
Citation: Zhang J, Ning XN, Yan H. Adjustment of IOL power for the second eye based on refractive error of the first-operated eye. Int J Ophthalmol 2019;12(8):1348-1350. DOI:10.18240/ijo.2019.08.18
·Brief Report·
Adjustment of IOL power for the second eye based on refractive error of the first-operated eye
Jie Zhang1, Xiao-Na Ning1, Hong Yan1,2
1Department of Ophthalmology, Tangdu Hospital, the Fourth Military Medical University, Xi’an 710038, Shaanxi Province, China
2Xi’an No.4 Hospital, Shaanxi Eye Hospital, Affiliated Guangren Hospital School of Medicine, Xi’an Jiaotong University, Xi’an 710004, Shaanxi Province, China
Correspondence to: Hong Yan. Department of Ophthalmology, Tangdu Hospital, the Fourth Military Medical University, No.569 Xinsi Road, Xi’an 710038, Shaanxi Province, China. yhongb@fmmu.edu.cn
Received:
Abstract
This study was to estimate refractive status of the second eye of those undergo bilateral cataract surgery based on the first-operated eye, and to evaluate the refractive error (RE) in the second eye after correcting 50% of the first-operated eye’s error when it exceeded ±0.50 diopter (D). In this prospective study, 80 patients were scheduled for cataract surgery in the second eye, who underwent cataract surgery in first eye 1-3mo previously. The RE of each eye postoperatively was determined according to SRK/T formula. When the first-eye refractive error (FERE) exceeded ±0.5 D, the intraocular lens (IOL) power of the second eye was adjusted 50% of the FERE. The second-eye refractive error (SERE) was measured 1mo after surgery. The FERE exceeded -0.50 D in 12 eyes (-0.675±0.16 D), and the adjusted SERE was -0.322±0.73 D (P<0.05). The FERE exceeded +0.50 D in 8 eyes (1.533±1.14 D), and the adjusted SERE was 0.168±1.36 D (P<0.05). The unadjusted SERE in 60 cases remained -0.38 to 0.42 D when the FERE within ±0.05 D. This prospective study confirmed that the prediction of the second eye could be improved by correcting 50% of FERE when this error exceeded ±0.50 D.
KEYWORDS: cataract surgery; refractive error; the first eye; the second eye
DOI:10.18240/ijo.2019.08.18
Citation: Zhang J, Ning XN, Yan H. Adjustment of IOL power for the second eye based on refractive error of the first-operated eye. Int J Ophthalmol 2019;12(8):1348-1350
INTRODUCTION
Precise intraocular lens (IOL) power calculation has been considered after cataract surgery because of reduction in incision size, refinement of IOL power formula, improvements in operative technique and IOL manufacture[1]. However, not every postoperative refractive outcome is within ±0.5 D even using the best biometry. One factor not considered is the relationship between the sequential two operated eyes’ refractive outcomes, especially if the target refractive outcome was not achieved in the first operated-eye[2]. The use of anterior chamber depth (ACD) obtained in postoperative measurement of the first operated-eye to calculate the IOL power of the second eye was reported to be beneficial for the accuracy of calculation[3]. Several studies suggested that the deviation of the first-eye refractive error (FERE) could be applied to improve the refractive outcomes of the second eye in bilateral cataract surgery[4-5]. In early 2010 Covert et al[2] discovered that theoretical refractive outcomes of the second eye could be improved by correcting 50% of the error from the first eye in 206 patients by using Holladay I and SRK II formula. In our prospective study, we try to test the hypothesis that the refractive error (RE) in the second eye was adjusted to correct for 50% of the first-operated eye’s error if it exceeded ±0.50 D.
SUBJECTS AND METHODS
Ethical Approval The study followed the principles of the Declaration of Helsinki. The research was in accordance with Guideline of Chinese GCP and ICH-GCP, and was approved by the Institutional Review Board of Tangdu Hospital, Fourth Military Medical University (TDLL-2014038). Informed consent was obtained from all patients for cataract surgeries and the IOL power calculation and adjustment.
Inclusion criteria included patients who underwent bilateral phacoemulsification and IOL implantation in Tangdu Hospital from May 2015 to May 2016. The same IOL model was implanted in both eyes using IOL Master (Version 5.5, Carl Zeiss, Germany). Both axial length (AL) and corneal curvature (K) were measured preoperatively using IOL Master. Patients with corneal pathologic features, corneal astigmatism of >3.00 D, extreme myopia and hyperopia, retinal diseases, undergoing trabeculectomy, pas plana vitrectomy were excluded.
The 80
consecutive patients were scheduled for cataract surgeries for the second eyes,
whose first eyes underwent cataract surgeries 1-3mo previously. The procedures
of phacoemulsification and IOL implantation were performed by only 1 surgeon
(Yan H). The SRK-T formula was chosen to calculate IOL power, as the AL of all
eyes was within normal range (22
Statistical Analysis Data were analyzed using SPSS (version 17.0, USA). The differences were compared using Chi-square test. P<0.05 was considered statistically significant.
For example: Female, 70 years old.
OD: -1.00 DS/-0.50 DC×10=0.4 (0.3), the spherical equivalent value: -1.25 D
OS: -0.50 DS/-0.75 DC×10=0.2 (0.1), the spherical equivalent value: -0.875 D
Axial
length: OD
SRK-T formula was chosen to calculate IOL power for the left eye. Bausch & Lomb ADAPT-AO IOL power of +23.5 D with the target postoperative refraction of -0.57 D was implanted in the left eye. The left eye RE was evaluated 1mo postoperatively.
OS: +0.25 DS/+0.50 DC×20=0.9 (0.6), the spherical equivalent value:+0.50 D
The RE of the left eye: +0.50 D –(-0.57 D)= +1.07 D
For the right eye, the 50% adjustment of IOL power means its refractive target should be calculated by subtracting 0.535 D (half of +1.07 D) from the predicted refraction.
RESULTS
In our previous study, we investigated the RE exceeded ±0.5 D in 40 eyes (32.3%) in 124 first-operated eyes (Figure 1).
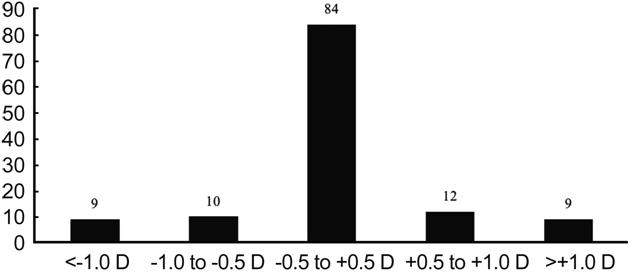
Figure 1 The RE was investigated in 124 eyes.
In the
prospective study, 80 patients were included, the mean age was 69±12y (range
55-79y), with an even sex distribution (45% men vs 55% women). The AL of
all eyes ranged from 22.08 to
The FERE was more than -0.50 D in 12 eyes. The FERE was -0.675±0.16 D, and the median was -0.625 D. After correcting 50% of FERE for the IOL power of the second eye, the aSERE was -0.322±0.73 D, and the median was -0.02 D (P<0.05). It showed that the 50% adjustment improved the RE of the second eye (Table 1).
Table 1 aSERE in 12 eyes when the FERE exceeded -0.50 D D
Parameters |
Mean±SD |
Median |
Within ±1 D |
FERE |
-0.675±0.16 |
-0.625 (-0.55 to -1.13) |
10/12 |
aSERE |
-0.322±
|
-0.02 (-1.92 to 0.16) |
10/12 |
aP<0.05.
The FERE was more than +0.50 D in 8 cases. After correcting 50% of FERE for the IOL power of the second eye, the FERE was 1.533±1.14 D, and the median was 1.125 D. The aSERE was 0.168±1.36 D, and the median was 0.18 D (P<0.05; Table 2).
Table 2 aSERE in 8 eyes when the FERE exceeded +0.50 D D
Parameters |
Mean±SD |
Median |
Within ±1 D |
FERE |
1.533±1.14 |
1.125 (0.77 to 3.19) |
4/8 |
aSERE |
0.168±
|
0.18 (-1.51 to 1.82) |
4/8 |
aP<0.05.
The 60 cases of second eyes remained the same when the FERE within ±0.05 D (Table 3).
Table 3 SERE in 60 cases when the FERE within ±0.50 D D
Parameters |
Mean±SD |
Median |
Within ±1 D |
FERE |
-0.084±0.28 |
-0.13 (-0.38 to 0.42) |
60/60 |
SERE |
-0.079±0.25 |
-0.16 (-0.33 to 0.46) |
60/60 |
DISCUSSION
Surgeons should consider the refraction of the first eye into designing the targeted refraction for the second eye. REs after cataract surgery are mainly due to lacking of correct preoperative estimation of the accurate postoperative IOL position and ACD[4,6]. There are also unexpected and uncontrollable prediction errors which derived from measurement errors and individual anatomical conditions. The refractive outcomes after cataract surgery of the first eye are associated with the second eye[1-3]. Covert et al[2] were the first to discover the IOL power calculation of the second eye could be improved by using the first eye data. Jabbour et al[5] found that a full adjustment of the first-eye error couldn’t improve predicted refraction of the second eye through 121 sequential cataract surgery cases. Partially adjusted method was proposed, and the refractive outcomes were proved to have a smaller aSERE than unadjusted or fully aSERE. It has been indicated that partial adjustment by 50% would gain the best prediction accuracy for the second eye[1-2,5,7]. This is similar to our study that, the FERE exceeded ±0.5 D, the second-eye results could be improved by adjusting partially for the error in the first eye.
The SRK-T formula is commonly chosen to calculate IOL power before cataract surgery, which could perform satisfying accurate outcomes[1,8]. However, it still could be significantly improved by adjusting predicted IOL power based on the first eye’s error. Our study verified that there is a possibility to ameliorate the prediction of the second eye from the first eye’s calculated with SRK-T formula, if this error exceeded ±0.5 D, which confirmed the previously published data[6]. Covert et al[2] also found a partial adjustment could lead to a significant improvement in 206 patients using Holladay I and SRK II formula. Because those patients with corneal astigmatism of >3.00 D, extreme myopia and hyperopia were excluded in this study, the limitation of this study is that only one formula was used. These data might be limited to the Hoffer Q formula, Haigis formula, etc[9-12]. Further studies will be required in the future.
Our prospective study implied that it would be beneficial to improve the final refractive result in the second eye by substituting half of the error of the first eye into the calculation.
ACKNOWLEDGEMENTS
Foundation: Supported by Natural Science Foundation of China (No.81300743)
Conflicts of Interest: Zhang J, None; Ning XN, None; Yan H, None.
REFERENCES