
·Investigation·
Measurement
of the depths at different regions of the anterior chamber in healthy Chinese
adults
Yuan
Zong1,2, Qing-Chen Li1,2, Huan Xu1,2, Jian Yu1,2,
Chun-Hui Jiang1,2,3, Xing-Huai Sun1,2
1Department of Ophthalmology and
Vision Science, Eye and ENT Hospital, Fudan University, Shanghai 200031, China
2Key Laboratory of Myopia of State
Health Ministry, and Key Laboratory of Visual Impairment and Restoration of
Shanghai, Shanghai 200031, China
3Department of Ophthalmology,
Shanghai Fifth People’s Hospital, Shanghai 200240, China
Co-first authors: Yuan Zong and Qing-Chen Li
Correspondence to: Chun-Hui Jiang. Department of
Ophthalmology and Vision Science, Eye and ENT Hospital, Fudan University, 83
Fenyang Rd, Shanghai 200031, China. chhjiang70@163.com
Received:
Abstract
AIM: To measure the depths
of different regions of the anterior chamber (AC) in healthy Chinese adults,
and to explore possible correlations with age or gender.
METHODS: The AC was imaged by
swept-source optical coherence tomography in healthy Chinese adults. The
horizontal scan of the right eye was used to measure the anterior chamber depth
(ACD) at 199 points.
RESULTS: A total of 309 images
from 309 subjects were analyzed. The ACD values at nearly all locations were
negatively correlated with age (all P<0.05), except for ACD1, 2, 198,
and 199 (correspond to the iris roots). The mean annual decrease 0.013±
CONCLUSION: This study showed that
optical coherence tomography can be used to measure the ACD of different
regions of the AC. We found reductions in ACD with age, although the reduction
varied among different points, in healthy Chinese adults.
KEYWORDS: optical coherence
tomography; anterior chamber depth; age; gender; anterior chamber
DOI:10.18240/ijo.2020.01.20
Citation:
Zong Y, Li QC, Xu H, Yu J, Jiang CH, Sun XH. Measurement of the depths at
different regions of the anterior chamber in healthy Chinese adults. Int J
Ophthalmol 2020;13(1):135-140
INTRODUCTION
The anterior
chamber depth (ACD) is of great interest to ophthalmologists, especially
glaucoma specialists, because of its relationship to primary angle-closure
glaucoma (PACG), which is responsible for nearly half of all cases of
glaucoma-related blindness worldwide[1]. Several
factors had been reported to play an important role in the increasing of PACG
incidence with age[2], including increases in lens
vault (LV)[3], lens thickness[4],
and iris curvature (IC)[5]. Monitoring all of
these parameters could be difficult and time consuming. But, because all of
these factors contribute to the pathogenesis of PACG via reductions in
ACD, measuring the depths of different regions of the anterior chamber (AC)
could be another alternative choice. However, in most prior studies, the ACD
was only measured once along the optical axis[6-7], so there is limited information on the ACDs of other
regions of the AC. Cheon et al[8] reported
that with the increasing in age, the angle opening distance at 500 μm from the
scleral spur (AOD500) decreases slower than the central ACD (AOD500:
SUBJECTS AND METHODS
Ethical Approval This study was approved by the
Institutional Review Board of the Eye and ENT Hospital of Fudan University, and
was performed in accordance with the principles of the Declaration of Helsinki.
All of the subjects signed informed consent forms.
Subjects Heathy Chinese adults were enrolled
between May and July, 2015. All of the subjects underwent thorough ocular
examinations, including measurement of best-corrected visual acuity (BCVA);
refraction measured by an auto-refraction system; spherical equivalent (SE),
which was calculated as the spherical diopter (D) plus one-half of the
cylindrical dioptric power; slit-lamp biomicroscopy; and undilated fundus
examination by direct ophthalmoscopy. The axial length (AL) was measured using
an IOL Master 500 (version 3.01; Carl Zeiss Meditec, Jena, Germany).
Intraocular pressure (IOP) was measured using a non-contact tonometer (Topcon
CT
Swept-Source Optical Coherence Tomography
Imaging and Analysis OCT scans
were obtained using a commercially available swept-source OCT (SS-OCT) system
(CASIA SS-1000; Tomey Corporation, Nagoya, Japan; software version 6H.4), under
normal room illumination (340 lx) without pupil dilation. An experienced
observer (Zong Y) performed all image acquisitions. We used the standard
anterior segment scan protocol, which produces a 3-dimensional scan of the
anterior segment with 128 radial slices (each
Measurements of Anterior Chamber
Depths at 199 Locations The horizontal (0°-180°) scans from
the right eyes was selected for further analyses. Rhinoceros-NURBS Modeling for
Windows (version 5.0; McNeel North America, Seattle, WA, USA) with the
Grasshopper plug-in (McNeel North America) were used to measure the ACDs at 199
points (ACD1-199) with the following procedure. First, the boundary of the AC
was drawn and the scale line from the OCT image was copied (Figure
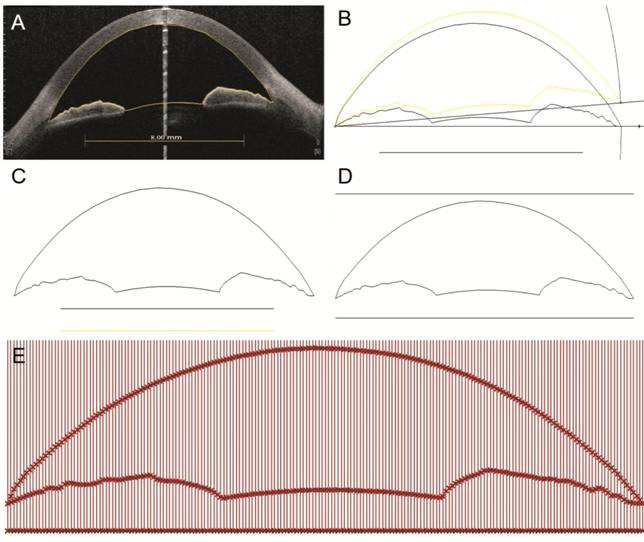
Figure 1 Measurement of ACD at 199
points A: The boundary of the AC was drawn
and the scale line was copied from the OCT image; B: The background bitmap was
removed and the outline of the AC was rotated to orientate both angle recesses
along one horizontal line; C: The image was recalibrated; D: Two horizontal
lines parallel to the line connecting the angle recesses were drawn above and
below the outline of the AC; E: The AC was divided by placing 200 lines using a
path created using the Grasshopper plug-in. ACD1-199 were defined from temporal
(T) side (180°) to nasal (N) side (0°). ACD1 was defined as the length of the
first vertical line from the T side, ACD2 was defined as length of the second
vertical line, and the other ACDs were defined in the same way.
Repeatability and
Reproducibility For the first 20 eyes,
intra-observer repeatability was determined by one observer who manually
measured ACD1-199 twice and inter-observer reproducibility was evaluated by two
observers who each measured ACD1-199 independently.
Statistical Analysis Only the data from the right eyes
was included in the final analysis. All analyses were performed using SPSS
software version 16.0 (SPSS Inc., Chicago, IL, USA). Data are presented as the
mean±standard deviation (SD). Intra-class correlation coefficients (ICC) and
Bland-Altman plots were used to assess the intra-observer repeatability and
inter-observer reproducibility of ACD measurements. The agreement between the
central ACD and ACD100 was assessed using ICCs and Bland-Altman plots. ICCs of
0.81-1.00 indicate almost perfect agreement and values of <0.40 indicate
poor to fair agreement. Linear regression was used to analyze the associations
between age, gender, and ACD1-199, and to determine the annual decrease in ACD.
The annual reduction in ACD was calculated as the annual ACD reduction divided
by the mean ACD. ACD1-199 were equally divided into three symmetrical regions:
ACD1-33 and ACD167-199 (peripheral region); ACD34-66 and ACD134-166 (middle
peripheral region); and ACD67-133 (central region). One-way analysis of
variance (ANOVA) and Bonferroni’s post-hoc test was used to compare the
difference in reduction rates among the three different parts, and between
pairs of region. The level of significance was set at P<0.05.
RESULTS
A total of 309 right eyes from 309
healthy Chinese adults (185 females and 124 males) with a mean±SD age of
36.48±9.51y (range: 18-65y) were analyzed in this study. Their mean IOP was
13.5±
The intra-observer and
inter-observer ICCs were >0.90 for all ACDs except for ACD1, 2, 198, and 199
(correspond to the iris roots) for which the ICCs were >0.8. Bland-Altman
analysis also showed good intra-observer and inter-observer conformity. The
mean central ACD was 2.89±
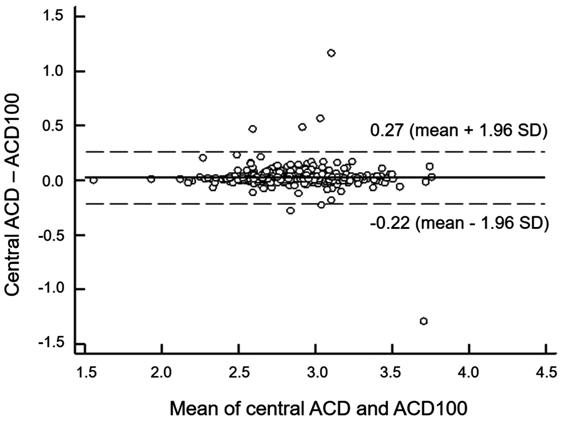
Figure 2 Bland-Altman plot for
assessing the agreement between the central ACD and the ACD at point 100.
Linear regression analysis showed
that all ACDs were negatively correlated with age (all P<0.05) except
for ACD1, 2, 198, and 199 (P>0.05), which correspond to the iris
roots. The mean annual decrease 0.013±
Table 1 Annual reductions in
anterior chamber depths according to age
|
ACD region |
Mean±SD (mm/y) |
Range (mm/y) |
Pa |
Pb |
|
A |
0.008±0.004 |
0.00002-0.014 |
<0.001 vs. B and C |
<0.001 |
|
B |
0.017±0.003 |
0.011-0.022 |
<0.001 vs. A and C |
|
|
C |
0.014±0.001 |
0.013-0.017 |
<0.001 vs. B and C |
ACD: Anterior chamber depth; SD:
Standard deviation; Region A: Peripheral region (ACD1-33 and ACD167-199); B:
Middle region (ACD34-66 and ACD134-166); C: Central region (ACD67-133). aOne-way
analysis of variance followed by Bonferroni post-hoc tests; bP
values from one-way analysis of variance for regions A, B, and C.
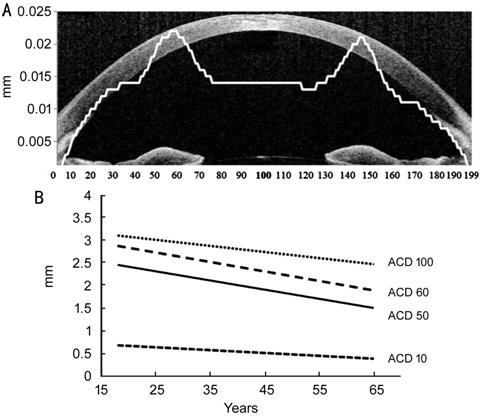
Figure 3 Mean annual reductions (A)
of ACD at points 1-199 and representative reduction sites of ACD (B).
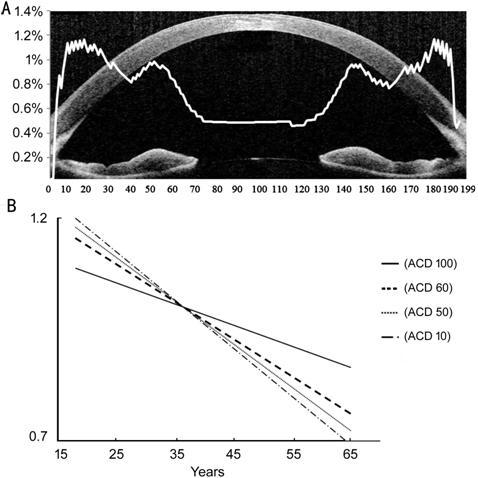
Figure 4 Mean annual reduction rates
(A) of ACD at points 1-199 and representative reduction rates sites of ACD (B).
In additional analyses, we found
that the majority (145/199) of ACDs were associated with gender (all P<0.05).
The ACDs were significantly lower in females than in males, except for ACD1-3,
ACD47-70, ACD131-153, and ACD196-199 (all P>0.05). These ACDs
correspond to the angle recess and iris collarettes regions. The mean
difference in ACD1-199 between males and females was 0.081±
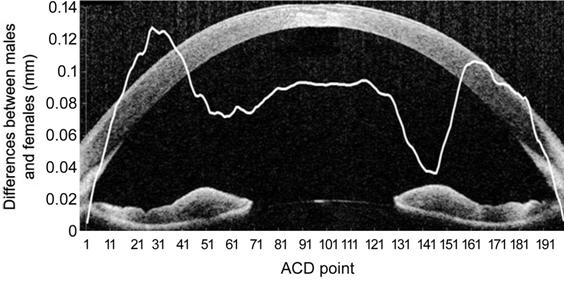
Figure 5 Differences in ACD at points
1-199 between males and females.
DISCUSSION
In this
study, we measured the depths of different regions of the AC, and determined
their possible correlations with age and gender. We found that most of the ACDs
were negatively correlated with age, but the annual reductions varied among
different regions of the eye. The ACDs around the pupil margin showed the
greatest annual reduction. The ACDs were significantly greater in males than in
females for 145/199 points, especially in the middle region of the iris. To our
knowledge, this is the first time to quantitative analysis of the AC at
different regions, it could give insights to understand potentially mechanism
of PACG, and guide us toward more effective diagnoses and treatments.
In prior
studies, ACD was measured by A-scan ultrasonography[10],
optical biometry (IOL Master), Scheimpflug camera (Pentacam)[11],
ultrasound biomicroscopy, and OCT[12]. However,
most of these studies focused on the central ACD. Notably, Ko et al[13] reported a poor correlation between the Van Herick
grade and the central ACD. Kashiwagi et al[14]
reported that, in some patients with closed angle glaucoma, the peripheral ACD
was correlated with elevated IOP, but central ACD was not. So evaluation of
only the central ACD was not enough. On the other hand, study found that most
of the PACG eyes had more than one mechanism underlying angle closure[15], and it was crucial to reveal all the mechanisms for
a better control of the IOP. And different mechanisms were related to the
reduction of the ACD at different part of the AC for example pupillary block (PB)
usually presents as a reduced depth of the central AC, while plateau iris (PI)
configuration and thick peripheral iris roll are usually characterized by a
relative deep central AC but a shallow peripheral AC[16-17]. Measuring the depths of different regions of the AC
was first proposed by Tornquist[18] and the
approach was modified by Hitchings et al[19].
But they determined the ratio between the peripheral and the axial chamber.
Kashiwagi et al[20] developed another
method that involved taking consecutive images under slit-lamp illumination but
the intra-observer repeatability and inter-observer reproducibility
deteriorated with increasing distance from the optical axis.
Here, we
used a novel method to measure the ACD at 199 points. The intra-observer
repeatability and inter-observer reproducibility of the method were good. The
Bland-Altman plots showed good conformity and spatial accordance between the
conventional central ACD and ACD100. Thus, the method used here could applied
in future studies in which the ACDs are measured in different regions.
ACDs
negatively correlated with age and female gender was in accordance with the
findings that advancing age and female gender are two major predisposing
factors for the development of PACG. Reductions in ACD with age have been
reported. In our study, the annual reduction of ACD100 was
Moreover,
while most of the ACDs were negatively correlated with age, the annual
reduction was higher around the iris collarettes at the pupil margin (Figure
3). On the other hand, although the annual reduction in the ACD was lower in
the periphery than in the central area, the annual reduction percentage was on
the contrary higher in the periphery than the center (Figure 4). And the
progression over the years would actually lead to the angular closure found in
elder subjects. The major mechanisms of PACG are categorized into four types
based on anterior segment OCT findings: PB, PI configuration, thick peripheral
iris roll, and exaggerated LV[28]. PB usually
presents as a reduced depth of the whole AC, while PI configuration and thick
peripheral iris roll are usually characterized by a relative deep central AC
but a shallow peripheral AC. The greatest reductions in ACD with age were found
at the AC angle and the pupil margin, was is consistent with the increasing
incidence of PACG with age.
We also found that the ACDs of
nearly all regions were less in females than in males, similar to the findings
reported by Fernandez-Vigo et al[29]. This
also agrees with our clinical experience that the prevalence of PACG is higher
in females than in males. The differences in ACDs between males and females
were most pronounced at ACD21-41 and ACD160-166 (all >
Some
limitations of our study include its cross-sectional design, the analysis of
horizontal scans only and as only subjects from 18 to 65 years old were
included in the study, the annual reduction of ACD at subjects over 65y was not
known. In following study, PACG patients with PI configuration or PB will
included, and ACD at different regions will be compared to find a valuable way
in differentiating PB and PI configuration.
In
conclusion, we successfully used SS-OCT to reliably and reproducibly measure
the depths of different regions of the AC. We found reductions in ACDs with
age, although the reductions were not uniform throughout the AC, and the
greatest reductions in ACD occurred in the region around the iris collarettes.
ACKNOWLEDGEMENTS
The authors thank the subjects and
our colleagues who helped perform this study.
Foundations: Supported by research grants from
the National Key R&D Program of China (No.2017YFC0108200); the Shanghai
Committee of Science and Technology (No.16140901000; No.13430710500;
No.15DZ1942204).
Conflicts of Interest: Zong Y, None; Li QC,
None; Xu H, None; Yu J, None; Jiang CH, None; Sun XH,
None.
REFERENCES