
Citation: Zhao ZL, Wang SM, Shao CY, Fu Y.
Ascher syndrome: a rare case of blepharochalasis combined with double lip and
Hashimoto’s thyroiditis. Int J Ophthalmol 2019;12(6):1044-1046
DOI:10.18240/ijo.2019.06.26
·Letter to the Editor·
Ascher
syndrome: a rare case of blepharochalasis combined with double lip and
Hashimoto’s thyroiditis
Zhan-Lin Zhao1,2,3, Sheng-Ming Wang1,
Chun-Yi Shao1,2, Yao Fu1,2
1Department
of Ophthalmology, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong
University School of Medicine, Shanghai 200011, China
2Shanghai Key
Laboratory of Orbital Diseases and Ocular Oncology, Shanghai 200011, China
3Shanghai
Jiao Tong University School of Medicine, Shanghai 200011, China
Correspondence
to: Yao Fu.
Department of Ophthalmology, Shanghai Ninth People’s Hospital, Shanghai Jiao
Tong University School of Medicine, Shanghai 200011, China. drfuyaofy@sina.com
Received:
DOI:10.18240/ijo.2019.06.26
Citation: Zhao ZL, Wang SM, Shao CY, Fu Y.
Ascher syndrome: a rare case of blepharochalasis combined with double lip and
Hashimoto’s thyroiditis. Int J Ophthalmol 2019;12(6):1044-1046
Dear Editor,
I am Dr. Yao Fu, from the Department of Ophthalmology,
Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of
Medicine, Shanghai, China. I write to present a rare case of Ascher syndrome.
Ascher syndrome was described first in 1920, presenting
as a combination of blepharochalasis, double lip, and non-toxic goitre[1]. It is considered to be a rare, sporadic, benign
condition and usually has onset during puberty. Although hormonal influences
and autosomal dominant inheritance have been involved in some cases[2], its etiology remains largely unknown. The report is in
accordance with the Declaration of Helsinki Ethical Principles. The patient has
given her consent for her images and related clinical information to be
reported in this journal.
A
28-year-old female patient consulted the Department of Ophthalmology
complaining of bilateral canthal adhesions between her upper and lower eyelids.
The patient had the first edema attack in her upper eyelids at age 14 and
gradually developed lax eyelids and bilateral canthal adhesions. She underwent
bilateral blepharoplasty and lateral canthotomy 7 years ago. However, the
lateral canthal adhesions recurred soon thereafter.
The
palpebral fissure length was:
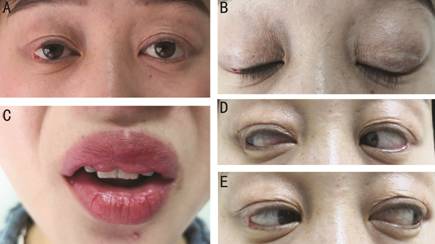
Figure 1
Bilateral blepharochalasis (A, B), double lip (C) and pseudoappearance of the
overaction of the lateral rectus (D, E).
Based on the
clinical and laboratory findings, the patient presented Ascher syndrome and
Hashimoto’s thyroiditis. She therefore underwent bilateral lateral
canthoplasty. Because the patient did not intend to correct the double lip at
the time, only a biopsy of the buccal mucosa was taken during the surgery.
Verhoeff’s elastic stain of the eyelid (Figure
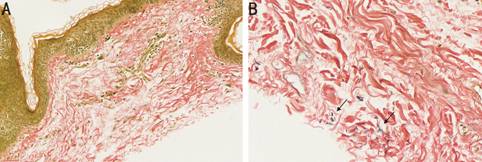
Figure 2
Verhoeff’s elastic stain showed loss of elastic fibres in eyelid (A, 20×) and
very few short elastic fibers (arrow) in buccal mucosa (B, 40×).
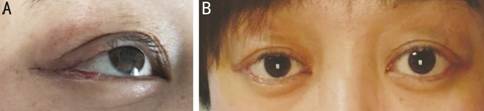
Figure 3
Seven days after the operation, before (A) and after (B) the removal of the
stiches.
Blepharochalasis
is a rare syndrome characterized by recurrent episodes of painless eyelid edema
and represents progressive skin laxity and atrophy due to decreased elastic
fibers. The upper eyelids are usually involved, with an appearance of atrophy,
wrinkles, and often discoloration of the skin[3],
which is present in approximately 80% of Ascher syndrome cases. In our case,
the patient presented with a lateral canthal reattachment, a rounded deformity
of the lateral canthal angle, and a horizontally shortened palpebral fissure.
Her inner intercanthal distance and interpupillary distance were normal. We
assume that this happened due to dehiscence of the lateral canthal tendon from
the orbital tubercle secondary to recurrent attacks of blepharochalasis. In
addition, the elongation/dehiscence of the lateral canthal tendon explained the
reduced distance from the lateral canthus to the mid-pupillary area and the
pseudoappearance of the overaction of the lateral rectus in this patient. Also,
the wrinkles and bronze discoloration at the junction of eyelids could be
observed because of the atrophic skin in the lateral canthal region. In
summary, the patient had a secondary blepharophimosis due to blepharochalasis.
A corrective surgical intervention is currently the primary treatment for
blepharochalasis and blephrophimosis and is recommended at least 6mo after the
most recent exacerbation[4-5].
Blepharochalasis
may also present as ptosis, pseudoepicanthal folds, conjunctival redness, lower
eyelid involvement, etc. It should be distinguished from other lax
eyelid conditions, such as floppy eyelids, herniated orbital fat, and
dermatochalasis. For example, both of blepharochalasis and floppy eyelid may
display eyelid laxity associated with dry eye, conjunctivitis and/or ocular
surface abnormalities (ptosis, upper or lower eyelid entropion). However,
floppy eyelids are more often observed in obese middle-aged men associated with
obstructive sleep apnea[6], while blepharochalasis
occurs in puberty without distinctive distribution between sexes[2].
The double
lip is indispensable for the diagnosis of Ascher syndrome. The deformity
consists of a redundant mucosa, often bilateral, with a midline constriction
because of the attachment of the frenulum[7].
Ascher syndrome usually affects the upper lip and is particularly obvious when
smiling. Recurrent swelling causes duplication between the inner and outer
parts of the upper lip[8]. The treatment for
double lip is corrective surgical intervention, which is indicated mostly for
aesthetic reasons or when having difficulty in chewing or speaking. Non-toxic
enlargement of the thyroid is present in only 10%-50% cases of Ascher syndrome[8], but it is not usually associated with Grave’s disease.
In our case, the five times high titer of blood serum TGAb and TPOAb implicate
Hashimoto’s thyroiditis, because increased antithyroid antibodies are currently
considered the most specific markers to establish the diagnosis[9]. The high plasma IgE level is a non-specific indicator
of over-reactive adaptive immune responses. The cause of Hashimoto’s
thyroiditis in the patient is unknown but may be related to an autoimmune
disorder.
Most cases
of Ascher syndrome are sporadic, but familial cases suggestive of autosomal
dominant inheritance have also been reported[10].
Genes related to blepharochalasis, such as GSN, OSMR, ADAMTS2,
MMP3, and MMP9, have been reported previously[11-13]. In our case, none of the known mutations were
detected in above genes.
This
syndrome is often undiagnosed because of its rarity. The acquired
blepharophimosis in our case is a rare form of blepharochalasis. The
pathological findings of the eyelid and buccal mucosa confirm the diagnosis of
Ascher syndrome. To the best of our knowledge, Hashimoto’s thyroiditis has
never been reported in patients with Ascher syndrome.
ACKNOWLEDGEMENTS
Foundations: Supported by Shanghai Science and Technology Development
Funds (No.17411963800); Shanghai Municipal Education Commission-Gaofeng
Clinical Medicine Grant
(No.20161421); Clinical Research Program of Ninth People’s
Hospital, Shanghai Jiao Tong University School of Medicine (No.JYLJ014); the
Science and Technology Commission of Shanghai (No.17DZ2260100).
Conflicts of
Interest: Zhao ZL, None; Wang SM, None; Shao CY, None; Fu Y, None.
REFERENCES