
Citation: Toto L, Viggiano P, Vecchiarino L, Evangelista F,
Borrelli E, Mastropasqua L. Anterior capsule contraction syndrome: a successful
multimodal therapeutic approach. Int J Ophthalmol 2019;12(8):1356-1358. DOI:10.18240/ijo.2019.08.20
·Letter to the Editor·
Anterior
capsule contraction syndrome: a successful multimodal therapeutic approach
Lisa Toto, Pasquale Viggiano, Luca Vecchiarino, Federica
Evangelista, Enrico Borrelli, Leonardo Mastropasqua
Ophthalmology
Clinic, Department of Medicine and Science of Ageing, University G. D’Annunzio
Chieti-Pescara, Chieti 66100, Italy
Correspondence
to: Pasquale
Viggiano. Ophthalmology Clinic, Department of Medicine and Science of Ageing,
University G. D’Annunzio Chieti-Pescara, Chieti 66100, Italy.
pasquale.viggiano90@gmail.com
Received:
DOI:10.18240/ijo.2019.08.20
Citation: Toto
L, Viggiano P, Vecchiarino L, Evangelista F, Borrelli E, Mastropasqua L.
Anterior capsule contraction syndrome: a successful multimodal therapeutic
approach. Int J Ophthalmol 2019;12(8):1356-1358
Dear Editor,
I am Dr.
Lisa Toto, from Department of Medicine and Science of Ageing, University G.
D’Annunzio Chieti-Pescara, Chieti, Italy. I write to present a case report of
anterior capsule contraction syndrome (ACCS).
ACCS is a
condition that can occur after cataract surgery and intraocular lens (IOL)
implantation[1]. This disorder is secondary to an excessive contraction
and fibrosis of the spared anterior capsule, which may result in the
obstruction of the visual axis, or alternatively may cause late complications
to the IOL, including pseudophacodonesis and IOL tilt, decentration, or
dislocation[1]. Several approaches have been used to treat this condition such as the use
of Nd:YAG laser or through surgical treatment. In this case report we propose a
multimodal therapeutic approach to successfully solve this post-surgical
complication.
A
51-year-old woman was referred to our department presenting with blurred vision
in her left eye (LE) for one week. The patient underwent cataract surgery with
phacoemulsification and IOL implantation in the capsular bag two months before.
A Zeiss CT ASPHINA 404 [aspheric Hydrophilic acrylic (25%) IOL with hydrophobic
surface, Carl Zeiss Meditec Inc., Germany] IOL (-06 diopters) for emmetropia
was successfully implanted in the capsule with 360° overlapping of capsular
edge onto the anterior IOL optic surface. All surgical procedures were
uneventful. The same IOL was implanted about two months earlier in the RE.
Furthermore, the two eyes were known to be affected by high myopia (axial
length of
At
presentation, best-corrected visual acuity (BCVA) was 0.0 and 1.0 logMAR in her
RE and LE, respectively. Slit lamp anterior segment examination of the LE revealed
anterior capsule fibrosis occluding the visual axis (Figure
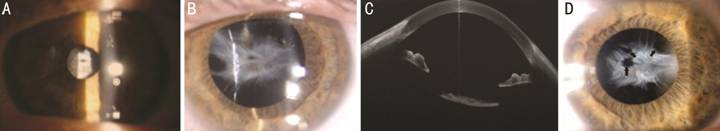
Figure 1
Capsule phimosis with complete occlusion of the optical zone due to an
excessive contraction and fibrosis of the spared anterior capsule A, B: Slit lamp segment anterior
photography of the left eye in miosis and midriasis; C: AS-OCT showing capsular
fibrosis adherent to the anterior surface of the IOL; D: Slit lamp segment
anterior photography of the left eye after using Nd:YAG laser to create three
holes into the fibrotic material (black arrows).
The
therapeutic approach to resolve this disease was divided in three complementary
and following phases. The first (or preoperative) phase was completed using a
Nd:YAG laser to create three holes into the fibrotic material (Figure 1D). The
energy was 3.2 µJ. During the second phase a dispersive ophthalmic
viscosurgical device (OVD) (IAL-f) [distributed by TRB Chemedica (Thailand)
Ltd.] was injected between the anterior capsule and the IOL optic to increase
the space between them although the three holes and under this patch to protect
the IOL. The third phase was performed using a femtosecond laser: the CATALYS
Precision Laser System (Abbott Medical Optics, Inc., Santa Ana, CA, USA). It
combines pulses of less than 600 femtosecond laser, gentle liquid optics
interface, and integrated 3D Full Volume Optical Coherence Tomography (OCT)
image-guidance system to create precise incisions in the lens and cornea.
During this phase, the patient’s eye was properly docked to the system, a
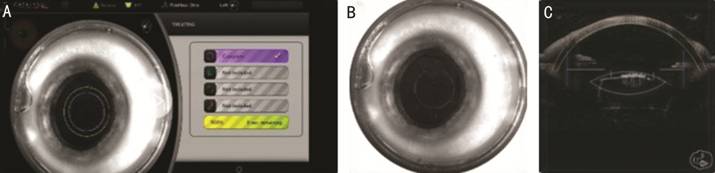
Figure 2
Phimosis excision A: The eye is docked to the laser,
and the capsulotomy (violet circle) is aligned on the center of the pupil and
includes the central part of the phimosis of the capsule; B: Completion of
capsulotomy treatment; C: Optical coherence tomography image of anterior
capsule phimosis in sagittal section; planned femtosecond laser incision.
At 1d
postoperatively, the BCVA was 0.7 logMAR in the left eye and the patient
reported a significant improvement of the visual symptoms. Both AS-OCT and
indirect ophthalmoscopy demonstrated a complete removal of the fibrotic
material (Figure 3). At the 1-week and 1-month follow-up visits, the BCVA was
0.4 logMAR and 0.2 logMAR, respectively, and both visual symptoms and clinical
alterations were completely resolved (Figure 3).
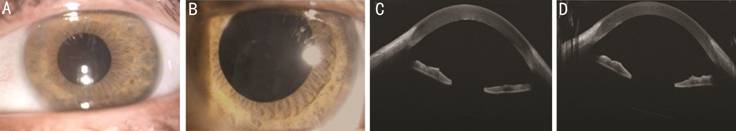
Figure 3 After multimodal therapeutic
approach Slit lamp segment
anterior photography of the left eye after capsulotomy femtosecond laser at
1-day follow-up visit (A) and at 1-month follow-up visit (B). AS-OCT at 1-day
follow-up visit (C) and at 1-month follow-up visit (D).
Although ACCS is a relatively
rare complication occurring after phacoemulsification, there are some cases
described in the literature.
The exact etiology of ACCS is not
well understood, however there are some risk factors[2]. associated with this disorder, including preexisting
systemic and ocular conditions (e.g. advanced age, diabetes mellitus,
Bechet’s syndrome, myotonic muscular dystrophy, zonular weakness, chronic
intraocular inflammation, PEX[3-4], retinitis pigmentosa, and high myopia)[1,4-5], a continuous curvilinear capsulorhexis (CCC) of small
size[1,6-7] and the IOL material and design, with silicone, acrylic,
plate haptic, and polyHEMA IOLs that have been associated with a higher rate of
ACCS. Our patient was thus characterized by some risk factors for ACCS,
including PEX[3,5], high myopia[5], and
acrylic IOL implantation[1,8-9].
The pathogenic process leading to
ACCS is poorly defined. Some authors speculated that a population of vital
crystalline epithelial progenitor cells (LECs), which may be still present on
the capsular bag even after cataract surgery, might differentiate into fibrous
cells. The metaplasia of these cells might be thus causative of the fibrosis
anterior to the IOL, which is hallmark of ACCS[2,7,10].
Although ACCS is frequently
asymptomatic, symptoms of ACCS may include painless, progressive blurred vision.
Advanced cases may be associated with glare, haloes, or monocular diplopia in
those cases ACCS causes IOL decentration.
ACCS was first reported by
Davison[1] who described
a case of anterior capsular fibrosis following cataract surgery. Since this
first description, several authors have tried to find the best approach to
either prevent or treat this complication.
In order to prevent ACCS
occurrence, Davison[1] first proposed YAG laser
relaxing anterior capsulotomies at 2 to 3wk after cataract surgery. This is
thought to reduce contracture of the anterior capsule and consequently reduce
the incidence of ACCS. Another preventing approach was proposed by Munoz and
Alio[11] who
introduced the use of capsular tension rings that maintain the round shape of
the capsular bag and prevent an excessive capsular shrinkage and fibrosis.
Therapeutic
approaches to ACCS are numerous. These include the use of YAG laser to open the
anterior fibrosis, as reported by Wilde et al[12] who described two cases where YAG
laser was performed in a continuous circular fashion to create a free-floating
fragment. However, after treatment, this fragment moved to the inferior part of
the anterior chamber and obscured vision during reading. In another previous
report, the authors[13] described a patient with ACCS
treated with a vitrector to create and remove a circular fibrotic flap[13]. Gerten et al[14] performed the first femtosecond
laser-assisted openings of a phimotic anterior capsules. They used the Lensx
femtosecond laser (Alcon Laboratories, Inc., USA) and this approach may offer
advantages especially in partial occlusion of anterior capsulorhexis.
In the current case we performed
a multimodal and combined therapeutic approach to solve ACCS. We showed that
this approach may be considered safe and effective. In particular, we believe
this may represent a valuable approach for at least three reasons. First, the
use of a conventional approach like Nd:YAG laser to create three holes into the
fibrotic material allowed for the successive injection of viscoelastic material
that protects the IOL during the surgical phase. Second, the employment of a
femtosecond laser yielded the creation of a circular fibrotic patch, which may
preclude recurrence and reduce the refractive changes (hyperopic shift,
internal astigmatism) introduced by the capsule phimosis. Finally, the surgical
removal of this patch led to absence of obstacle at reading. This multimodal
approach is characterized by more benefits respect to the conventional
approaches regarding complete occlusion of the optical zone. Using only Nd:YAG
laser has disadvantages, in particular a high emission of laser energy may
weaken the zonular fibers, break the posterior capsule, or destabilize the IOL
position, resulting in IOL dislocation. Although the femtosecond laser approach
seems to reach good results, in this case report the presence of a thick
capsule fibrosis adherent to the anterior surface of the IOL optic could make
difficult the planning of capsule incision and subsequent treatment without
avoiding damage of the IOL during laser treatment. The subcapsular injection of
OVD allowed the separation of the two planes id est capsule and anterior
IOL optic making laser procedure safer and efficient. In conclusion, in this
case report we provided a novel and multimodal strategy to resolve ACCS. This
strategy is safe and effective. If replicated in future studies, this
multimodal approach may prove to be a useful treatment for ACCS.
ACKNOWLEDGEMENTS
Conflicts of
Interest: Toto L, None;
Viggiano P, None; Vecchiarino L, None; Evangelista F, None;
Borrelli E, None; Mastropasqua L, None.
REFERENCES