
Citation: Wang JX, Li YL, Gao YM, Zhang LN, Huang LP, He QH, Xie
HM, Jiang TY, Jia ZS, Wang XL. Radiofrequency ablation micro-dissecting
of eyelid nevus with XL-RFA device under operating microscope. Int J
Ophthalmol 2019;12(7):1116-1121
DOI:10.18240/ijo.2019.07.10
·Clinical Research·
Radiofrequency ablation micro-dissecting of eyelid nevus with XL-RFA device under operating microscope
Jing-Xin Wang1,2, Yi-Lan Li2, Yue-Ming Gao3, Li-Ning Zhang3, Li-Ping Huang3, Qing-Hua He4, Hui-Min Xie3, Tian-Yu Jiang3, Zi-Shan Jia3, Xing-Lin Wang3
1Medical School of Chinese PLA, Beijing 100853, China
2Department of Rehabilitation, Zhengzhou Central Hospital Affiliated to Zhengzhou University, Zhengzhou 100853, Henan Province, China
3Rehabilitation Medicine Center, the 1st Medical Center, Chinese PLA General Hospital, Beijing 100853, China
4Department of Ophthalmo-center, Chinese PLA General Hospital, Beijing 100853, China
Correspondence to: Xing-Lin Wang and Zi-Shan Jia. Rehabilitation Medicine Center, the 1st Medical Center, Chinese PLA General Hospital, Beijing 100853, China. WangXL0620@126.com; jia12323jia@163.com
Received:
Abstract
AIM: To study the effect of an innovative micro-dissection procedure by radiofrequency ablation (MRA) in removing eyelid nevus.
METHODS: Fifty-six consecutive outpatients with eyelid nevus were treated with MRA using a monopolar device. The effect of MRA was determined after following-up for 6mo to 5y.
RESULTS: Fifty-two cases (52 eyes, 92.9%) were cured once, and 4 cases (4 eyes, 7.1%) received second treatment for small residual. All cases healed well after surgery, with no pigmentation, no scars, no loss of eyelashes, no deformation of eyelid margin. There was no visual impairment after healing.
CONCLUSION: MRA of eyelid nevus using the XL-RFA device is highly efficient without significant complications.
KEYWORDS: radiofrequency ablation; micro-dissecting; eyelid nevus
DOI:10.18240/ijo.2019.07.10
Citation: Wang JX, Li YL, Gao YM, Zhang LN, Huang LP, He QH, Xie HM, Jiang TY, Jia ZS, Wang XL. Radiofrequency ablation micro-dissecting of eyelid nevus with XL-RFA device under operating microscope. Int J Ophthalmol 2019;12(7):1116-1121
INTRODUCTION
Eyelid nevus is a type of neoplasm. The main contents are nevus cells, the most of which was melanocyte[1]. The nevus is located either subdermal or a pigmented growth on the skin. Melanin is responsible for their dark color. The cause is not clearly understood. Sunlight and hormones maybe another two factors which may cause nevus. The prevalence of eyelid nevus in Asian population ranged from 8.6% to 12.1%[2].
Because of the troublesome location and affecting facial beauty caused by eyelid nevus, patients usually seek for a removal of it. The common procedures to remove the eyelid nevus are surgical excision and laser treatment. However, they are generally not well-accepted by patients. Surgery is a common ophthalmology, but surgical excision of eyelid nevus has some difficulties and may pose some risks, such as defect and deformation of eyelid margin. Postoperative complications may include deformation caused by eyelid margin defect or scar formation. The laser treatment, with low controllability, prone to induce massive collateral injury, including deformation, corneal damage and eyelash loss, etc[2].
Radiofrequency ablation has been used in many minimal invasive procedure. For example, it was used to eradicate arrhythmia in heart diseases. Radiofrequency ablation has different effects under various temperature. It causes contacting tissue molecular oscillation by electromagnetic wave passing through the treatment electrode. It has a good hemostatic effect on the ablated tissue. Radiofrequency ablation has been shown to have multiple advantages over traditional operational methods with feasibility of accurate control, less collateral damage and limited complications. The technique has been used in treating venous malformation[3, 4], knee osteoarthritis[5] palpebral margin neoplasm[6] and periorbital syringomas[7]. But till now, no studies reported the effectiveness of radiofrequency ablation in eyelid nevus treatment. In present study, we aimed to examine the efficacy of the innovative radiofrequency ablation device in the removal of eyelid nevus.
SUBJECTS AND METHODS
Ethical Approval All participants gave informed consent to take part in the study. The study protocol was approved by the Institutional Review Board of Chinese PLA General Hospital (No.413EG642) and was conducted in accordance with the Declaration of Helsinki.
Subjects A total of 56 patients from the Clinic of Ophthalmology and Rehabilitation in Chinese PLA General Hospital from 2013 to 2018 were recruited. The inclusion criteria are as followed: 1) diagnosed eyelid nevus; 2) informed consent form signature confirmed. The exclusion criteria are 1) obvious diseases which may affect ablation; 2) combined other eye diseases. The characteristics of the disease’s distribution and size were collected. The characteristic information including age and gender, etc, was recorded. A digital camera was used to take photos of lesion locations prior and posterior to treatment. Among the 56 included subjects, 10 were male and 46 were female. Their age ranged from 11 to 71y, with an average of 39.9y. The course of disease varied from 2 to 51y, with an average course of 21.4y.
Treatment Device Patients were treated with a monopolar device (XL-RFA device invented by Xing-Lin Wang from Chinese PLA General Hospital). The instrument has been authorized by State Food and Drug Administration of China (CFDA; No.2250584). The radiofrequency electrodes aligned with eyelid nevus, removed the lesions and melanocytes from the nevus nest along the border of diseased tissue by micro-dissection radiofrequency ablation (MRA) technique.
Treatment Protocol The 5% iodophor conventionally disinfected the skin, and 2% lidocaine was used for infiltration anesthesia. The treatment was performed under 2.5 loupe magnifications using XL-RFA device. During the process, the operators can observe whether there was any residue, whether the radian of margin was smooth, and removing the lesion into bottom to firm a solidified protective layer. Besides, some tissues were taken with tweezers for pathological examination. After the first treatment, the patients were informed of postoperative precautions, such as keeping the wound clean and waiting for natural healing after crust falling off. The residue was removed again in selected days.
Therapeutic
Evaluation The curative effect was divided into
5 categories: recovered, markedly improved, effective, failed and aggravated.
The standards were as followed: 1) recovered: the eyelid nevus completely
disappeared with the normal palpebral margin, no scars and no recurred in the
next 3mo; 2) markedly improved: the eyelid nevus disappeared with a defect <
RESULTS
Distribution
of Eyelid Nevus Of the 56 patients (56 eyes), 32
cases were in the right side and 24 cases in the left; 21 cases in upper
eyelid, 35 cases in lower eyelid. Male patients accounted for 17.9%. The mean
age was 40.4±7.5y in men and in 39.8±12.5y in women. Only one case had inner
canthus eyelid nevus. The lesion sizes were different. There were 38 cases with
diameter less than
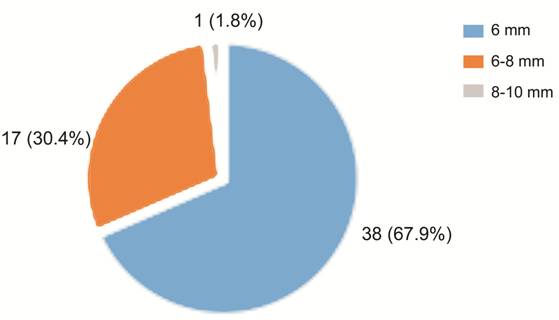
Figure 1 The distribution of eyelid nevus size.
Table 1 Summary of results
Patient |
Age (y) |
Sex |
Location of margin |
Size (mm2) |
CD (y) |
Cross gray line and mucosa |
Follow-up (y) |
Once cured |
1 |
20 |
F |
Right-upper |
5×4 |
20 |
N |
0.2 |
Y |
2 |
48 |
F |
Right-upper |
8×5 |
30 |
N |
0.2 |
Y |
3 |
32 |
F |
Left-upper |
3×3 |
20 |
N |
1 |
N |
4 |
58 |
M |
Right-upper |
6×3 |
20 |
N |
5 |
Y |
5 |
43 |
M |
Right-upper |
6.5×5 |
20 |
N |
1 |
Y |
6 |
33 |
F |
Right-upper |
4.5×4 |
5 |
N |
1 |
Y |
7 |
43 |
M |
Left-lower |
1×2 |
20 |
N |
1 |
Y |
8 |
11 |
F |
Right-lower |
6.5×4 |
11 |
N |
1 |
Y |
9 |
43 |
F |
Right-lower |
2×2 |
20 |
Y |
1 |
Y |
10 |
36 |
F |
Right-lower |
2×2 |
36 |
Y |
1 |
N |
11 |
37 |
F |
Right-lower |
3×3 |
37 |
Y |
1 |
Y |
12 |
24 |
F |
Right-lower |
3×3 |
24 |
N |
- |
Y |
13 |
20 |
F |
Right-lower |
9×7 |
20 |
Y |
- |
Y |
14 |
34 |
F |
Right-lower |
3.5×3.5 |
34 |
N |
- |
Y |
15 |
38 |
F |
Left-lower |
1.5×1.5 |
24 |
N |
- |
Y |
16 |
32 |
M |
Left-upper |
5×5 |
10 |
N |
- |
Y |
17 |
46 |
F |
Right-lower |
6×6 |
20 |
Y |
- |
Y |
18 |
33 |
F |
Right-lower |
7×5 |
33 |
N |
- |
Y |
19 |
42 |
F |
Right-upper |
6×3 |
42 |
N |
- |
Y |
20 |
39 |
M |
Right-lower |
7×7 |
39 |
N |
- |
Y |
21 |
46 |
F |
Right-upper |
4×4 |
10 |
N |
2 |
Y |
22 |
58 |
F |
Left-lower |
7×5 |
40 |
N |
2 |
N |
23 |
29 |
F |
Left inner canthus |
5×5 |
25 |
N |
2 |
Y |
24 |
51 |
F |
Left-lower |
7×5 |
51 |
N |
1.1 |
Y |
25 |
37 |
F |
Left-upper |
7×5 |
37 |
N |
2 |
Y |
26 |
37 |
F |
Left-lower |
5×5 |
10 |
N |
2.5 |
Y |
27 |
43 |
F |
Right-lower |
2×1.5 |
30 |
Y |
2.5 |
Y |
28 |
69 |
F |
Right-lower |
7×4 |
14 |
N |
- |
Y |
29 |
71 |
F |
Right-lower |
3.5×2.5 |
10 |
Y |
- |
Y |
30 |
34 |
F |
Left-lower |
4×3 |
30 |
N |
- |
Y |
31 |
25 |
F |
Right-lower |
2×2 |
20 |
Y |
- |
Y |
32 |
44 |
M |
Left-lower |
4.5×3.5 |
10 |
N |
- |
Y |
33 |
42 |
F |
Right-upper |
4×3 |
6 |
N |
- |
Y |
34 |
62 |
F |
Left-lower |
4×3 |
20 |
N |
- |
Y |
35 |
40 |
F |
Left-lower |
4×2 |
21 |
N |
- |
Y |
36 |
35 |
M |
Left-lower |
4×2 |
20 |
Y |
5 |
Y |
37 |
41 |
F |
Right-upper |
4×3 |
6 |
N |
5 |
Y |
38 |
38 |
F |
Right-upper |
6×4 |
20 |
N |
- |
Y |
39 |
27 |
F |
Right-lower |
5×5 |
20 |
Y |
5 |
N |
40 |
48 |
F |
Right-lower |
4×2.5 |
8 |
Y |
3 |
Y |
41 |
30 |
F |
Left-upper |
6×4 |
10 |
N |
5 |
Y |
42 |
58 |
F |
Left-upper |
5×4 |
20 |
N |
5 |
Y |
43 |
44 |
M |
Left-lower |
3.5×3.5 |
40 |
N |
1.7 |
Y |
44 |
37 |
F |
Left-upper |
5×3.5 |
18 |
N |
3 |
Y |
45 |
43 |
F |
Left-lower |
4×3.5 |
28 |
Y |
0.25 |
Y |
46 |
42 |
F |
Left-lower |
7×4 |
42 |
Y |
5 |
Y |
47 |
50 |
F |
Right-upper |
8×5 |
50 |
Y |
5 |
Y |
48 |
42 |
F |
Right-upper |
4×3 |
10 |
N |
5 |
Y |
49 |
56 |
F |
Right-lower |
3×3 |
10 |
N |
1 |
Y |
50 |
31 |
M |
Right-lower |
3.5×2.5 |
2 |
Y |
- |
Y |
51 |
26 |
F |
Right-lower |
3×2.5 |
2 |
Y |
- |
Y |
52 |
31 |
F |
Left-upper |
7×3 |
7 |
N |
- |
Y |
53 |
43 |
F |
Left-upper |
4×4 |
8 |
N |
2 |
Y |
54 |
35 |
M |
Left-upper |
3×3 |
35 |
N |
- |
Y |
55 |
41 |
F |
Left-lower |
3×3 |
5 |
Y |
- |
Y |
56 |
26 |
F |
Right-lower |
3×3 |
20 |
N |
5 |
Y |
CD: Course of disease.
Effect of MRA Treatment Fifty-two cases (52 eyes, 92.9%) were cured once, and 4 cases (4 eyes, 7.1%) had a small residual after first treatment for whom a retreatment was sorted. One case was remarkable once, but one case recurred. The first cure rate was 92.9%. After MRA, the pain of affected eyelids was not obvious. After the treatment, the wounds became scarred next day, and healed with scars fell off after 7 to 15d. No infection occurred, and no cases of malignant transformation due to MRA were found during follow-up. The mean follow-up time was 2.5y (0.2-5y). All cases healed well after surgery, with good eyelid radian, no obvious side effects, including defect and deformation of margin, scars, loss of eyelashes, deformation of eyelid margin, visible removal after healing, corneal epithelial injury. The results of pathological biopsy were intradermal nevus, mixed nevus and pigmented nevus. No malignant lesions were found (Figure 2).
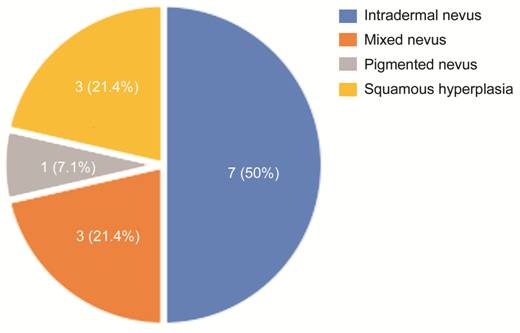
Figure 2 The distribution of eyelid nevus pathological biopsy.
Typical Cases
Case 1: Eyelid nevus on lower right A
48-year-old woman presented with eyelid nevus on the lower right palpebral
margin, size: 4.0×2.5-mm2, crossed the gray line and involved in
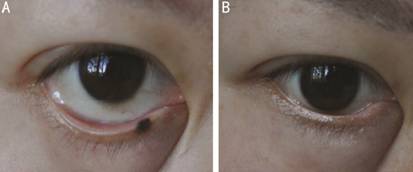
Figure 3 Clinical appearance in patient No.40 before and after treatment A: Before the treatment, the size of eyelid nevus (right-lower) was 4.0×2.5-mm2; B: After treatment, the eyelid nevus completely removed.
Case 2: Eyelid nevus on lower left A
51-year-old woman presented with eyelid nevus on the lower left palpebral
margin, size: 7×5-mm2, crossed the gray line (Figure
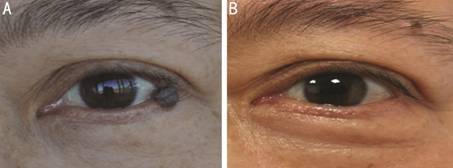
Figure 4 Clinical appearance in patient No.24 before and after treatment A: Before the treatment, the size of eyelid nevus (left-lower) was 7×5-mm2; B: After treatment, the eyelid nevus completely removed.
Case 3: Eyelid nevus on upper left A
43-year-old woman presented with eyelid nevus on the upper left palpebral
margin, diameter:
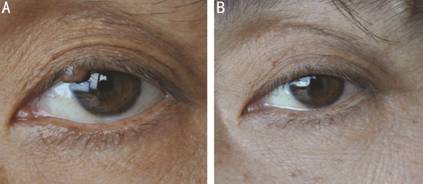
Figure 5 Clinical appearance in patient No.53 before and after treatment A: Before the treatment, the diameter of
eyelid nevus (left-upper) was
DISCUSSION
The eyelid
margin is a fibrous arc-like structure which plays an important role in
maintaining human appearance. As a transition zone between skin and mucosa,
eyelid margin is also a common site of orbital lesion. The thickness of the
eyelid nevus is about
In the removal of eyelid nevus, some scholars have used CO2 laser treatment[8]. CO2 laser treatment has the advantages of simplicity and effectiveness. But location of lesion’s removal during operation relies on visible light control but with poor controllability and low precision. Surgeons are required to wear protective glasses because of flashed light and smoke during laser treatment and it is easy to have residue and complications[10, 11, 12, 13]. Domestic researchers have reported about the curative effect using high-energy ultra-pulsed CO2 laser treatment on palpebral margin neoplasm. There were 2 cases of corneal damage while cured by treatment, 10 cases of eyelashes loss on the wound surface[14]. It has been reported that the use of laser for orbital plastic surgery can cause dry eyes. Eye dryness symptoms appear after laser treatment for 1wk to 4mo. Some patients with exposure keratopathy caused by laser treatment need surgical correction of orbital malformation and rabbit eye disease in order to significantly improve the symptoms of dry eyes[15]. Hammes et al[16] reported that the use of pulsed dye laser to treat wine cockroaches which did not protect the patient’s eyes and pupillary motor dysfunction and hypersensitivity to light appeared without completely relieved during 1y of observation. Therefore, surgeons and patients should wear protective lens to protect the eyes when removing eyelid lesions, and keep the laser at a safe distance from the eyeball during laser treatment. Hence, it is a challenging procedure to remove eyelid nevus for surgeons.
Radiofrequency ablation has the advantage of surgery, namely makes the excision controlled under the microscope to become a micro-dissection[17]. Therefore, we have combined ablation and micro-dissection to create MRA technique to remove the eyelid nevus, which avoiding the above-mentioned side effects, and significantly increasing patients’ acceptance and satisfaction. Besides, radiofrequency ablation would not affect lacrimal punctum if near the lesion. Under microscope, the micro-cutting edge can be precisely ablated, and the damage is mild. Because the radiofrequency electrode contacts the tissue to produce ablation, it’s easy to control, and it causes no damage to adjacent untouched tissue, such as eyeball, which obviously improves the safety and accuracy of the operation. During the operation, the surgeon does not need to wear any protective glasses, and operations under surgical microscope could obviously improves the clarity of the visual field and make the operation more convenient[18]. At the same time, radiofrequency ablation avoids suture and its associated adverse post-operation complications.
The grayish
white line in the middle of eyelid margin is gray line, which divided the
margin into front and back lip. It is common that the lesion involves gray
line. The mucous membrane involvement which cross the gray line means that the
lesion grows on the gray line and involves in the mucosa. In the present study,
17 cases had lesions crossed the gray line and mucosa. The total number of
patients with gray line infiltration was 49 which accounted for 87.5%. Nine
cases involved in 1 to
The eyelid
nevus usually has melanocyte nest infiltrated into margin, and this part of
melanocytes has high activity. It is easy to relapse if removal is incomplete.
Generally, the eyelid nevus is only about
A 12-year-old child we treated had a recurrence due to the incomplete removal of melanocyte nests. Since the child was developed unstably, we considered the recurrence was derived from regenerated pigmented nevus. No suture was needed after the treatment. No ischemia happened with tension caused by suture. No local blood was affected. Thus, MRA technique can ensure nutrition support to regenerate tissues and avoid local scar hyperplasia. The therapeutic effect after follow-up was no visible removal after healing. Therefore, MRA technique using XL-RFA device can eliminate the pathological tissue with minimal damage[14].
Other physical ways such as laser can also cause recur even if small pigmented nevus removed. The reason is that some pigmented nevus has a melanocytes nest that protrudes into or lies on the dermis. If the melanocyte nest is not completely eradicated, the pigmented nevus will recur[19, 20]. Repeated laser treatment has the potential of malignance. Therefore, it’s not strongly recommended to remove pigmented nevus using laser. Because of the special location and large damage to eyelid nevus, it is easy to cause defect of eyelid margin and scar healing. Methods such as laser have low precision and have no effects on removing melanocyte nests during treatment, which may lead to recurrence. However, MRA technique assisted by microscope, without flashed light and smoke, can provide the surgeon with good vision on the depth of the pigmented nevus and render a precise ablation and removal of the root and edge of pigmented nevus, which enjoy significant advantages over laser removal. Some large pigmented nevi protrude from the eyelid margin, and there may be abundant blood supply under the skin. It is easy to bleed when removed. However, the MRA technique could prevent bleeding of the wound surface and enable a solid layer protection. The visual field was clear, and only one patient recurred in 56 patients (recurrence rate =1.85%).
The XL-RFA device has been used in our center for more than 10y. The technique has been used in treating many diseases, such as venous malformation[3], palpebral margin neoplasm[4] and periorbital syringomas[5]. MRA technique for removal of eyelid nevus has not been reported before. Reports abroad on facial treatment were mainly about non-ablative methods for facial skin wrinkles, which can make skin younger[21]. Radiofrequency ablation technique was originally used for supraventricular arrhythmia treatment, and further developed for lumbar disc herniation, prostatic hypertrophy, tumor, etc. We have reported a single center experience about MRA technique using XL-RFA device to eradicate margin lesions and created a radiofrequency ablation microsurgery. Radiofrequency ablation microsurgery achieves the goal of precise and targeted eradication of lesions. It has multiple advantages, including short treating time, no bleeding during operation, mild collateral damage, forming protective layer on wound after treatment, rapid wound healing, no scar formation, disposable treatment electrode, no cross infection, which meet the need of clinical practice. Meanwhile, it is convenient during the whole operation process, and can accurately remove pathological tissues. Protective glasses are not warranted for the operators and patients. The postoperative inflammatory reaction was light. Therefore, radiofrequency ablation microsurgery can completely eradicate the eyelid nevus, and make patients achieve aesthetic appearance. Therefore, MRA technique is a highly accurate, practical and effective treatment in removing eyelid nevus, which possesses a potential of clinical recommendation. Further investigations regarding this innovative therapeutic approach is warranted.
ACKNOWLEDGEMENTS
Foundation: Supported by Health Department of
General Logistics (No
Conflicts of Interest: Wang JX, None; Li YL, None; Gao YM, None; Zhang LN, None; Huang LP, None; He QH, None; Xie HM, None; Jiang TY, None; Jia ZS, None; Wang XL, None.
REFERENCES