·Brief
Report·
Treatment
of upper and lower lacrimal punctal occlusion using retrograde canaliculotomy
and punctoplasty
Ai
Zhuang1,2, Jing Sun1,2, Wo-Dong Shi1,2
1Department
of Ophthalmology, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University
School of Medicine,
2Shanghai
Key Laboratory of Orbital Diseases and Ocular Oncology,
Co-first authors: Ai Zhuang and Jing Sun
Correspondence to: Wo-Dong Shi. Department of Ophthalmology, Shanghai Ninth
People’s Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai
Key Laboratory of Orbital Diseases and Ocular Oncology, 639 Zhi Zao Ju Road,
Shanghai 200011, China. siwodo@hotmail.com
Received:
Abstract
This is a retrospective, noncomparative analysis of
a case series to explore the safety and effectiveness of retrograde
canaliculotomy and punctoplasty for treating epiphora due to upper and lower
lacrimal punctal occlusion. During the procedure, the horizontal portion of the
normal lower canaliculus was identified; the corresponding punctum was
reconstructed via retrograde canaliculotomy and punctoplasty. Intubation
was performed to prevent postoperative reocclusion. Patients were followed up
for 12 to 24mo. A total of 16 patients with unilateral upper and lower lacrimal
punctal occlusion were included. Satisfactory outcomes were achieved: all 16
patients exhibited improvement of epiphora; 31 rebuilt punctal openings and
canaliculi achieved recanalization. Only one upper punctal opening could not be
reconstructed because the corresponding canaliculus exhibited severe injury. No
significant complications occurred as a result of the treatments. Retrograde
canaliculotomy and punctoplasty appears to effective, safe, and minimally
invasive for treatment of upper and lower punctal occlusion.
KEYWORDS: punctal occlusion; retrograde canaliculotomy;
punctoplasty; intubation
DOI:10.18240/ijo.2019.09.20
Citation:
Zhuang A, Sun J, Shi WD. Treatment of upper and lower
lacrimal punctal occlusion using retrograde canaliculotomy and punctoplasty. Int
J Ophthalmol 2019;12(9):1498-1502
INTRODUCTION
Lacrimal punctal occlusion can be caused by trauma,
inflammation, congenital anomalies, or surgical intervention[1-3]. Soft tissues or scars close the punctum, obstructing
tear drainage through the canaliculus into the nasal cavity[4].
Thus, patients may experience severe epiphora and report low quality of life.
For patients with punctal stenosis alone or minimal and superficial punctal
scars, direct punctoplasty and silicone tube intubation can be used for
treatment[5-6]. For patients
with complete upper or lower punctal occlusion, some clinicians have reported
the use of a pigtail probe from the normal punctum through the canalicular system
to identify and repair the occluded punctum[7].
For those with simultaneous upper and lower lacrimal punctal occlusion,
lacrimal bypass with a conjunctivodacryocystorhinostomy (CDCR) may be an
option, although it carries the known risks of displacement, recurrent
stenosis, conjunctival granuloma, and backflow from the nasal cavity to the eye[8]. Here, we chose retrograde canaliculotomy and
punctoplasty to treat simultaneous upper and lower lacrimal punctal occlusion.
By incising the canaliculus from the grey line and the conjunctival surface,
then travelling backwards to reconstruct the punctal opening, we achieved
satisfactory outcomes in sixteen patients.
SUBJECTS AND METHODS
Ethical Approval
The study followed the
tenets of the Declaration of Helsinki and was approved by the Ethics Committee
of Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of
Medicine. Written informed consent for participation in the study was obtained
from participants or their guardians. Permission was obtained for the use of
patients’ images.
Overview This is a retrospective, non-comparative analysis of
a case series. We included patients who presented to the hospital between
September 2015 and September 2016 for treatment of upper and lower lacrimal punctal
occlusion. We reviewed patient records, including outpatient and inpatient
medical records, as well as follow-up data and photos recorded by the surgeon
(Shi WD). In the affected eyes, normal punctal structures could not be found
with the naked eye and via slit lamp examination (Figure 1). In
accordance with Kashkouli et al’s[9] visual
grading system, punctal occlusion was scored as Grade 0. All patients presented
with prominent epiphora either indoor or outdoor, and suffered inconvenience
from wiping away tears from time to time. Patients with any of the following
concomitant conditions were excluded: additional lacerations or obstructions
involving the lacrimal sac and/or nasolacrimal duct, craniofacial fractures,
injuries of the optic nerve or the globe, prior surgery involving the lacrimal
system, or a combination thereof. All patients underwent retrograde
canaliculotomy and punctoplasty to reconstruct the punctal opening and
canaliculus. We recorded patient age, sex, etiology (congenital/acquired),
affected side, duration of time from onset to surgery, and concomitant
conditions. Epiphora (frequency and indoor/outdoor characteristics), tear
drainage function, punctal opening shape, and complications were assessed in
the retrospective analysis.

Figure 1 Upper and lower punctal occlusion in a
single patient A: The original upper punctal opening was
undetectable (white arrow); B: The lower punctal opening was replaced by white
scar tissues (black arrow).
Surgical Procedure The patients underwent general or local anesthesia. Each
patient was placed in the supine position. The surgery was performed under the
OPMI Visu 150 surgical microscope (ZEISS,
If the identified canaliculus was unobstructed,
lacrimal irrigation was performed to ensure that the distal lacrimal system was
patent. A Vannas scissor was used to incise the canaliculus, and a Bowman probe
was inserted backward into the proximal canaliculus, such that the tip of the
probe tented the occluded punctal area. Then a punctal opening was made,
approximately
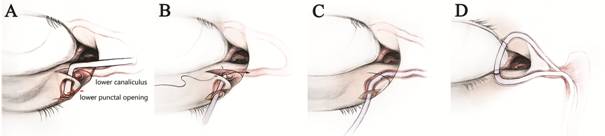
Figure 2 Graphic drawings of the surgical
procedure A: After exposing the horizontal canaliculus, a
Bowman probe was inserted backward to tent the occluded punctal area, and then
a punctal opening was made; B: A silicone stent was intubated through the new
opening and lacrimal canaliculus, eventually reaching the nasal cavity; C: The
incision was closed with 8-0 absorbable sutures; D: Bicanalicular nasolacrimal
duct intubation with the silicone stent was done.
If the identified canaliculus was occluded, an
incision was made in a more medial location, in order to identify the
canaliculus lumen. If a single canaliculus was completely occluded, the
corresponding upper or lower punctum and canaliculus was reconstructed. Thus,
only one head of the silicone tube was extracted from the nasal cavity;
together with the other head from the reconstructed punctal opening, it was
used to form square knots and was then fixed in the nasal cavity. The incisions
were repaired with 8-0 absorbable sutures. If both upper and lower canaliculi
were completely occluded, lacrimal bypass with a CDCR was performed instead.
Furthermore, concomitant conditions were also
treated. For symblepharon, the adhesion was dissected and covered with amniotic
membrane. For bilateral lower eyelid entropion and trichiasis, the modified
Hotz procedure was performed[10-11].
For the lower eyelid ectropion, the rotation flap was used for correction.
Because the upper eyelid coloboma exhibited a small size, the eyelid was
reconstructed by suturing the defected tarsal plate, trimming the skin, and
suturing the eyelid margin.
Postoperative Follow-up Visits Follow-up visits were scheduled 1wk, 1, 3, 6, and 12mo
after surgery. At each visit, the shape of the newly formed punctal opening was
examined via slit lamp; the symptomatic epiphora and lacrimal irrigation outcomes
were recorded. Additionally, the silicone tube was examined at both the puncta
and the nasal cavity during the first 3mo. The silicone tube remained in the
canaliculi for at least 3mo before ultimate removal.
RESULTS AND DISCUSSION
A total of 16 patients (16 upper punctum and 16 lower
punctum) with unilateral upper and lower lacrimal punctal occlusion were
included in the study. Among these 16 patients, there were eight males and
eight females with a mean age of 27.3y (range, 5-74y). Causes included
congenital anomaly (n=7, 43.75%) and heat burn (n=9, 56.25%). The
median time interval from onset to surgery was 5y (range, 4mo to 23y). All
patients exhibited prominent epiphora of the sick eye, especially outdoors in
cold weather. The normal punctal structures of the affected eye could not be
found with the naked eye or via slit lamp examination. Prior to
undergoing the present surgical procedure, 13 patients had received topical eye
drops (e.g. levofloxacin, tobramycin, or sodium hyaluronate) to relieve
the symptoms; three patients had not previously received any related treatment.
Concomitant conditions included symblepharon (n=3), lower eyelid
ectropion (n=2), upper eyelid coloboma (n=1), and bilateral lower
eyelid entropion and trichiasis (n=2).
All patients underwent retrograde canaliculotomy and
punctoplasty to reconstruct the puncta and canaliculi. In 15 of 16 patients
(93.75%), successful reconstruction of both upper and lower punctal openings
was achieved (Figure 3). In one patient, the upper canaliculus was severely
injured and could not be found, despite extension of the first incision and
creation of an additional incision toward the common lacrimal canaliculus.
Fortunately, the lower canaliculus was found; lower punctum and canaliculus
reconstruction and intubation were then successfully performed.

Figure 3 Retrograde canaliculotomy and
punctoplasty A: The lower punctal opening (white triangle) was
reconstructed, and a silicone stent was inserted from the reconstructed
punctum, through the canaliculus (white arrow) and nasolacrimal duct,
eventually reaching the nasal cavity; B: The horizontal part of the upper
canaliculus (black arrow) was identified; C: A silicone stent was intubated
from both the reconstructed upper and lower punctal openings to prevent
postoperative reocclusion.
The median follow-up period was 15mo (range,
12-24mo). At 1 and 3mo, all puncta remained smooth and well-formed; all 16
patients exhibited good tear drainage function with patent lacrimal passages by
lacrimal irrigation. However, 5 patients complained of occasional epiphora
(less than 5 times per day). At 6mo, all 16 patients exhibited symptomatic
improvement of epiphora; 4 patients reported complete elimination of epiphora
both indoors and outdoors, while 12 patients reported continuing epiphora
outdoors in cold weather. At the final follow-up visit, there were fewer
changes in the lacrimal passage conditions than at 6mo after surgery. No
recurrent adhesion or occlusion was found, and recanalization was verified by irrigation
from 31 rebuilt punctal openings (Table 1). In addition, the concomitant
conditions of symblepharon (No.2, No.3, and No.6), ectropion (No.2 and No.9),
eyelid coloboma (No.4), and entropion and trichiasis (No.10 and No.12) were
successfully repaired or corrected.
Table 1 Follow-up outcomes
|
No. |
Epiphora |
State of affected punctum |
Lacrimal irrigation |
|||
|
Preop. |
Final follow-up |
Preop. |
Final follow-up |
Preop. |
Final follow-up |
|
|
1 |
Y |
Improved |
Occluded |
Well-formed |
- |
Patent |
|
2 |
Y |
Improved |
Occluded |
Well-formed |
- |
Patent |
|
3 |
Y |
Improved |
Occluded |
Well-formed |
- |
Patent |
|
4 |
Y |
Improved |
Occluded |
Well-formed (LLP) |
- |
Patent (LLC) |
|
5 |
Y |
Eliminated |
Occluded |
Well-formed |
- |
Patent |
|
6 |
Y |
Improved |
Occluded |
Well-formed |
- |
Patent |
|
7 |
Y |
Improved |
Occluded |
Well-formed |
- |
Patent |
|
8 |
Y |
Eliminated |
Occluded |
Well-formed |
- |
Patent |
|
9 |
Y |
Improved |
Occluded |
Well-formed |
- |
Patent |
|
10 |
Y |
Improved |
Occluded |
Well-formed |
- |
Patent |
|
11 |
Y |
Improved |
Occluded |
Well-formed |
- |
Patent |
|
12 |
Y |
Eliminated |
Occluded |
Well-formed |
- |
Patent |
|
13 |
Y |
Improved |
Occluded |
Well-formed |
- |
Patent |
|
14 |
Y |
Improved |
Occluded |
Well-formed |
- |
Patent |
|
15 |
Y |
Eliminated |
Occluded |
Well-formed |
- |
Patent |
|
16 |
Y |
Improved |
Occluded |
Well-formed |
- |
Patent |
Preop.: Preoperative; Y: Yes; LLP: Lower lacrimal
punctum; LLC: Lower lacrimal canaliculus. The symbol of “-” means “unable for
lacrimal irrigation”.
The lacrimal punctum is the beginning point of the
lacrimal system. The definition of punctal occlusion is not universally agreed
upon. In our study, we made a diagnosis of punctal occlusion when a punctal
opening could not be found with the naked eye and the slit lamp[12]. Punctal occlusion can lead to severe
epiphora and require surgical correction, especially when ipsilateral upper and
lower puncta are both involved[13]. In
contrast to external punctal stenosis, no open punctum is available in punctal
occlusion. Therefore, the following methods are not suitable in this situation:
direct punctal dilation and canaliculotomy; 1-snip, 2-snip, or 3-snip
punctoplasty; punctoplasty with laser or electrocauterization; and punch ampullectomy[6,13-17]. Some
clinicians have reported the of a pigtail probe to treat the punctal occlusion,
by passing the probe through lacrimal canaliculi and tenting the accurate
position of the occluded punctum with the probe tip. However, this method is
difficult to apply to patients with congenital anomalies, such as canalicular
agenesis or simultaneous upper and lower punctal occlusion[7].
Retrograde intubation of the canaliculi during dacryocystorhinostomy is a new
solution; however, this procedure increases scarring of the inner canthus skin[18]. CDCR with insertion of a Jones tube is not a
suitable first choice because of the potential difficulty in maintaining the
tube’s position and patency, and the tear flow outflow rate[19-20].
In this study, we performed retrograde canaliculotomy
at the horizontal part of the canaliculus. The critical stage of the procedure
is exploration of the horizontal part of the canaliculus, in order to locate
the punctal area. Within the first
Rather than using a tear drainage tube implant, such
as the Jones tube, our method uses the original lacrimal passage; thus, it
follows the original anatomy and avoids the risks of rejection. Additionally,
the middle canalicular incision was meticulously closed with microsurgical
techniques, thereby reducing the incidence of incision obstruction[21]. In our study, 31 of 32 (96.9%) occluded puncta and
canaliculi were successfully reconstructed with this method. In a single
patient, the upper canaliculus could not be found, despite two incisions at the
horizontal part, each 5-mm deep. This failure occurred because the proximal
upper canaliculus was severely injured with extensive scarring, such that
normal canalicular mucosal tissues could not be found. Fortunately, we were
able to find the lower canaliculus; thus, we successfully performed lower punctum
and canaliculus reconstruction and intubation. Considering that the lower
canaliculus demonstrates approximately 75% of the tear drainage function, we
discontinued further intervention of the upper punctum and canaliculus after
discussion with the patient[24]. Five patients
complained of occasional epiphora at 1 and 3-month follow-up visits; however,
all patients achieved improvement of symptomatic epiphora after removal of the
silicone tube. Therefore, the symptoms might have been caused by temporary iatrogenic
lacrimal stenosis of the intubation. At the final follow-up visit, despite
sufficient reconstruction of the punctal opening and canaliculus, 12 patients
continued to exhibit epiphora outdoors in cold weather. This outcome suggests
that our method failed to reconstruct the punctal sphincter, such that punctal
function could not be fully restored. Therefore, patients remain at risk of
insufficient tear drainage under some conditions. Notably, occasional epiphora
was reported by the patient in whom the upper canaliculus could not be found.
Nonetheless, the patient considered the outcome to be acceptable, and there was
no requirement for further intervention.
A limitation of this method is that it is only
suitable for patients with relatively normal common canaliculus, lacrimal sac,
and nasolacrimal duct. However, for patients with both upper and lower punctal
occlusion, it is difficult for clinicians to perform preoperative evaluation of
the distal part of the lacrimal duct. When attempting the procedure, an
alternative method, such as CDCR, should be available in case the distal
lacrimal duct is occluded. We note that the small sample size is also a
limitation of this study. In conclusion, retrograde canaliculotomy and
punctoplasty is a relatively simple method that uses the original lacrimal
system and can adjust the tear outflow rate. It appears to be a safe and
effective method for treating upper and lower lacrimal punctal occlusion.
ACKNOWLEDGEMENTS
We thank Ryan Chastain-Gross, Ph.D., from Liwen Bianji,
Edanz Group
Authors’ contributions: Zhuang A analyzed and interpreted the patient data. Sun J
reviewed and revised the manuscript. Shi WD performed the surgeries, and was a
major contributor in writing the manuscript. All the authors read and approved
the final manuscript.
Foundations: Supported by the National Natural Science Foundation of
Conflicts of Interest: Zhuang A, None; Sun J, None; Shi WD, None.
REFERENCES