
Citation: Li L, Li SF, Liu JH, Deng GD, Ma Y, Ma J, Lu H. Novel transscleral
sutureless subretinal fluid drainage using a 25-gauge trocar-cannula with a
self-closing valve in patients with advanced Coats disease. Int J Ophthalmol 2019;12(9):1444-1449
DOI:10.18240/ijo.2019.09.12
·Clinical
Research·
Novel transscleral sutureless subretinal fluid drainage using a 25-gauge trocar-cannula with a self-closing valve in patients with advanced Coats disease
Liang Li, Song-Feng Li, Jing-Hua Liu, Guang-Da Deng, Yan Ma, Jing Ma, Hai Lu
Beijing Ophthalmology and Visual Science Key Laboratory, Beijing Tongren Eye Center, Beijing Tongren Hospital, Capital Medical University, Beijing 100730, China
Correspondence to: Hai Lu and Song-Feng Li. Beijing Ophthalmology and Visual Science Key Laboratory, Beijing Tongren Eye Center, Beijing Tongren Hospital, Capital Medical University, No.1 Dongjiao Min Xiang Street, Beijing 100730, China. hailu2017@163.com; lsf_0309@163.com
Received:
Abstract
AIM: To assess surgical outcomes of a novel method of transscleral drainage of subretinal fluid using a 25-gauge trocar-cannula with a self-closing valve (DTV) in patients with severe exudative retinal detachment (ERD) in Coats disease.
METHODS: Retrospective consecutive cases of 20 patients (20 eyes) of severe ERD due to Coats disease (stage 3B) in total 156 Coats patients between June 2015 and April 2019 were included in this study. The participants were aged 1 to 10y with a mean age of 3.50±1.79y. The mean follow-up time were 11.9mo. Subretinal fluid was drained transsclerally using a novel method of DTV. The height of the retinal detachment and the regression of abnormal vessels including telangiectasias and aneurysms were observed. Complications including vitreoretinal fibrosis, tractional retinal detachments (TRD), endophthalmitis, retinal holes, and hemorrhages were evaluated.
RESULTS: Following surgeries, the patients showed the replacement of ERD and regression of telangiectatic retinal vessels observed with binocular indirect ophthalmoscopy. Six patients received retinal cryotherapies and 12 patients received laser photocoagulations following first external subretinal fluid drainage using DTV. All patients underwent intravitreal anti-vascular endothelial growth factor therapies to induce residual subretinal fluid absorption. During follow-ups, 8 patients underwent a second drainage operation, 17 patients received retinal laser photocoagulations and 7 patients received cryotherapies. Vitreoretinal fibrosis was found in 7 patients and 6 patients underwent micro-invasive vitrectomies during the follow-up period. Severe TRD, iatrogenic retinal holes, and hemorrhages were not found.
CONCLUSION: The authors present a new therapeutic approach that successfully drains subretinal fluid in advanced stage 3B Coats disease with severe ERD. This is a simple, safe and less invasive approach when compared with traditional managements. However, it should be strictly selected for patients with high bullous ERD close to the central axis of the eye in order to avoid the complication of retinal holes.
KEYWORDS: Coats disease; subretinal fluid; exudative retinal detachment; transscleral drainage
DOI:10.18240/ijo.2019.09.12
Citation: Li L, Li SF, Liu JH, Deng GD, Ma Y, Ma J, Lu H. Novel transscleral sutureless subretinal fluid drainage using a 25-gauge trocar-cannula with a self-closing valve in patients with advanced Coats disease. Int J Ophthalmol 2019;12(9):1444-1449
INTRODUCTION
In 1908, Coats first described a
case of male monocular retinal hemorrhage in a child with retinal
telangiectasia[1].
Coats disease typically manifests as idiopathic retinal vascular abnormalities,
retinal telangiectasia and retinal, intraretinal and subretinal infiltration,
which can lead to severe exudative retinal detachment (ERD). The previous
studies[2-4] classified Coats
disease into five stages: (stage 1) presence of retinal telangiectasia only;
(stage 2) telangiectasia and exudation (
Treatment is aimed at eliminating telangiectasias and aneurysms, which will inhibit further exudation, induce resorption of already formed exudate, and lead to resolution of serous retinal detachment. Retinal laser photocoagulation or cryotherapy is generally successful in stages 1 and 2 of Coats disease. However, in advanced cases with serous retinal detachment (stage 3B), laser photocoagulation and cryotherapy may not be effective because of the persistence of subretinal fluid. Therefore, subretinal fluid drainage (SRFD) is usually required[5-7]. Traditional SRFD was performed by perforating sclera externally with a micro-blade, and subretinal fluid was then drained through the sclerotomy site. Drainage procedure is one of the most delicate and critical steps due to the risk of intraoperative complications such as vitreoretinal incarceration, retinal perforation, subretinal hemorrhage, eye hypotony and choroidal detachment[8-11].
This report highlights a novel, simple and controllable surgical method using a 25-gauge trocar-cannula with a self-closing valve (DTV) to drain subretinal fluid in severe ERD of stage 3B Coats disease, and evaluate its safety, effectiveness and facilitation.
SUBJECTS AND METHODS
Ethical Approval The study was conducted in accordance with the ethical standards stated in the 1964 Declaration of Helsinki and approved by the Ethics Committee of Beijing Tongren Hospital. Both patients and their parents gave written informed consent after explanation of the nature and possible consequences of the treatment.
This study was a retrospective
consecutive case series review of 20 patients (20 eyes) of severe ERD due to
Coats disease (stage 3B) in total 156 Coats patients. Each case of our study
was reviewed to confirm that it met the definition for Coats disease as an
idiopathic retinal vascular telangiectasia with aneurysmal dilatations
associated with exudation and ERD in the absence of arterial macroaneurysms and
proliferative vitreoretinopathy. Patients were diagnosed between June 2015 and
April 2019 at the Eye Center of Tongren Hospital, Beijing, China. Participants
were aged 1 to 10y with a mean age of 3.50±1.79y. All had monocular diseases,
and were combined with severe ERD close to the central axis of the eye which
can be seen sitting against the lens through the dilated pupil. Thus, the
height of the detachment may be more than
Table 1 Clinical data of patients
Case |
Gender |
Age (y) |
Stage |
Follow-up (mo) |
SRFD using a DTV (times) |
Traditional SRFD (times) |
Intravitreal anti-VEGF therapies (Y/N) |
Retinal cryotherapy (times) |
Retinal laser photocoagulation (times) |
Vitrectomy (Y/N) |
Complications |
1 |
Male |
3 |
3B |
21 |
1 |
1 |
Y |
2 |
1 |
N |
None |
2 |
Female |
4 |
3B |
14 |
1 |
1 |
Y |
4 |
3 |
N |
None |
3 |
Female |
5 |
3B |
21 |
1 |
0 |
Y |
1 |
3 |
N |
None |
4 |
Male |
10 |
3B |
15 |
1 |
0 |
Y |
3 |
1 |
N |
VF |
5 |
Male |
3 |
3B |
8 |
1 |
0 |
Y |
0 |
2 |
N |
None |
6 |
Male |
4 |
3B |
11 |
2 |
1 |
Y |
2 |
2 |
N |
None |
7 |
Male |
3 |
3B |
26 |
1 |
1 |
Y |
2 |
2 |
Y |
VF |
8 |
Male |
3 |
3B |
26 |
1 |
0 |
Y |
1 |
4 |
Y |
VF |
9 |
Male |
3 |
3B |
26 |
2 |
1 |
Y |
2 |
1 |
Y |
VF |
10 |
Male |
3 |
3B |
26 |
1 |
0 |
Y |
1 |
2 |
Y |
VF |
11 |
Male |
2 |
3B |
22 |
1 |
1 |
Y |
2 |
5 |
N |
None |
12 |
Male |
1 |
3B |
6 |
1 |
0 |
Y |
1 |
0 |
Y |
VF |
13 |
Male |
3 |
3B |
16 |
1 |
1 |
Y |
3 |
3 |
N |
None |
14 |
Male |
3 |
3B |
17 |
1 |
0 |
Y |
1 |
3 |
N |
None |
15 |
Male |
3 |
3B |
9 |
1 |
0 |
Y |
1 |
2 |
Y |
VF |
16 |
Male |
3 |
3B |
9 |
2 |
0 |
Y |
0 |
4 |
N |
None |
17 |
Male |
4 |
3B |
8 |
1 |
0 |
Y |
0 |
2 |
N |
None |
18 |
Male |
3 |
3B |
10 |
1 |
0 |
Y |
0 |
3 |
N |
None |
19 |
Male |
5 |
3B |
5 |
1 |
0 |
Y |
0 |
3 |
N |
None |
20 |
Male |
2 |
3B |
1 |
1 |
0 |
Y |
0 |
2 |
N |
None |
SRFD: Subretinal fluid drainage; VF: Vitreoretinal fibrosis.
On evaluation under anesthesia, all
patients had total retinal detachment involving macula, with telangiectatic
retinal vessels and massive subretinal exudation suggestive of stage 3B.
Subretinal fluid was drained transsclerally in one or more quadrants,
preferably in areas corresponding with the highest retinal detachment site
confirmed with binocular indirect ophthalmoscopy. Moreover, it was drained
using a novel method of penetrating sclera externally with a DTV (Alcon, Fort
Worth, TX, USA). The surgical procedure was divided into two parts: (Part 1)
the DTV was inserted under the retina toward the optic disc by transsclerally
sclerotomies. The bayonet was then removed and the DTV was gently pressed,
allowing the subretinal fluid to flow out slowly, which made the intraocular
pressure more controllable; (Part 2) a transparent corneal incision was made by
a 15 degree bayonet and then perfusate was injected into the anterior chamber
through the incision when intraocular pressure decreased. This two-part
procedure was repeated until the subretinal fluid was no longer flowing out.
The intraocular length of trocar-cannula system with bayonet was
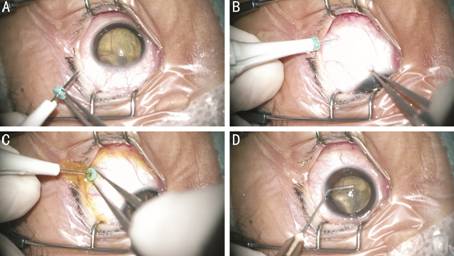
Figure 1 Illustration of the surgical procedure of SRFD A: All cases with Coats disease (stage 3B) were combined with severe ERD close to the central axis of the eye which can be seen sitting against the lens through the dilated pupil; B: The 25-gauge trocar-cannula with the self-closing valve was inserted under the retina toward the optic disc by transscleral sclerotomies; C: The subretinal fluid flowed out slowly while pulling out the bayonetand pressing the self-closing valve gently; D: Perfusate was injected into the anterior chamber through the incision when intraocular pressure decreased.
Patients were followed up at 1d, 1wk, and 1mo after surgery. The follow-up time was determined according to the patients’ retinal condition. The height of retinal detachment and the regression of abnormal retinal vessels were observed. Complications including vitreoretinal fibrosis, tractional retinal detachments (TRD), endophthalmitis, retinal holes, and hemorrhages were evaluated.
RESULTS
No retinoblastoma cells were found on cell smears with histopathological confirmation after first surgery in all patients. All cases were followed up for 1 to 26mo. The mean follow-up time were 11.9mo. Resorption of subretinal fluid and reattachment of ERD, which provided conditions for subsequent retinal laser photocoagulations and cryotherapies, were used as criteria for the evaluation of the efficacy of surgeries. The results of our study are shown in Table 1. After surgeries, patients showed varying degrees of reattachment of ERD assessed with binocular indirect ophthalmoscopy (Figure 2). Six patients received retinal cryotherapies and 12 patients received laser photocoagulations following first SRFD using the DTV. All patients underwent intravitreal anti-VEGF therapies to induce residual subretinal fluid absorption, which allowed the retina to be treated with laser therapies at a later stage. Eight patients underwent a second drainage operation, 17 patients received retinal laser photocoagulations and 7 patients received cryotherapies during follow-ups. At the final follow-up, all eyes showed an anatomical improvement with the replacement of ERD and the regression of telangiectatic retinal vessels. Seven patients developed varying degrees of subretinal fibrosis or fibrotic vitreoretinopathy and 6 patients underwent micro-invasive vitrectomies during the follow-up period. Severe TRD, iatrogenic retinal holes, and hemorrhages were not found.
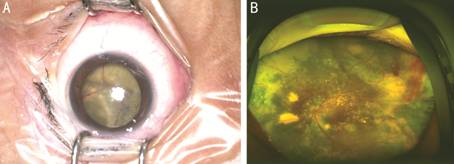
Figure 2 Retinopathies of an 11-year-old male patient with stage 3B Coats disease Preoperative high bullous ERD sitting against the lens through the dilated pupil (A) and postoperative reattachment ERD at the first day after surgery (B).
DISCUSSION
Treatment of stage 3B Coats disease is often difficult due to the presence of ERD. Some studies have shown that SRFD, when combined with other treatments such as intravitreal anti-VEGF therapies and retinal laser photocoagulation, has achieved good results for stage 3B patients[5-6,12-16]. Traditional SRFD was performed by perforating sclera externally with a micro-blade, left an incision that may often be sutured. There may be several intraoperative complications such as vitreoretinal incarceration, retinal perforation, subretinal hemorrhage, ocular hypotension as well as significant postoperative eye discomfort, particularly in children. Recently, some novel minimally invasive methods of SRFD have been reported[17-20]. However, the puncture instrument used in these methods does not have self-closing valve, and surgeons may drain the remaining subretinal fluid by pressing the scleral puncture incision. As a result, the outflow of subretinal fluid was not controllable, which may cause subsequent retinal injuries.
Given these limitations, we investigated a novel SRFD method. A DTV was inserted under the retina by transscleral sclerotomies. This procedure released the subretinal fluid and cholesterol crystals of Coats patients by switching the valves (Figure 1). Subsequent retinal reattachment provided conditions for retinal laser photocoagulations and cryotherapies (Figure 2). This modified therapeutic approach offered several advantages, including: 1) The procedure to insert the 25-gauge trocar-cannula was minimally invasive and did not require suturing; 2) The valve can be left under the retina after the puncture, and allowed simple and accurate control of the drainage rate, thus preventing ocular hypotension; 3) As the intraocular end of the trocar-cannula was blunt and the valve was able to control the drainage rate, it reduced further injury of retina; 4) The diameter of the cannula allowed to discharge some large subretinal cholesterol crystals of Coats patients extrasclerally.
Although we have managed to drain the subretinal fluid during surgery, a small amount of fluid remained in the subretinal space. Intravitreal injection of anti-VEGF agents could induce further reabsorption of subretinal fluid and resolution of exudates, allowing subsequent laser treatments and retinal cryotherapies[21-25]. In our study, 6 patients received retinal cryotherapies and 12 patients received photocoagulations following first SRFD using this modified methods. Retinal cryotherapies and laser photocoagulations were successfully performed in 18 patients during follow-ups. As injection of anti-VEGF agents combined with subretinal drainage and cryotherapy may lead to TRD[26], there were varying degrees of subretinal fibrosis or fibrotic vitreoretinopathy in 7 patients compared with the preoperative period and 6 patients underwent micro-invasive vitrectomies during the follow-up period. However, there were no significant TRD and complications of retinal holes and hemorrhages following the surgical procedure.
However, there are some certain
limitations in our study. Although there may be some risks associated with this
procedure, such as retinal holes and hemorrhages, complications can be avoided
by these ways below. In order to avoid the occurrence of retinal tears, we
recommend choosing patients with high bullous ERD, of which highly detached
retina reached to the posterior surface of the lens. The intraocular length of
trocar-cannula system with bayonet is
In conclusion, the technique used in our study may provide a simple, safe and reliable method of SRFD in patients of severe ERD with advanced stage 3B Coats disease. However, it may not suitable for all patients with stage 3B Coats disease, and should be strictly selected for patients with high bullous retinal detachment close to the central axis of the eye in order to avoid the complication of retinal holes.
This is a small-sample study with a relatively short follow-up time. Furthermore, a larger cohort of patients may be observed for any potential complications.
ACKNOWLEDGEMENTS
We thank David Dimasi, PhD, from LiwenBianji, Edanz Editing China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
Foundation: Supported by Beijing Tongren Hospital, Capital Medical University (No.TRZDYXZY201703).
Conflicts of Interest: Li L, None; Li SF, None; Liu JH, None; Deng GD, None; Ma Y, None; Ma J, None; Lu H, None.
REFERENCES