
·Letter to the Editor·
Central
retinal artery occlusion after uneventful glaucoma valve implantation surgery
with retrobulbar anesthesia: a case report
Fang-Yu Lin, Ming-Shui Fu
Department
of Ophthalmology, Shanghai General Hospital, Shanghai 200080, China
Correspondence
to: Ming-Shui
Fu. Department of Ophthalmology, Shanghai General Hospital, Shanghai, No.100,
Haining Road, Hongkou District, Shanghai 200080, China. fumingshui@126.com
Received:
DOI:10.18240/ijo.2019.08.22
Citation:
Lin FY, Fu MS. Central retinal artery occlusion after uneventful glaucoma valve
implantation surgery with retrobulbar anesthesia: a case report. Int J
Ophthalmol 2019;12(8):1362-1365
Dear Editor,
I am Dr.
Fang-Yu Lin from the Department of Ophthalmology, Shanghai General Hospital,
Shanghai, China. I am writing to present to you a case of central retinal
artery occlusion after routine glaucoma valve implantation surgery with
retrobulbar anesthesia. Retrobulbar anesthesia has been extensively applied in
intraocular surgery for many years. It is generally considered a low risk
procedure. However, there is a possibility of retinal vessel occlusion, such as
central retinal artery occlusion (CRAO), a rare yet devastating complication
causing a sudden and permanent loss of vision. This refers to an acute ocular
vascular occlusive disorder with dramatic onset of painless vision loss. We
report a case of CRAO after uncomplicated glaucoma valve implantation surgery
with retrobulbar anesthesia.
A 17-year-old
boy with a history of congenital cataract, was found to have an intraocular
pressure (IOP) in the right eye of
The decision
to go forward with the surgery was made. Eye examination did not show any
vascular abnormalities prior to surgery, BCVA was 20/20 and IOP was
The next
day, his right visual acuity was hand motion, not improving with pinhole. IOP
in the right eye was
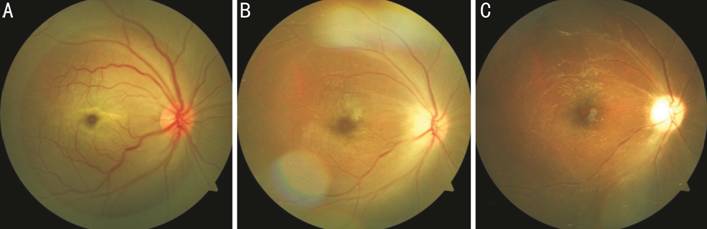
Figure 1 Fundus
photography showed cherry red spot with diffuse retinal edema on the first
postoperative day (A); Retinal edema subsided and optic disk was slightly pale
a week later (B); A pale optic disk with attenuated retinal veins and arteries
one month later (C).
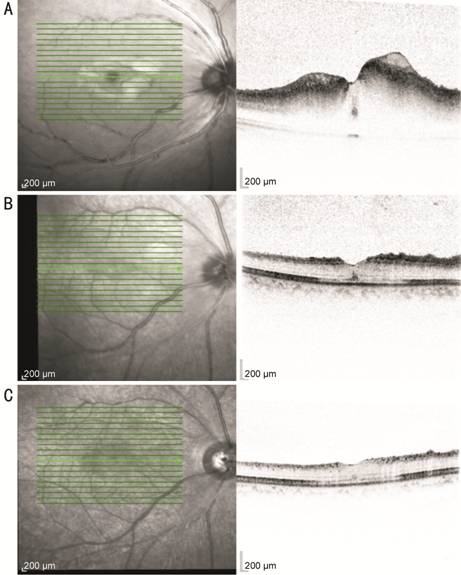
Figure 2
Macular region OCT scans showed retinal edema on the first postoperative day
(A) and edema gradually faded away one week (B) and one month later (C).
The patient
was urgently given a retrobulbar injection of 0.5 mg of atropine, oxygen
inhalation therapy, and 70 mg prednisone orally per day. As the patient noticed
only minimal improvement with the treatment, he was further administered
immediate 200 mg salvianolate with 250 mL normal saline and 5 μg alprostadil
injection with 20 mL normal saline treatment per day, and also 500 μg
methycobal with 20 mL normal saline twice a day. Carotid artery ultrasound and
color doppler echocardiography were performed and showed no abnormalities. The
patient was given extracorpored counterpulsation treatment with a pressure of
0.02 MPa per day.
Fundus
photography and the optical coherence tomography (OCT) examination showed most
of the retinal edema subsided but the optic disk became pale at one week
(Figures 1B, 2B). After two weeks, fundus fluorescein angiography (FFA) showed
normal arm-retinal circulation time (A-RCT) and retinal vein filling time
(RVFT) with no visible emboli in the retinal circulation (Figure 3). Only
extracorpored counterpulsation treatment was continued for another month.
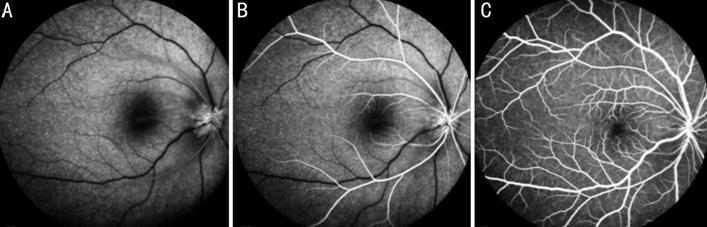
Figure 3 FFA
showed normal A-RCT and RVFT at 15s (A), 17s (B) and 41s (C) two weeks after
surgery.
One month
later, there was no improvement in vision acuity, which remaining hand motion.
Ocular fundoscopy examination showed a pale optic disk with attenuated retinal
vessels (Figure
Carotid
artery disease is the most common etiological factor of retinal arterial
occlusion (RAO), resulting in RAO by embolism, which can hemodynamically induce
retinal ischemia. On the other hand, serotonin (5-hydroxytryptamine) secreted
by rough vascular endothelium can induce arterial spasm[1].
The patient in this case was a 17-years-old young boy with no pre-existing
general illness except congenital cataract and juvenile glaucoma that was
diagnosed during outpatient follow-up. Our literature review did not show any
association between congenital cataract and definite vascular abnormalities or
increased risk of thrombosis. On the other hand, the glaucoma valve implantation
surgery itself was uneventful. Although there is a very small probability that
the valve may cause vascular compression, this impact would be negligible.
Therefore we consider, in this case, that this complication is possibly
attributable to retrobulbar anesthesia rather than surgical procedures or
potential general artery disease.
There are
many case reports describing CRAO after several types of ocular surgeries, such
as cataract surgery[2-3], anti-glaucoma
surgery[4], vitrectomy[5]
or even pterygium excision[6] which were performed
under sub-Tenon’s, peribulbar or retrobulbar anesthesia. To our knowledge, this
is the first report of CRAO after uneventful glaucoma valve implantation
surgery.
Retrobulbar
anesthesia has been widely used in ocular surgeries, and complications of this
procedure (e.g. retrobulbar hemorrhage, injection of lidocaine and air
into the optic nerve sheath, trauma to and partial injection of lidocaine in
the central retinal artery) have been described by Morgan et al[7]. These complications could result in emboli in both
choroidal and retinal circulations, occlusion of the central retinal artery and
vein, or outer retinal ischemic infarction[7-8]. This implies that when anesthesia is administered,
there are ocular blood flow changes[8], which have
been shown by color Doppler imaging (CDI)[9]. We
suggest that pulsatile ocular blood flow (POBF) falls during anesthesia may be
the possible mechanism for CRAO in our case. A reduced ocular blood flow may be
hazardous to patients regardless of whether IOP is raised or not[10-11]. This effect recovers slowly
and is still present after surgery[8,12].
Several
hypotheses have been proposed herein to explain the possible mechanism of a
dramatic reduction of the blood flow velocity after retrobulbar anesthesia.
First, there may be a central retinal artery vasospasm in response to the
injection[13] or the anesthetic agent itself
could possibly diffuse into the artery[2]. This
disturbs the autoregulation of the retinal circulation. Meyer et al[14] found that porcine ciliary arteries were prevented
from relaxation by agents like lidocaine. Riva et al[15]
showed that local anesthetic agents (lignocaine, bupivacaine, and ropivicaine)
could cause relative vasoconstriction at lower concentrations and vasodilation
at higher concentrations. Findl et al[16]
also demonstrated in human that choroidal and central retinal artery blood flow
decreased 15% one minute after peribulbar anesthesia, which is supposed to be
safer than retrobulbar anesthesia. This effect persisted at five to ten minutes[10,16]. This may be an explanation for
the decrease of POBF but it is difficult to determine its clinical relevance as
it is impossible to measure concentration of local anesthetic agent around the
artery.
Secondly,
the mechanical compression of the retrobulbar tissue space by local anesthetic
agent (2.5 mL in our case) may cause a volume effect to the globe. The central retinal
artery is most likely to be compressed within the orbit, especially sincethe
anesthetic agent form a “trapped bolus” before graduallydiffusing throughout
the peribulbar space[2,8]. This
volume effect may initiate a sudden blockage of the central retinal artery.
Huber and Remky[9] reported that a reduction could
be detected in retrobulbar velocity after a 2 mL injection, while systolic
retinal and ciliary perfusion pressure were reduced after an injection of 5 mL
rather than 2 mL.
Thirdly, a
rise in IOP secondary to globe compression might also cause CRAO. It is well
known that an extreme and prolonged increase in IOP is required to produce CRAO[13]. However, several studies showing similar results
indicated that there were not a statistically significant change in IOP
following retrobulbar anesthesia[10-11,17], and others[8,18]
demonstrated a rise in IOP by 3
In
conclusion, CRAO is a rare complication after retrobulbar anesthesia in several
kinds of ocular surgeries, and it is always associated with poor visual
outcome. The mechanism of this unusual complication is still uncertain, but
alternative and possibly safer methods such as topical anesthesia may be
preferred, especially in patients who may have preexisting vascular compromise
or high preoperative IOP level.
ACKNOWLEDGEMENTS
Conflicts of
Interest: Lin FY, None; Fu MS, None.
REFERENCES