
·Letter to the Editor·
Incomplete
capsulotomy and lens fragmentation during femtosecond laser-assisted cataract
surgery associated with emulsified anterior chamber silicone oil: a case report
Wei Chen, Yong Wang, Jian Wu, Huai-Jin Guan
Department
of Ophthalmology, Affiliated Hospital of
Correspondence
to: Huai-Jin
Guan and Jian Wu. Department of Ophthalmology, Affiliated Hospital of
Received:
DOI:10.18240/ijo.2019.06.27
Citation: Chen
W, Wang Y, Wu J, Guan HJ. Incomplete capsulotomy and lens fragmentation during
femtosecond laser-assisted cataract surgery associated with emulsified anterior
chamber silicone oil: a case report. Int J Ophthalmol
2019;12(6):1047-1049
Dear Editor,
I am Dr. Wei
Chen, from Department of Ophthalmology, Affiliated
Silicon oil
tamponade is widely used as an effective treatment for complicated cases of
ocular retinal diseases. However, silicone oils are not biodegradable and
associated with several undesired complications such as silicone oil
emulsification[1], cataract, glaucoma[2] and keratopathy[3].
Therefore, it is currently acknowledged that silicon oil should be evacuated as
soon as a stable situation in the retina has been achieved[4],
residual silicone oil droplets are not uncommon after silicone oil removal.
Usually, larger amounts of silicone oil entering the anterior chamber can
easily be found free to move in the anterior chamber. Sometimes, however, small
emulsified silicone bubbles in the anterior chamber are not easily observed
during routine slit-lamp examination.
Image-guided
FLACS has become increasingly more common within the past several years. The
laser can be used to perform the corneal incision, capsulotomy and lens
fragmentation. Importantly, the laser pulses and the integrated OCT imaging
system signal must pass through transparent media to work properly.
This study
was performed according to the Helsinki Declaration and informed consent was
obtained from the patient. This was a 41-year-old man who suffered from
unilateral cataract in the right eye. Two years earlier, he underwent pars
plana vitrectomy and silicone oil injection because of retinal detachment in
the eye and underwent silicone oil removal after 6mo. Preoperatively, best corrected
visual acuity (BCVA) was 1.0 logMAR OD. Intraocular pressure measured with
noncontact tonometer in the right eye was
At the time
of surgery, the patient was placed supine with head and eyes in primary gaze.
The eye was stabilized by docking it into the laser platform (Alcon-LenSx Inc.,
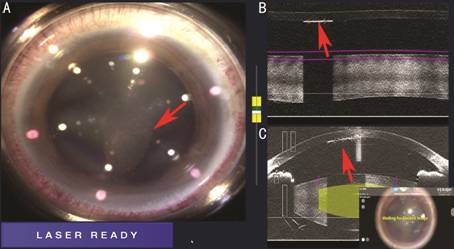
Figure 1
Intraoperative images of silicone oil droplets A: Intraoperative image showing
agminated silicone oil droplets underneath the cornea (red arrow); B, C:
Intraoperative sagittal AS-OCT view showing a retrocorneal line with
hyperreflectivity that is concerning for the emulsified silicone oil (red
arrow) and an underlying dark shadow due to the low OCT signal penetration.
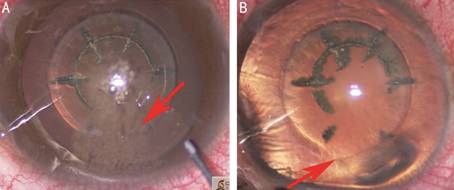
Figure 2
Incomplete capsulotomy and lens fragmentation caused by emulsified silicone oil
in the anterior chamber A: Intraoperative view showing
the emulsified silicone oil in the anterior chamber (red arrow). The droplets
floated in the aqueous humor and moved with changes in head position. B:
Intraoperative image showing an incomplete capsulotomy and lens fragmentation
(red arrow) in the area beneath the silicone oil after removal of the emulsified
silicone oil.
DISCUSSION
Intraocular
silicone oil is commonly used for complicated retinal detachments, trauma, and
severe proliferative diabetic retinopathy[5]. The
timing of emulsification is commonly based on the breakdown of the integrity of
the large silicone oil bubble into smaller bubbles. Silicone oil emulsification
is not an uncommon complication in long-term vitreous tamponade[6]. Several factors related to silicone oil emulsification
have been discussed in earlier papers[1,7-8]. The less viscous a substance, the lower the energy
that is required to disperse a large bubble of the substance into small
droplets. High viscosity silicone oil is less likely to emulsify. Silicone oil
viscosities now commonly used include 1000 and 5000 centistokes (cSt). While
higher-viscosity silicone oils are more resistant to emulsification, it is more
difficult to inject and remove them using small-gauge cannulas. Surface active
agents, which can decrease the liquor surface tension, may potentially aid
emulsification. Several intrinsic surfactants, such as serum, fibrin, fibrinogen,
and LDLs, present at higher levels in the perioperative setting, may increase
the risk of emulsification[8]. The largest factor
in silicone oil emulsification, however, is attributed to the duration of
tamponade. Toklu et al[9] reported a mean
time of 13.2mo (range, 5 to 24mo) of silicone oil emulsification in a
retrospective study in 32 eyes.
Silicone oil
tends to emulsify over time and can migrate into various locations within the
globe[10]. The droplets may migrate through
broken zonules into the anterior chamber, they will hide at the superior angle,
which is not easy to find by routine slit lamp inspection. In our case, there
are two reasons why emulsified silicone oil was not found in the anterior
chamber during slit lamp examinations: one is that silicone oil was not too
much to be visible, the other is negligence caused by opacity of the upper
cornea near the corneoscleral limbus. We also need to notice that emulsified silicone
oil may affect the IOL power calculations when we use A-scan ultrasound data.
Hence, patients who have an ocular surgery history of silicone oil
endotamponade are recommended to perform careful gonioscopy or AS-OCT of the
superior angle before FLACS.
In this
case, the AS-OCT images showed a hyperreflective line along the endothelium. It
was approved that the hyperreflective line is the optical coherence features of
intraocular silicone oil emulsification during phacoemulsification, which is in
accordance with the report of Errera et al[11]
that identical hyperreflective spherical bodies were observed in the AS-OCT
after injection of emulsified silicone oil into the model rubber eyes. There
was no signal reflected under the retrocorneal hyperreflective area, implying
that emulsified silicone oil prevented penetration of AS-OCT signal.
Incomplete
capsulotomy and incomplete lens fragmentation in this case were associated with
failure of laser delivery prevented by emulsified silicone oil. Under normal
circumstances, laser beams are focused onto a target through the interface
between cornea and aqueous humor. When emulsified silicone oil enters the
anterior chamber, the different refractive indices of the cornea, aqueous humor
and emulsified silicone oil may lead to laser light scattering or a wrong laser
focus. Inadequate laser energy resulted in incomplete capsulotomy and
incomplete lens fragmentation.
In
conclusion, thorough examination of eyes with a history of silicone oil endotamponade
is necessary before FLACS including careful gonioscopy or AS-OCT imaging of the
superior angle to identify the presence of emulsified silicone oil in the
anterior chamber. If there is silicone oil in the anterior chamber, optical
measurement of the axial eye length will be more accurate than ultrasonic
examination. It is also critical to observe if there is retrocorneal
hyperreflective signal in AS-OCT image before laser shot. Emulsified silicone
oil in the anterior chamber may result in incomplete capsulotomy and lens
fragmentation of FLACS.
Acknowledgements
Thanks to
the assistance of Ye-Meng Huang during the surgery.
Authors’
contributions: Chen W has
collected data and has been involved in drafting the manuscript. Wang Y has
collected data and helped revising the draft critically for important
intellectual content. Wu J has made substantial contributions in analysis and
interpretation of data and revising the draft critically for important
intellectual content. Guan HJ contributed to data analysis and interpretation
and helped revising the draft critically for important intellectual content.
All the authors read and approved the final manuscript and agreed to be
accountable for all aspects of the work in ensuring that questions related to
accuracy or integrity of any part of the work are appropriately investigated
and resolved.
Foundations:
Supported by
Technology and Science Foundation of
Conflicts of
Interest: Chen W, None; Wang Y, None; Wu J, None; Guan HJ, None.
REFERENCES