
Citation: Park J, Jeon H, Choi H. Pilomatrixoma of the upper eyelid
in a 10-month-old baby. Int J Ophthalmol
2019;12(9):1510-1513
DOI:10.18240/ijo.2019.09.23
·Letter to the Editor·
Pilomatrixoma
of the upper eyelid in a 10-month-old baby
Jungyul Park1, Hyeshin Jeon1,2,
Hee-Young Choi1,2
1Department of Ophthalmology, Pusan
National University Hospital, Busan 49241, Korea
2Biomedical Research Institute, Pusan
National University Hospital, Busan 49241, Korea
Correspondence to: Hee-Young Choi. Department of
Ophthalmology, School of Medicine, Pusan National University, 1-10, Ami-dong,
Seo-gu, Busan 602-739, Korea. hychoi@pusan.ac.kr
Received:
DOI:10.18240/ijo.2019.09.23
Citation: Park
J, Jeon H, Choi H. Pilomatrixoma of the upper eyelid in a 10-month-old baby.
Int J Ophthalmol 2019;12(9):1510-1513
Dear Editor,
I am Dr. Jungyul Park from the
Division of Oculoplasty, Department of Ophthalmology, Pusan National University
Hospital, Busan, Korea. I am writing to present a case of pilomatrixoma of the
upper eyelid in a 10-month-old baby that first appeared when the baby was 3
months old. To our knowledge this is the youngest reported case of this tumor
type. The authors obtained informed consent in person and adhered to the tenets
of the Declaration of Helsinki.
Pilomatrixoma (“benign calcifying
epithelioma of Malherbe”; pilomatricoma) is a rare benign adnexal tumor arising
from the matrix cells at the base of a hair[1]. It
was first described by Malherbe[2] in 1880 as a
“calcifying epithelioma” and was thought to be derived from the sebaceous
gland. The exact pathogenesis is still unknown but has been linked to molecular
genetic mutations in the Wnt signaling pathway in basophilic and shadow cells[3]. Downregulation of the adenomatous polyposis coli (APC)
gene in Gardner syndrome contributes to the Wnt signaling, with overexpression
of beta-catenin[4-5] described
in some literature. Additional gene interactions associated with Turner
syndrome and myotonic dystrophy have also been reported[6-7].
In the discipline of ophthalmology,
Ashton[8] reported 3 cases of epithelioma of
Malherbe on the eyelids of female patients, and Forbis and Helwig[9] later suggested the currently accepted name
“pilomatrixoma”. This tumor type typically presents a solitary, superficial,
slow-growing, irregularly shaped, nodular and non-tender mass which is easily
movable over the subcutaneous tissue[10]. It is
usually located near the lateral aspect of the eyebrow or upper eyelid, and is
frequently first diagnosed as a dermoid cyst. Pilomatrixoma occasionally
exhibits rapid growth and may resemble a keratoacanthoma, and can rarely
undergo malignant transformation into a pilomatrix carcinoma[11-13]. It is more common in the first 2 decades of life,
and has tendency to affect young females[14-16]. Among case reports and case series’ of periocular
pilomatrixoma worldwide, the youngest patient of whom we are aware was a
1-year-old female[17]. In this case report, we
report an upper eyelid pilomatrixoma in a 10-month-old female, with the first
symptoms and mass presenting at 3 months of age. To our knowledge, this is the
youngest such case reported.
The 10-month-old female baby
presented at the hospital with a slowly growing mass in the subciliary area of
the right upper eyelid that had first appeared at 3mo. It was first localized
in the right upper eyelid as a small, nodular and bluish colored lesion (Figure
1). Her parents described the mass as a bruise, but she had no history of
trauma. The bluish mass later gradually enlarged and changed color to mixed red
and blue. On palpation, it was fairly well circumscribed, movable, firm and
round in shape rather than ulcerated. Physical examination and interviews with
the parents indicated no birth or infection history, family history or other
history which might be associated with a tumor or mass lesion. On examination,
the patient’s light-reflex, relative afferent pupillary defect, and ocular
motility examinations were all normal. The mass was located on the central to
lateral aspect of the right upper eyelid, involving nearly the entire eyelid
vertically but not the eyelid margin and causing mechanical ptosis. It showed
non-tender characteristics and did not cause pain. The eyelid eversion test
showed a normal palpebral conjunctiva. Magnetic resonance imaging (MRI) with
contrast of the orbit showed a 1.7×1.3×1.1-cm well-circumscribed nodular mass.
It showed high signal intensity on T1-weighted images and minimal enhancement,
and isometric signal intensity with adjacent muscle on T2-weighted MRI. It
contained internal calcification (Figure 2). Differential diagnoses based on
MRI findings were pilomatrixoma and ossifying hematoma. When the patient was
approximately 1 years old, we performed a total excisional biopsy using a
sub-brow line incision approach. There were no specific complications.
Fortunately, the mass was not infiltrative to adjacent tissues and was totally
removed. The gross resected mass was

Figure 1 Preoperative right upper
eyelid photograph It demonstrates mixed red to
blue colors with central yellowish lipid like deposit, 1.7×
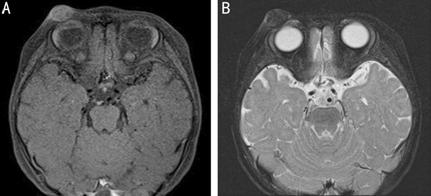
Figure 2 MRI of the orbit A: T-1 weighted image; B: T-2
weighted image. It showed high signal intensity on T1-weighted images and
minimal enhancement, and isometric signal intensity with adjacent muscle on
T2-weighted MRI. It contained internal calcification.
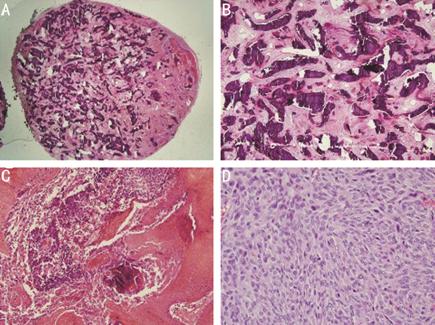
Figure 3 Pilomatrixoma
histopathology A: Well
capsulated circumscribed mass was observed (H&E 1.25×); B: Many
calcifications were observed inside the mass (H&E 4×); C, D: Many
basophilic cells and anucleated “shadow or ghost” cells were composed solid
nest which undergoing trichilemmal-type keratinization (H&E 40×, 400×).

Figure 4 Over the course of a 6-year
follow up picture of patient, no relapse or complication has been observed, and
the scar is almost faded.
Pilomatrixoma is a relatively rare
periocular tumor[16]. Eyelid pilomatrixoma is
usually solitary although it presents as multifocal in 5% of cases.
Approximately 40% of cases occur in the first decade of life and an additional
20% in the second[18-20]. Over
75% of cases were reported to occur in patients 13 years old or younger[20]. A bimodal distribution of occurrence for eyelid
pilomatrixoma has been suggested, with a second peak in the fifth to seventh
decades of life[21]. Actually, in the ophthalmic
literature, only a few case reports or series were reported and according to
the report published until now, the youngest age was 1 year-old female baby[17,20,22]. A racial
study revealed that most cases presented in Caucasians and relatively few in
Asians[23]. We report an onset age of 3mo that is
the youngest published thus far. Ophthalmologists are often unfamiliar with
pilomatrixoma, and if the patient is too young for a delicate examination, such
as in this case, determination of management strategies is difficult. It is
therefore important to know the clinical characteristics of each tumor lesions.
Zloto et al[17] recently suggested that only 16% of pilomatrixoma
cases are correctly diagnosed preoperatively. Other studies also reported low
diagnostic accuracies of 12.5% and 23.07%[20],
attributable to a lack of awareness about this type of tumor. Pilomatrixoma
generally presents as a subcutaneous red to blue mass that is well
circumscribed, mobile, and firm or gritty to palpation[1].
Its appearance and characteristic location on the lateral aspect of the eyebrow
frequently suggests alternative diagnoses such as dermoid cyst, sebaceous cyst,
trichoepithelioma, eyelid cyst, retention cyst, and abscess[24].
Histopathologically, the memorable features of pilomatrixoma are a
proliferation of viable basaloid cells, shadow cells, foci of calcification,
and occasionally ossification. The tumor contains sheets of bland, uniform,
basophilic hair matrix cells that readily undergo necrosis forming eosinophilic
shadow cells with ghostly nuclei[20]. In the case
we report here, initial alternative diagnoses were a dermoid cyst, a tumor
derived from vascular origin, or pilomatrixoma because of the reddish
vascularitic, bluish and central necrotic appearance.
Ultrasound is most commonly reported
modality used to identify the pilomatrixoma, which shows well-defined, ovoid,
hypoechoic heterogenous masses with posterior shadowing and echogenic internal
foci[25]. Hoffmann et al[26] first suggested that MRI may be diagnostic for
pilomatrixoma. Recently, pilomatrixoma has been described as a well-defined
mass with intermediate homogeneous signal intensity on T1-weighted images and
high signal intensity on T2-weighted images[27-30]. In our case study, MRI showed a nodular
well-circumscribed mass with central calcification. The tumor showed high
signal intensity on T1-weighted images, and isometric signal intensity with
adjacent muscle and minimal enhancement on T2-weighted images. The difference
between the T2-weighted images we obtained and those from other studies made
our definite diagnosis as a pilomatrixoma somewhat difficult.
Complete resection with clear
margins is agreed to be the definitive treatment and diagnostic method for
pilomatrixoma[3]. Some studies[31-32] suggest that a fine needle aspiration may be used for
preoperative diagnosis, but this technique is not useful in 0- to 1-year-old
babies. Spontaneous regression of pilomatrixoma has never been reported or
observed. Incomplete resection leads to high recurrence rates[33], so achievement of complete excision is important.
Forbis and Helwig[9] report relapse rates of 2%-6%
but Guinot-Moya et al[34] found a
significantly lower recurrence of 0.48%. We report no relapse, complications or
cosmetic problems over the course of a 6-year follow up.
Currently, pilomatrixomas are
believed to associated with mutation of the Wnt pathway, which is not well
described in the ophthalmologic literature. This tumor type is often initially
misdiagnosed, particularly at the preoperative stage. However, with better
understanding of the tumor and lesion, it is treatable without unnecessary
management or pre- and postoperative complications. Even in patients younger
than 1y, we should be able to diagnose this tumor type and perform complete
surgical removal for diagnostic confirmation and treatment.
We hope that our report of the
successful surgical removal of an upper eyelid pilomatrixoma first presented at
3mo and treated at approximately 1y without relapse or cosmetic complication over
a 6-year follow-up will help ophthalmologists with early diagnoses and surgical
removal of this tumor type even in baby patients.
ACKNOWLEDGEMENTS
Conflicts of Interest: Park J, None; Jeon H,
None; Choi H, None.
REFERENCES