteachment (2 eyes, 5.1%; Table 5).
Table 5 Postoperative complication rates after
dislocated IOL surgeries
n (%)
|
Complications |
All
procedures (n=39) |
Exchange
surgery (n=19) |
Repositioning
surgery (n=20) |
|
Glaucoma |
5 (12.8) |
3 (18.8) |
2 (10) |
|
CME |
0 |
0 |
0 |
|
RD |
0 |
0 |
0 |
|
Vitreous hemorrhage |
1 (2.6) |
0 |
1 (5) |
|
Corneal decompansation |
2 (5.1) |
0 |
2 (10) |
|
Tilted IOL |
1 (2.6) |
0 |
1 (5) |
|
Suture exposure requiring
scleral flap surgery |
1 (2.6) |
1 (5.3) |
0 |
|
Endophthalmitis |
1 (2.6) |
0 |
1 (5) |
|
Glaucoma+CME |
2 (5.1) |
1 (5.3) |
1 (5) |
|
Glaucoma+RD |
1 (2.6) |
1 (5.3) |
0 |
|
None |
25 (64.1) |
13 (68) |
11 (55) |
CME: Cystoid macular
edema; RD: Retinal
deteachment.
Dislocation of IOLs are optical malpositioning complications of cataract
surgery. IOLs seem to be
dislocated with respect to time in a bimodal distribution[13]. Early
dislocations ocur due to improper IOL fixation within the secure capsular bag
and usually caused by tearing of the posterior capsule and zonular rupture.
Late dislocations occur three months or later after uncomplicated cataract
surgery as a result of progressive zonular weakness. Zonular insufficiency is
the common cause of in-the-bag late IOL dislocations[4,8,10]. The rate of
posterior chamber IOL dislocations has been reported as 0.2% to 3% and late
spontaneous dislocation is a small part of this group[10,14].
There are many predisposing factors associated with zonular weakness
including PEX, previous vitreoretinal surgery, axial myopia, uveitis, retinitis
pigmentosa and connective tissue disorders. Most of the previous studies of
spontaneous in-the-bag late IOL dislocation concluded that PEX was the most
common significant risk factor[15-18]. In our study,
similar to the previous studies the most predisposing risk factor was PEX in 12
eyes (30.8%). PEX accumulations mechanically weaken the zonule, and impair
zonular anchoring. When enough zonules are breached, dislocation of the bag-IOL
complex occurs[19-20]. In our study,
the overall mean time from cataract surgery to in-the bag IOL dislocation was
7.23y. In the PEX group, the
intervale was 8.63y. This results are similar to those reported in previous
studies of late in-the-bag IOL dislocations in which major predisposing factor
was identified as PEX (e.g. 6.9y[21], 8.3y[3], 8.5y[10] and 10.3y[22]). The
analysis of the eyes with and without PEX revealed some significant differences:
the mean age at cataract surgery (70.38y, P=0.003) and dislocation
surgery (79y, P<0.001) were older in patients with PEX and they had a
shorter axial lenght (
Previous studies have analyzed whether the type of posterior chamber IOL
can influence the risk of in the bag lens dislocation. The most common
dislocated IOL was 3 piece acrylic in the studies of Hayashi et al[3] and Lorente et al[24] and 1 piece
PMMA in the studies of Gimbel et al[2], Kim et al[15]
and Gross et al[21]. However, none of these studies allow us
to evaluate the risk for spontaneous late dislocation associated with a
particular IOL material or design because they did not include a control group.
Davis et al[13] indicated that all types of IOL could be
involved. The preponderance of 1 type of IOL over others more likely reflects
the most commonly used IOL at the time of original surgery. In our study, all
dislocated IOLs were hydrophobic material because of this we did not make any
comparison of the effect of this condition on dislocation.
Several associated conditions were detected (glaucoma, age-related macular
degeneration, epiretinal membrane, macular hole, previous retinal deteachment
surgery) in our patients. The most common condition was glaucoma which was
detected in 6 eyes before surgery, 5 of which presented with pseudoexfoliation.
We observed a normalization of IOP after surgical correction of IOL position in
1 case spontaneously, in 3 cases with medical therapy and in 1 case with
trabeculectomy in patients with pseudoexfoliation. In other predisposing factor
groups we required medical treatment for IOP decrease after dislocation surgery
which was not enough alone. Several
previous studies have reported an association between late in-the-bag IOL
dislocation and increased IOP[24-25]. Regardless of
the explanatory mechanism, there are examples where associated high IOP has
been resolved by IOL dislocation surgery, either completely or partially[16,24].
But both studies have few patients and this condition limits their ability to
examine the possible IOP-lowering effect of dislocation surgery. Kristianslund et
al[22] reported that
increased IOP after in-the-bag IOL
dislocation can not be resolved by dislocation surgery alone and IOL exchange
surgery may have a more benefical effect on the postoperative IOP compared to
repositioning surgery.
Different surgical techniques can be used in management of dislocated IOL.
The choice of surgical thecnique depends on the surgeon’s preferences and
management of the IOL with different suturing techniques and if the IOL is
preserved or exchanged[2]. There is no consensus on which technique
to use and several surgical methods are suggested to give good results[2,21]. In some eye
clinics, dislocated IOLs are operated by only vitreoretinal surgeons, in
others, such as in ours, also anterior segment surgeons manage these conditions
that IOL-capsule complex can be identified in the pupillary area. We used to
compare 2 principally different operation methods. One of them posterior
chamber IOL fixation with transcleral or iris suturing of patients original
IOLs. Other method is exchange the original IOL to new three piece foldabl IOL
which was implanted to posterior chamber with transcleral fixation sutures. In the exchange
surgery group, we experienced a significant improvement in BCVA postoperatively
and 78.9% of the patients reached gain of more than 1 line at 1mo postoperative
follow-up. In the repositioning surgery
group, we did not experienced a significant improvement in BCVA postoperatively
and 15% of patients reached loss of 1-2 lines at 1mo postoperative follow-up.
We think that this result is due to serious postoperative complications
(retinal deteachment, endophthalmitis, corneal decompansation) in repositioning
group. Because, furthermore, 70% of the patients reached gain of more than 1
line in repositioning group and this result was close to the exchange surgery
group. Therefore, mean
logMAR BCVA improved significantly from 0.63 to 0.42 (P<0.001), and
logMAR BCVA of 0.4 or better achieved in 74.3% of all patients. In exchange
surgery group, mean logMAR BCVA
improved significantly from 0.64 to 0.21 (P=0.001), with logMAR BCVA of
0.4 or better achieved in 89.5%. The mean logMAR BCVA of
0.3 or better achived in 47.5% and 62.22% after exchange surgery in
Fernández-Buenaga et al[18] and Lorenta et al[24]
studies respectively. Fernández-Buenaga et al[18] have
attributed this result to postoperative serious complications. High
complication rate was seen in our
study because of the ocular comorbidities of patients which was explained in
results. The most of specified complications were related with the ocular
history of the patients, not related with dislocation surgery.
In some of previous studies compairing IOL
repositioning with IOL exchange by different thecniques, suggested that the
operation methods had similar efficacy in terms of visual outcome[22,24-26].
On the other hand, some authors agree that it is desirable to reposition the
existing IOL if possible, to avoid the complications related with exchange
surgery such as induced corneal astigmatism and surgical trauma because of
large corneal wound[3]. In our study, all removed lenses were
foldabl and cut through a small incision and implantation of new three piece
foldable IOL was
performed through this small incision. We observed that corneal astigmatism
increased after both of the surgical type but the difference did not reach
statistical significance in two methods.
In conclusion, our study includes the comparison of risk factors for late
dislocations as well as comparison of two different specific surgical methods
for the treatment of this condition. It highlights that PEX is an important predisposing factor for the spontaneous
late in-the-bag IOL
dislocation after uneventful cataract surgery. Dislocation related with PEX
occured at an older age than other predisposing factors. It shows that small
incision exchange surgeries can be performed safely in dislocations and the
effects on refractive state will not be worse than repositioning surgery by
means of visual acuity improvement. IOL exchange with transcleral suturing with
small corneal incision was a good and safe technique, postoperative visual
outcomes improved significantly with low complication rates.
Conflicts of Interest: Subasi S, None; Yuksel N, None; Karabas VL, None; Yilmaz Tugan B, None.
|
1 Davison
JA. Capsule contraction syndrome. J Cataract Refract Surg 1993;19(5):582-589. |
|
|
|
|
|
2 Gimbel
HV, Condon GP, Kohnen T, Olson RJ, Halkiadakis I. Late in-the-bag intraocular
lens dislocation: incidence, prevention, and management. J Cataract Refract
Surg 2005;31(11):2193-2204. |
|
|
|
|
|
3 Hayashi
K, Hirata A, Hayashi H. Possible predisposing factors for in-the-bag and
out-of-the-bag intraocular lens dislocation and outcomes of intraocular lens
exchange surgery. Ophthalmology 2007;114(5):969-975. |
|
|
|
|
|
4 Böke WR,
Krüger HC. Causes and management of posterior chamber lens displacement. J Am
Intraocul Implant Soc 1985;11(2):179-184. |
|
|
|
|
|
5 Jehan
FS, Mamalis N, Crandall AS. Spontaneous late dislocation of intraocular lens
within the capsular bag in pseudoexfoliation patients. Ophthalmology
2001;108(10):1727-1731. |
|
|
|
|
|
6 Zech JC,
Tanniére P, Denis P, Trepsat C. Posterior chamber intraocular lens
dislocation with the bag. J Cataract Refract Surg 1999;25(8):1168-1169. |
|
|
|
|
|
7 Yasuda
A, Ohkoshi K, Orihara Y, Kusano Y, Sakuma A, Yamaguchi T. Spontaneous
luxation of encapsulated intraocular lens onto the retina after a triple
procedure of vitrectomy, phacoemulsification, and intraocular lens
implantation. Am J Ophthalmol 2000;130(6):836-837. |
|
|
|
|
|
8 Hayashi
K, Hayashi H, Matsuo K, Nakao F, Hayashi F. Anterior capsule contraction and
intraocular lens dislocation after implant surgery in eyes with retinitis
pigmentosa. Ophthalmology 1998;105(7):1239-1243. |
|
|
|
|
|
9 Cionni
RJ. Surgical management of the congenitally subluxated crystalline lens using
the modified capsular tension ring. In: Steinert RF, ed. Cataract Surgery:
Technique, Complications, and Management. 2nd ed. Philadelphia, PA: Saunders
2004:305-313. |
|
|
|
|
|
10 Krėpštė
L, Kuzmienė L, Miliauskas A, Janulevičienė I. Possible predisposing factors
for late intraocular lens dislocation after routine cataract surgery.
Medicina (Kaunas) 2013;49(5):229-234. |
|
|
|
|
|
11
Nikeghbali A, Falavarjani KG. Modified transscleral fixation technique for
refixation of dislocated intraocular lenses. J Cataract Refract Surg
2008;34(5):743-748. |
|
|
|
|
|
12 Kaynak
S, Ozbek Z, Pasa E, Oner FH, Cingil G. Transscleral fixation of foldable
intraocular lenses. J Cataract Refract Surg 2004; 30(4):854-857. |
|
|
|
|
|
13 Davis
D, Brubaker J, Espandar L, Stringham J, Crandall A, Werner L, Mamalis N. Late
in-the-bag spontaneous intraocular lens dislocation: evaluation of 86
consecutive cases. Ophthalmology 2009;116(4):664-670. |
|
|
|
|
|
14 Stark WJ
Jr, Maumenee AE, Datiles M, Fagadau W, Baker CC, Worthen D, Auer C, Klein P,
McGhee E, Jacobs ME. Intraocular lenses: complications and visual results.
Trans Am Ophthalmol Soc 1983;81:280-309. |
|
|
|
|
|
15 Kim SS,
Smiddy WE, Feuer W, Shi W. Management of dislocated intraocular lenses.
Ophthalmology 2008;115(10):1699-1704. |
|
|
|
|
|
16
Jakobsson G, Zetterberg M, Lundström M, Stenevi U, Grenmark R, Sundelin K.
Late dislocation of in-the-bag and out-of-the bag intraocular lenses: ocular
and surgical characteristics and time to lens repositioning. J Cataract
Refract Surg 2010;36(10):1637-1644. |
|
|
|
|
|
17
Pueringer SL, Hodge DO, Erie JC. Risk of late intraocular lens dislocation
after cataract surgery, 1980-2009: a population-based study. Am J Ophthalmol
2011;152(4):618-623. |
|
|
|
|
|
18
Fernández-Buenaga R, Alio JL, Pérez-Ardoy AL, Larrosa-Quesada A,
Pinilla-Cortés L, Barraquer R, Alio JL 2nd, Muñoz-Negrete FJ. Late in-the-bag
intraocular lens dislocation requiring explantation: risk factors and
outcomes. Eye (Lond) 2013;27(7):795-801; quiz 802. |
|
|
|
|
|
19 Conway
RM, Schlötzer-Schrehardt U, Küchle M, Naumann GO. Pseudoexfoliation syndrome:
pathological manifestations of relevance to intraocular surgery. Clin Exp
Ophthalmol 2004;32(2):199-210. |
|
|
|
|
|
20 Zenkel
M, Pöschl E, von der Mark K, Hofmann-Rummelt C, Naumann GO, Kruse FE,
Schlötzer-Schrehardt U. Differential gene expression in pseudoexfoliation
syndrome. Invest Ophthalmol Vis Sci 2005;46(10):3742-3752. |
|
|
|
|
|
21 Gross
JG, Kokame GT, Weinberg DV; Dislocated In-The-Bag Intraocular Lens Study
Group. In-the-bag intraocular lens dislocation. Am J Ophthalmol
2004;137(4):630-635. |
|
|
|
|
|
22 Kristianslund
O, Råen M, Østern AE, Drolsum L. Late in-the-bag intraocular lens
dislocation: a randomized clinical trial comparing lens repositioning and
lens exchange. Ophthalmology 2017;124(2):151-159. |
|
|
|
|
|
23
Mönestam EI. Incidence of dislocation of intraocular lenses and
pseudophakodonesis 10 years after cataract surgery. Ophthalmology
2009;116(12):2315-2320. |
|
|
|
|
|
24 Lorente
R, de Rojas V, Vazquez de Parga P, Moreno C, Landaluce ML, Domínguez R,
Lorente B. Management of late spontaneous in-the-bag intraocular lens
dislocation: Retrospective analysis of 45 cases. J Cataract Refract Surg
2010;36(8):1270-1282. |
|
|
|
|
|
25 Østern
AE, Sandvik GF, Drolsum L. Late in-the-bag intraocular lens dislocation in
eyes with pseudoexfoliation syndrome. Acta Ophthalmol 2014;92(2):184-191. |
|
|
|
|
|
26
Sarrafizadeh R, Ruby AJ, Hassan TS, Williams GA, Garretson BR, Trese MT,
Margherio RR. A comparison of visual results and complications in eyes with
posterior chamber intraocular lens dislocation treated with pars plana
vitrectomy and lens repositioning or lens exchange. Ophthalmology
2001;108(1):82-89. |
|