
DOI:10.18240/ijo.2019.07.25
Citation: Hua X, Dong Y, Wang L, Li Z, Du J, Chi W, Yuan X. Intraocular lens implantation performed first to protect the posterior capsule in Morgagnian cataracts during phacoemulsification. Int J Ophthalmol 2019;12(7):1215-1218
·Brief Report·
Intraocular lens implantation performed first to protect the posterior capsule in Morgagnian cataracts during phacoemulsification
Xia Hua1, Yongxiao Dong2, Ling Wang3, Zhiqing Li4, Jianying Du2, Wei Chi5, Xiaoyong Yuan6
1Department of Ophthalmology, the Second Hospital of Tianjin Medical University, Tianjin 300211, China
2Department of Ophthalmology, the First People’s Hospital of Xianyang, Xianyang 712000, Shaanxi Province, China
3Tianjin Medical University, Tianjin 300070, China
4Tianjin Medical University Eye Hospital, Tianjin 300384, China
5State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-sen University, Guangzhou 510060, Guangdong Province, China
6Tianjin Eye Hospital, Tianjin Key Laboratory of Ophthalmology and Visual Science, Clinical College of Ophthalmology, Tianjin Medical University, Tianjin 300020, China
Co-first authors: Xia Hua and Yong-Xiao Dong
Correspondence to: Wei Chi. State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-sen University, Guangzhou 510060, Guangdong Province, China. chiwei@mail.sysu.edu.cn; Xiao-Yong Yuan. Tianjin Eye Hospital, Tianjin Key Laboratory of Ophthalmology and Visual Science, Clinical College of Ophthalmology, Tianjin Medical University, Tianjin 300020, China. yuanxy_cn@hotmail.com
Received:
Abstract
This study evaluated the safety of a modified method to implant an intraocular lens (IOL) into the capsular bag immediately after capsulorhexis with a whole or partial nucleus to protect the posterior capsule (PC) during phacoemulsification in a series of 12 Morgagnian cataracts. For 3 cases of hypermature cataracts with smaller and rigid nuclei, after a complete capsulorhexis, an IOL was directly inserted into the capsular bag, which protected the PC during the subsequent phacoemulsification process in the iris plate. For the other 9 cases with larger and softer nuclei, after the nucleus was partially emulsified, the IOL was inserted into the bag. Even with an obvious surge for some cases, the surgeries were uneventful in all 12 cases, with no PC rent or vitreous loss. IOL implantation into the capsular bag with a whole or partial nucleus can provide effective protection for the PC for hypermature cataract during phacoemulsification.
KEYWORDS: intraocular lens; hypermature cataract; Morgagnian cataract; phacoemulsification; posterior capsule
DOI:10.18240/ijo.2019.07.25
Citation: Hua X, Dong Y, Wang L, Li Z, Du J, Chi W, Yuan X. Intraocular lens implantation performed first to protect the posterior capsule in Morgagnian cataracts during phacoemulsification. Int J Ophthalmol 2019;12(7):1215-1218
INTRODUCTION
Morgagnian cataracts are a challenge for almost all ophthalmic surgeons during phacoemulsification, as this type of cataract exhibits a fibrous anterior capsule, a liquid cortex, an expanding capsular bag, zonular weakness, and a hard nucleus[1-3]. Even with surgical expertise and caution, the loss of corneal endothelial cells, posterior capsule (PC) rupture, and related posterior complications are sometimes inevitable. Some experts have recently suggested the use of different techniques for these difficult cataract cases. These techniques include the visco-shell technique[4] and intraocular lens (IOL) scaffold technique[1], both of which have achieved satisfactory results. Here, we report our results using the IOL scaffold technique to protect the PC immediately after capsulorhexis with the whole nucleus or part of the nucleus phacoemulsified in a series of Morgagnian cataracts.
SUBJECTS AND METHODS
Ethical Approval This retrospective study was approved by the Ethics Committee of the First People’s Hospital of Xianyang, and all procedures were performed in accordance with the principles outlined in the Declaration of Helsinki.All patients signed an individual consent form before cataract surgery.
From January 1, 2016 to December 12, 2018, patients with a clinical diagnosis of Morgagnian cataracts based on slit lamp microscopy who underwent phacoemulsification with IOL implantation to protect the PC right after capsulorhexis or partial emulsification of nuclei were retrospectively reviewed.
After
topical anesthesia was applied, a 1-mm side port clear corneal incision was
made, followed by an injection of indocine green (ICG, 0.5%, Ruidu®,
Dandong, China) to stain the anterior capsule for 15s before it was replaced by
balanced saline solution. An ophthalmic viscosurgical device (OVD), 1.5% sodium
hyaluronate (Shanghai Qisheng Biological Agent Co., China), was used to fill
the anterior chamber. A 2.8-mm, 3-step, clear corneal incision was made at 90
degrees to the right of the side port incision. Capsulorhexis was initiated by
pinching the anterior capsule with forceps, and the liquid cortex was then
aspirated from the capsular bag with a 5 mL syringe. A 5.5-mm continuous
curvilinear capsulorhexis (CCC) was then performed with forceps. No
hydroprocesses were performed, and some of the OVD was injected into the
capsular bag to tilt the lens nucleus and provide more space between the
nucleus and the rim of the CCC. A 3-piece IOL was implanted with the assistance
of a Sinskey hook and a spatula to prolapse the lens nucleus into the anterior
chamber and to provide space for the IOL in the capsular bag. A venture system
phaco machine (Stellaris, Bausch & Lomb, Rochester, New York, USA) was set
to a smaller perimeter than normal and used at a vacuum pressure of
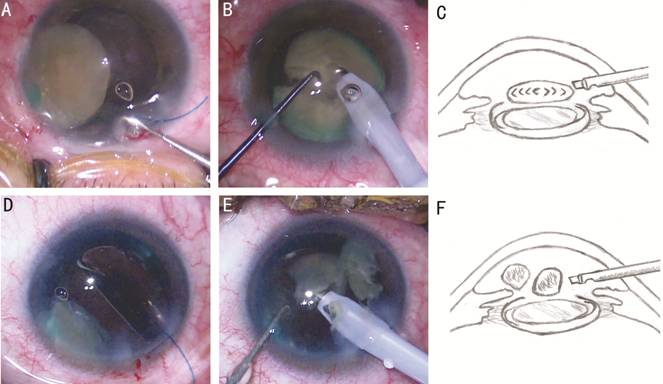
Figure 1 Diagram of IOL implantation first to protect the PC in Morgagnian cataract during phacoemulsification A: Insertion of the IOL into the capsular bag under a whole lens nucleus using a Sinskey hook; B: Phaco-chop of the whole lens nucleus performed in the iris plane after the IOL was placed in the bag to protect the PC; C: Schematic diagram of phacoemulsification of the whole nucleus in the iris plane with the IOL in the capsular bag; D: Insertion of the IOL into the capsular bag under a partial nucleus using a Sinskey hook; E: Phaco-chop of the partial nucleus performed in the iris plane after the IOL was placed in the bag to protect the PC; F: Schematic diagram of phacoemulsification of the partial nucleus in the iris plane with the IOL in the capsular bag.
For some
cases of hypermature cataracts, IOL was inserted into the capsular bag after
the partial nucleus was phacoemulsified. The routine procedures were performed
as mentioned previously, with the difference being the timing of IOL
implantation. In all the cases selected for this series, the anterior chamber
was shallow, and the pressure in the posterior chambers was increased. After
the integrity of PC was verified, the IOL was carefully inserted into the
capsular bag, as some pieces of nucleus could be found in the anterior chamber
or in the bag (Figure 1D
RESULTS
In total, 12 cases of Morgagnian cataracts with IOL to protect the PC were identified among 5500 routine phacoemulsification. Among these, the IOL was inserted into the capsular bag immediately after capsulorhexis and before phacoemulsification in 3 cases, and in the other 9 cases, the IOL was implanted after part of the lens nucleus was emulsified. On day one post-operation, some corneal edema with some folds in Decemet’s membrane was observed in most cases and resolved within 1wk. Temporarily high IOP was found in 3 eyes, which was controlled by tapping some of the aqueous, and resolved within 2d. In 2 eyes with uneventful surgery, obvious macular degeneration was found after surgery (Table 1).
Table 1 Clinical and demographic data of the cases of Morgagnian cataract
Cases |
Gender |
Age, y |
Right/Left |
VA (preop.) |
Timing of IOL implantation |
BCVA (1wk postop.) |
No.1 |
Male |
72 |
Right |
LP |
After the nucleus was partially emulsified |
20/25 |
No.2 |
Male |
68 |
Left |
LP |
After the nucleus was partially emulsified |
20/20 |
No.3 |
Female |
82 |
Left |
LP |
After the nucleus was partially emulsified |
20/40 |
No.4 |
Female |
77 |
Left |
HM |
After capsulorhexis |
20/25 |
No.5 |
Female |
64 |
Right |
HM |
After the nucleus was partially emulsified |
20/20 |
No
|
Male |
86 |
Right |
HM |
After the nucleus was partially emulsified |
20/200 |
No.7 |
Male |
69 |
Left |
LP |
After the nucleus was partially emulsified |
20/25 |
No.8 |
Male |
74 |
Left |
HM |
After the nucleus was partially emulsified |
20/25 |
No
|
Female |
74 |
Right |
HM |
After capsulorhexis |
20/200 |
No.10 |
Female |
73 |
Right |
HM |
After capsulorhexis |
20/25 |
No.11 |
Male |
73 |
Left |
LP |
After the nucleus was partially emulsified |
20/25 |
No.12 |
Male |
68 |
Left |
LP |
After the nucleus was partially emulsified |
20/32 |
VA: Visual acuity; IOL: Intraocular lens; BCVA: Best corrected visual acuity; LP: Light perception; HM: Hand motion. aObvious macular degeneration was observed after surgery.
DISCUSSION
Although the incidence of Morgagnian cataract is decreasing, it remains common in China, especially in rural and underdeveloped areas. Even when treated by experienced clinicians, the rate of surgical complications when treating this type of cataract is much higher than that when treating cataracts of other stages and types and can include shrinkage and fibrosis of the anterior capsule, weak zonules, a liquid cortex, an enlarged capsular bag, and a hard nucleus with indeterminate thickness[5-7]. Several groups have attempted to use the IOL as a shell to protect the PC during phacoemulsification[1,8]; this approach resulted in a lower incidence of PC rupture and nucleus drop into the vitreous cavity[9]. In addition, estimating the thickness of the hard nucleus was difficult, and therefore, we decided to insert the IOL into the capsular bag after capsulorhexis to protect the PC and perform a much safer phacoemulsification. Several points need to be addressed regarding this process.
For the 3
cases of hypermature cataracts, after successful capsulorhexis, we found that
the nucleus was as rigid as N5 and less than
For the
other 9 cases, we found that the nucleus was relatively large (above 5.5
As the IOL was in the bag, the whole or partial nucleus was emulsified in the iris plate. We found that in most cases the zonules were weak, and the setting of bottle height and vacuum were slightly lower than usual. Special care needed to be taken as the OVD was injected into the anterior chamber, lowering the speed at which the lens pieces were emulsified, especially the last piece, avoiding obvious surge during the surgery. Moreover, we used the bevel-down technique to attempt to limit the phaco energy to the nucleus rather than the cornea.
In conclusion, Morgagnian cataracts are a very difficult type of cataract to treat with surgery with a high incidence of complications. IOL implantation into the capsular bag can provide effective protection for the PC for a subsequent phacoemulsification and may increase surgical safety and produce satisfactory results, especially in cases with a hard nucleus with underdetermined thickness.
ACKNOWLEDGEMENTS
The authors would like to express their gratitude to the patients who participated in this study.
Foundations: Supported by National Natural Science Foundation of China (No.81570830, No.81670817); Key R&D Program Projects in Shaanxi Province (No.2017SF-273); the Tianjin Research Program of Application Foundation and Advanced Technology (No.17JCYBJC27200); the Science & Technology Foundation for Selected Overseas Chinese Scholar, Bureau of Personnel of China, Tianjin, and Talent Innovation Group of 131, Bureau of Personnel, Tianjin, Tianjin Science and Technology Project (Popularization of Science 17KPHDSF00230); Xi’an Science and Technology Project [No.2017116SF/YX010(1)].
Conflicts of Interest: Hua X, None; Dong Y, None; Wang L, None; Li Z, None; Du J, None; Chi W, None; Yuan X, None.
REFERENCES