IF in JCR CiteScore
Rank About IJO Current
Issue Featured Articles Articles In Press Recent Accepted
 International Journal
of Ophthalmology
International Journal
of Ophthalmology
2017; 10(9): 1379-1384
·Clinical Research·
Long-term efficacy and safety of ExPress
implantation for treatment of open angle glaucoma
Geun Young Lee1, Chong Eun Lee2,
Kyoo Won Lee1, Sam Seo1
1Department of
Ophthalmology, Cheil Eye Hospital, 1 Ayang-ro, Dong-gu, Daegu 41196, Korea
2Department
of Ophthalmology, Keimyung University, Dongsan Medical Center, Dongsan-dong,
Jung-gu, Daegu 41931, Korea
Correspondence to: Sam Seo.
Department of Ophthalmology, Cheil Eye Hospital, 1 Ayang-ro, Dong-gu, Daegu
41196, Korea. vit.s0324@gmail.com
Received: 2017-01-13
Accepted: 2017-04-21
Abstract
AIM: To
compare the long-term efficacy and safety of ExPress implantation and standard
trabeculectomy in patients with primary open angle glaucoma (POAG).
METHODS:
In this retrospective study, we compared 17 eyes treated by ExPress
implantation with 23 eyes treated by trabeculectomy. Efficacy was assessed
according to the relevant intraocular pressure (IOP) values and success rates
during the first year of follow-up. Postoperative corneal endothelial cell loss
was also compared.
RESULTS: The
number of antiglaucoma medications and the IOP reduction were similar between
the 2 groups during the follow-up period. Although the mean IOP was similar,
the IOP-fluctuation rate during the early postoperative period was
significantly lower in the ExPress group than in the trabeculectomy group (P=0.038).
A Kaplan-Meier survival curve analysis showed no significant success-rate
difference between the groups (P=0.810). The corneal endothelial cell
loss rate, moreover, was significantly lower in the ExPress group (P=0.05).
CONCLUSION: ExPress
implantation compared with trabeculectomy showed similar IOP-reduction and
success rates along with lower IOP fluctuation and endothelial cell loss rates.
For this reason, it can be considered to be the treatment of choice for
patients with advanced glaucoma or low corneal endothelial cell density.
KEYWORDS: primary
open angle glaucoma; ExPress implant; trabeculectomy
Citation: Lee GY, Lee CE, Lee KW, Seo S. Long-term efficacy and safety of ExPress
implantation for treatment of open angle glaucoma. Int J Ophthalmol 2017;10(9):1379-1384
INTRODUCTION
Trabeculectomy is the most commonly performed
operation for intraocular pressure (IOP) reduction in glaucoma patients since
1968[1]. Potentially devastating complications
including early hypotony, choroidal detachment and bleb-related problems,
however, have prompted calls for a safer, better surgical option[2]. In recent years, several alternative
procedures have been evaluated relative to trabeculectomy[3-4]. ExPress glaucoma filtration device (Alcon,
Fort Worth, Texas, USA) implantation, for example, shows similar IOP-reduction
efficacy with fewer complications[5-6].
The ExPress implant is a non-valved stainless steel tube that is inserted
under a partial-thickness scleral flap to connect the anterior chamber to the
subconjunctival space. The theoretical advantages of this device include
increased reproducibility, simplicity, and reduced possibility of ocular tissue
trauma.
Although glaucoma surgery has made
significant progress in terms of safety, complications are still possible. One
reportedly late postoperative complication of both trabeculectomy and
implantation surgery is corneal decompensation[7].
Implantation surgery is considered to be a safer procedure overall,
though it can cause more corneal complications than trabeculectomy[8-9]. Corneal decompensation for
instance, based on a long-term follow-up study of Ahmed valve implantation, has
been reported to occur in up to 30% of patients[10].
There are as yet no long-term follow-up reports on the safety of ExPress
implantation in the corneal endothelium. In the present study, therefore, we
compared the clinical outcomes of ExPress implantation and standard
trabeculectomy in patients with medically uncontrolled glaucoma, in terms of
not only the hypotensive effect, but also any complications related to corneal
endothelial damage.
SUBJECTS AND METHODS
Subjects We retrospectively reviewed the records
of all patients treated consecutively by ExPress implantation or trabeculectomy
between January 2014 and June 2014 at the Cheil Eye Hospital Glaucoma Clinic.
Eyes treated by ExPress implantation were compared with eyes treated by
trabeculectomy during an overlapping period. The main inclusion criterion was
primary open angle glaucoma with unsatisfactory IOP control despite maximally
tolerated topical and systemic medication. Additional inclusion criteria were
noncompliance with antiglaucoma medication regimen, allergy to medication,
significant IOP fluctuation, and/or documented progression of visual field (VF)
defect despite medication-controlled IOP. The exclusion criteria included
previous ocular surgery except cataract surgery, closed or narrow angle, or
ocular disease other than glaucoma. Cheil Eye Hospital Institutional Review
Board approval was obtained prior to the review of the patients’ medical
records.
Preoperative and Postoperative
Examinations All of the
patients underwent a complete ophthalmic examination preoperatively, which
included best-corrected visual acuity measurement, slit-lamp biomicroscopy, IOP
using Goldmann applanation tonometry (Haag-Streit, Koeniz, Switzerland),
gonioscopy, and optical coherence tomography (Cirrus HD-OCT; Carl Zeiss,
Dublin, California, USA) of the optic disc and retinal nerve fiber layer.
Additionally, standard automated perimetry using Swedish interactive threshold
algorithm 30-2 (Humphrey Field Analyzer II; Carl Zeiss Meditec, Inc., Dublin,
CA, USA) was carried out. The corneal endothelial cell density (ECD), which is
to say, the number of cells per square millimeter, was measured using the SP-3000P
specular microscope (Topcon, Oakland, USA).
Postoperative examinations with respect to
IOP, antiglaucoma medication, and complications were carried out for 7
consecutive days as well as at the 1st, 2nd, 3rd,
6th, 9th, and 12th months postoperatively. The
postoperative assessment was similar to that carried out preoperatively, but
with particular attention paid to possible complications and the necessity of
additional procedures or antiglaucoma medication change. In cases of elevated
IOP, digital scleral massage or laser suturelysis was performed. For
encapsulated or flat blebs, needling revision with or without subconjunctival
injection of adjunctives (5-fluorouracyl) was performed.
During the 1st postoperative week,
IOP measurements were taken twice at the same time each day, 9 a.m. and 5 p.m.,
regarding the diurnal variation. During the remainder of the follow-up period,
measurements were taken also at the same time, but between 9 a.m. and 11 a.m.
Long-term IOP fluctuation was defined in terms of the standard deviation (SD)
in IOP values over a given period, with measurements occurring on different
days. Large IOP fluctuation was defined as an IOP SD >3 mm Hg during a given
time. Additionally, the ECD was measured at the postoperative 12th
month, and the percentage loss of ECD relative to the baseline (ECD loss%) was
calculated.
Success was analyzed in two ways: complete
and qualified. Complete surgical success was defined as IOP >5 mm Hg and IOP
<21 mm Hg without use of antiglaucoma medications, without further glaucoma
surgery, and the absence of complications. Qualified success was defined as IOP
>5 mm Hg and IOP <21 mm Hg with a maximum of 2 antiglaucoma medications.
Persistent hypotony, loss of light perception, and reoperation for IOP control
were also defined as failure.
Surgical Procedures All of the
surgical procedures were performed, for consistency, by one experienced surgeon
(Lee KW) using a standardized technique for each surgery type. In both
procedures, a fornix-based conjunctiva flap was created with a relaxing
incision on one side. Next, a 50% thickness limbus-based trapezoidal (3 mm×3
mm) scleral flap was constructed. In the ExPress group, after creation of the
pilot hole using a 26 gauge needle, the filtration device (Ex-PRESS P 50) was implanted
under the scleral flap; in the trabeculectomy group, sclerectomy was performed
under the scleral flap, in the grey limbal zone, and a peripheral iridectomy
was created. During both surgeries, the scleral wound bed was treated for 2min
with 0.02% mitomycin C-soaked sponges. The scleral flap and conjunctiva were
closed with 10/0 nylon sutures. Postoperatively, topical antibiotics and
steroid treatment were administered.
Statistical Analysis IBM SPSS
Statistics ver. 21.0 software (SPSS, Chicago, IL, USA) was used for the
statistical analysis. Data were obtained in the forms of mean±SD and frequency
percentage. The inter-group analysis was performed by Mann-Whitney U
test. For categorical data, the Chi-square and Fisher exact tests were used.
Intra-group differences, obtained from data taken at different time points,
were evaluated using the Wilcoxon signed-rank test. The success rates between
the groups were compared by Kaplan-Meier life table analysis and log rank test.
P values <0.05 were considered to be significant.
RESULTS
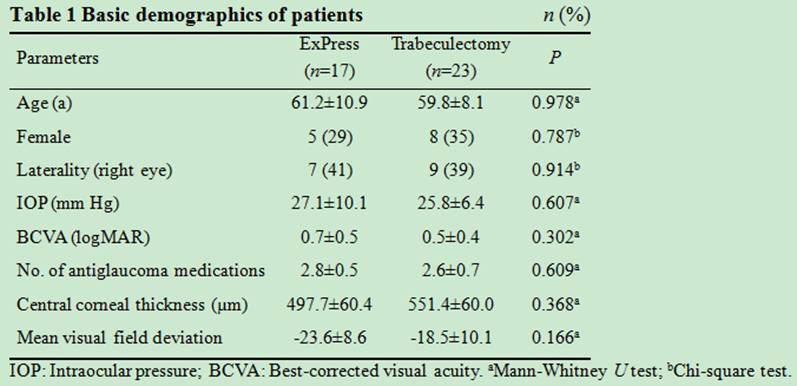
In total, 40 eyes of 40 participants were
enrolled, 17 of which were subject to ExPress glaucoma filtration device
implantation (ExPress) and 23 standard trabeculectomy (Trab). The demographic
data are summarized in Table 1. There were no significant differences in sex,
mean age, visual acuity, glaucoma severity, IOP or number of antiglaucoma
medications between the 2 groups.
Intraocular Pressure Figure 1
shows the mean postoperative IOP in both groups. The mean preoperative IOP in
the ExPress group was 27.1±10.1 mm Hg. After 12mo of follow up, it had
decreased by 55.1%, to 12.1±4.2 mm Hg (P=0.01). Over the same time
period, the mean IOP in the Trab group had decreased by 39.9%, from 25.8±6.4 to
15.5±6.2 mm Hg (P<0.01). Throughout the duration of the study, there
were no statistically significant inter-group differences (P>0.05)
(Table 2).
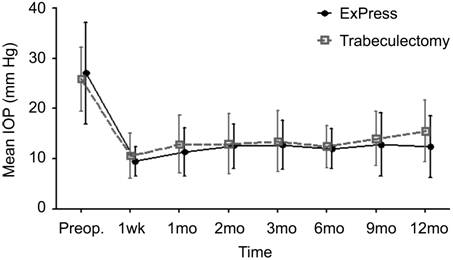
Figure 1 Mean values and standard deviations
of IOP during each follow-up period after ExPress implantation and
trabeculectomy.
Table 2 Comparison of IOP in ExPress
implantation and trabeculectomy groups at specific times postoperatively mm Hg
P value by Mann-Whitney U test.
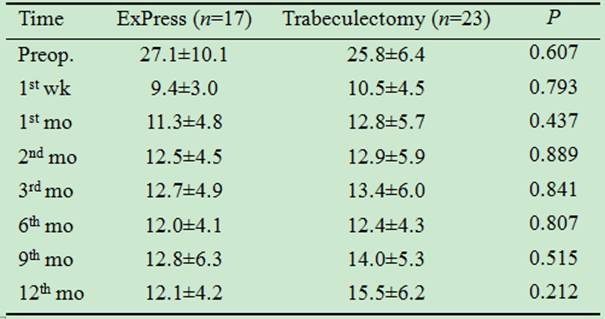
Antiglaucoma Medication Preoperatively,
the average number of antiglaucoma medications was 2.75±0.45 in the ExPress group
and 2.55±0.74 in the Trab group. Over the 12-month evaluation period, the
number of medications in the ExPress group decreased to 0.53±0.80 (P<0.01),
and in the Trab group, to 0.78±1.13 (P<0.01). There were no
statistically significant inter-group differences in the number of medications
at any time pre- or postoperatively (Table 3).
Table 3 Comparison of antiglaucoma medication
amount in ExPress implantation and trabeculectomy groups at specific times
postoperatively
Long-term Intraocular Pressure
Fluctuation The IOP
fluctuation during the 1st week postoperatively was 2.4 mm Hg (SD)
in the ExPress group and 4.2 mm Hg (SD) in the Trab group (P=0.027). The
IOP of the ExPress group was maintained more stably during this 1st
week (Figure 2).
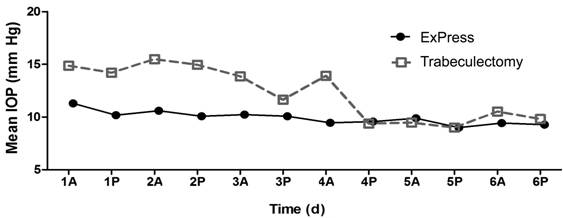
Figure 2 Mean IOP at 1st week
after ExPress implantation and trabeculectomy The IOP was maintained more stably in
the ExPress implantation group. The number indicate the postoperative day, A
indicated the IOP measured at 9 a.m., and P indicated the IOP measured at 5
p.m.
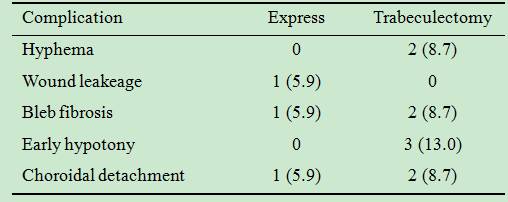
The long-term fluctuations of IOP in the
ExPress and Trab groups are summarized in Table 4. During that 1st week,
2 eyes from the ExPress group (11.8%) and 13 from the Trab group (56.5%) showed
large fluctuation (P=0.009). At 3mo postoperatively, the number of eyes
with large fluctuation in the ExPress group (23.6%) was still lower than that
(56.5%) in the Trab group (P=0.038) (Figure 3).
Table 4 Comparison of long-term IOP
fluctuation (in mm Hg) between ExPress implantation and trabeculectomy groups
during follow-up period

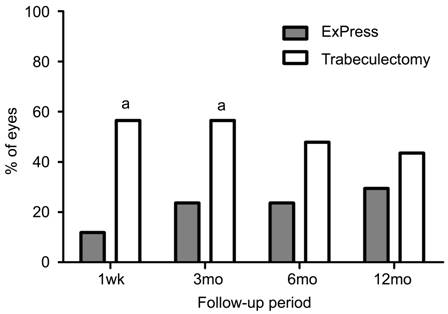
Figure 3 Histogram of eyes with large IOP
fluctuation across 12mo
Large IOP fluctuation was defined as 3 mm Hg or greater. The
trabeculectomy patients were more likely to show large fluctuations during
follow up. aStatistically significant difference between the groups.
Endothelial Cell Count The
preoperative corneal endothelial cell count was 1906.6±605.8 in the ExPress
group and 2186.7±367.9 in the Trab group (P=0.241). After 12mo of follow
up, the number of endothelial cells decreased by 10.0%±7.0% (P=0.139) in
the ExPress group and by 18.2%±13.3% (P=0.021) in the Trab group. That
is, more significant endothelial cell loss was observed in the Trab group (P=0.05,
Table 5).
Table 5 Comparison of corneal ECD in ExPress
implantation and trabeculectomy groups at postoperative 12mo %

Corrected Distance Visual Acuity The
preoperative CDVA was 0.7±0.5 logMAR in the ExPress group and 0.5±0.4 logMAR in
the Trab group (P=0.302). Throughout the entire follow-up period, the
CDVA did not change significantly; by the end of the follow-up period, the scores
were 0.7±0.5 logMAR and 0.5±0.4 logMAR in the ExPress and Trab groups,
respectively (P=0.284).
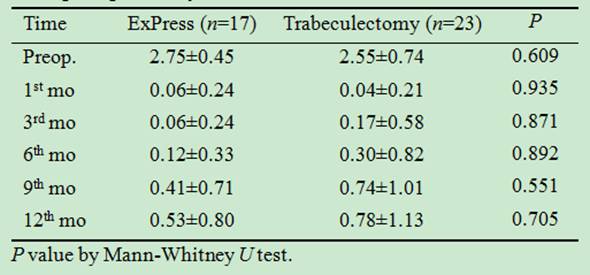
Surgical Success Kaplan-Meier
survival curves of the ExPress and Trab groups are plotted in Figure 4.
Complete success was achieved in 65% and 61% of the patients, respectively (P=0.810),
while qualified success was achieved in 82% and 78% of patients, respectively (P=0.757).

Figure 4 Kaplan-Meier survival curves after
ExPress implantation and trabeculectomy The rates of complete success for the
ExPress and trabeculectomy groups were 82% and 83% at 6mo and 65% and 61% at
12mo, respectively. The differences between the 2 groups’ survival curves were
not statistically significant (P=0.845). Complete success was defined as
5<IOP<21 mm Hg without antiglaucoma medication.
Complications and Additional Procedures Laser
suturelysis was performed in 3 patients from the ExPress group (17.6%) and in 5
patients from the Trab group (21.7%) (P=0.537). There were 1 (5.8%) and
5 (21.7%) bleb needling procedures performed in the ExPress and Trab groups,
respectively. The difference is not statistically significant (P=0.216).
The postoperative complication profiles are
summarized in Table 6. Complications in the ExPress group included wound
leakage (5.9%), bleb fibrosis (5.9%), and choroidal detachment (5.9%). Trab
group patients, meanwhile, experienced complications such as hyphema (8.7%),
bleb fibrosis (8.7%), early hypotony (13.0%), and choroidal detachment (8.7%).
Table 6 Postoperative complications after
ExPress implantation and trabeculectomy n (%)
DISCUSSION
In recent years, several new IOP-lowering
procedures have been developed as alternatives to standard trabeculectomy.
ExPress implantation, for example, is a new means of standardizing
trabeculectomy that shows outcomes quite similar to those of trabeculectomy[6,11].
In the present study, the ExPress group relative
to the Trab group had similar IOP-lowering and success rates but a lower rate
of IOP fluctuation. Throughout the follow-up period, good IOP control was
achieved in both groups. A trend toward lower mean IOP in the ExPress group was
observed, though this did not represent a statistically significant difference
relative to the Trab group. The number of antiglaucoma medications used
postoperatively was not significantly different between the two groups.
Our results are in accordance with those of a
prospective, case control study by Wagschal et al[11].
The rate of complete success was 70% after ExPress implantation compared with
57% after trabeculectomy at the 1y follow-up. There were no differences between
the 2 groups in IOP, success rates, complications or additional intervention.
Dahan et al[12]
reported the results of a prospective comparison between ExPress implantation
and trabeculectomy. As in the present study, both treatment groups demonstrated
significant IOP decrease from the baseline: 44% for the ExPress group, and 48%
for the trabeculectomy group. Unlike our result however, the eyes receiving
ExPress implantation had a significantly higher probability of complete
success. This might be partially explained by their lower, <18 mm Hg IOP
cut-off point.
The statistically significant IOP-fluctuation
difference (to the advantage of the ExPress group) observed in the early
postoperative period in our study is noteworthy. There have been no reports in
the literature on the rate of IOP fluctuation in cases of ExPress implantation
in glaucoma patients. The importance of IOP fluctuation nonetheless was
identified in the pointwise linear regression analysis of AGIS patients
reported by Nouri-Mahdavi et al[13].
Indeed, in their study, IOP fluctuation remained a significant predictor of VF
worsening despite inclusion of mean IOP and number of glaucoma interventions as
independent covariates in their regression models.
As for the present study, although good IOP
control was achieved in both groups, IOP fluctuation was significantly lower
after ExPress implantation in the early postoperative period from week 1 to
month 3. In contrast to trabeculectomy, ExPress implantation does not require
either sclerostomy or peripheral iridectomy. This might reduce the variability
of results among ExPress implantation patients relative to trabeculectomy
cases. This might also reduce postoperative inflammation, which is a very
desirable effect [14]. One possible explanation
for the present result is that the small lumen of the ExPress device provided
additional resistance to aqueous flow during the early postoperative period. In
fact, aqueous flow through that small lumen probably is more constant than that
through the wide sclerectomy of trabeculectomy, even when both apertures are
secured by overlying scleral flaps.
During the immediate postoperative period,
there was a greater need for postoperative manipulation (specifically, laser
suturelysis) in the Trab group than in the ExPress group. The Trab group’s
higher rate of IOP fluctuation during the first week might be associated with
this finding.
In this study, trabeculectomy resulted in a
higher rate of postoperative complications (39%) than ExPress implantation
(17%). Most notably, hyphema and early hypotony were observed only in the Trab
group. These results are in accordance with Dahan and Carmichael’s[15] study, which reported a lower rate of postoperative
complications in the ExPress group (20% vs 33%). These and other such
results are the reason that ExPress implantation has been proposed and promoted
as a less invasive procedure than trabeculectomy, given particularly its lower
rate of complications resulting from postoperative hypotony.
The results of studies on the impact of
trabeculectomy on ECD vary greatly: for example, from 1.6% to 54.8% in
investigations conducted by Smith et al[16].
There have been no reports in the literature on the long-term effects of
ExPress shunt on endothelial cells. In our analysis, the ECD loss % was
significantly higher in the Trab group.
The exact mechanics of endothelial damage by
trabeculectomy are unknown. There are, however, hypotheses, that such damage is
caused by a postoperative inflammatory reaction in the anterior chamber or by
hypoxia directly or indirectly induced by persistent IOP elevation[7,17]. As noted earlier in these
pages, ExPress implantation, in the present study, induced a lower rate of
postoperative IOP fluctuation. ExPress implantation, furthermore, does not
require a large sclerectomy or an iridectomy, which can reduce operative time
and, thus too, postoperative inflammation. These differences might also tend
toward reduced postoperative endothelial cell loss in ExPress compared with
Trab patients.
Another unfavorable factor with respect to
postoperative endothelial damage is the use of antimetabolites and viscoelastics
substances during surgery. Antimetabolites’ corneal endothelial cytotoxicity
has been demonstrated in previous studies[18-19]. Remnant viscoelastic material in the anterior
chamber, meanwhile, can interfere with aqueous outflow, thereby inducing IOP
spikes in the early postoperative period. Anterior chamber collapse during
sclerostomy or peripheral iridectomy also can damage corneal endothelial cells.
The major limitations of our study are its
small sample size (40 eyes) and retrospective design. Notwithstanding, this
small group was sufficient to show statistically significant differences
between the compared procedures, particularly in IOP fluctuation and the rate of
endothelial cell loss. In any case, further studies with longer follow-up
periods and larger numbers of subjects are required.
In summary, ExPress implantation, as compared
with trabeculectomy, is a more predictable and reproducible technique that is less
subject to variability. Especially, it appears to have early-postoperative
advantages such as reduced rates of IOP fluctuation and corneal endothelial
cell loss. ExPress implantation also is an effective treatment in cases of
low-ECD advanced-stage glaucoma for which stable IOP reduction is essential.
ACKNOWLEDGEMENTS
Authors’ Contributions: Lee GY
conceived of the study, and was major contributor in writing the manuscript.
Lee CE participated in its design and coordination and helped to draft the manuscript.
Lee KW conducted the study, and help to collect the data. Seo S made
substantial contributions to analysis and interpretation of data and give final
approval of the version to be published. All authors read and approved the
final manuscript.
Conflicts and Interest: Lee GY, None; Lee
CE, None; Lee KW, None; Seo S, None.
REFERENCES
1 Mosaed S, Minckler DS. Aqueous shunts in
the treatment of glaucoma. Expert Rev Med
Devices 2010;7(5):661-666. [CrossRef] [PubMed]
2 Olayanju JA, Hassan MB, Hodge DO, Khanna
CL. Trabeculectomy-related complications in Olmsted County, Minnesota, 1985
through 2010. JAMA Ophthalmol 2015;133(5):574-580. [CrossRef] [PMC free article] [PubMed]
3 Gedde SJ, Schiffman JC, Feuer WJ,
Herndon LW, Brandt JD, Budenz DL, Tube versus Trabeculectomy Study G. Treatment
outcomes in the Tube Versus Trabeculectomy (TVT) study after five years of
follow-up. Am J Ophthalmol 2012;153(5):789-803.e2. [CrossRef] [PMC free article]
[PubMed]
4 Kerr NM, Wang J, Barton K. Minimally
invasive glaucoma surgery as primary stand-alone surgery for glaucoma. Clin Exp Ophthalmol 2017;45(4):393-400. [CrossRef] [PubMed]
5 Salim S. The role of the Ex-PRESS
glaucoma filtration device in glaucoma surgery. Semin
Ophthalmol
2013;28(3):180-184. [CrossRef]
[PubMed]
6 Shaarawy T, Goldberg I, Fechtner R.
EX-PRESS glaucoma filtration device: review of clinical experience and
comparison with trabeculectomy. Surv
Ophthalmol
2015;60(4):327-345. [CrossRef]
[PubMed]
7 Arnavielle S, Lafontaine PO, Bidot S,
Creuzot-Garcher C, D'Athis P, Bron AM. Corneal endothelial cell changes after
trabeculectomy and deep sclerectomy. J
Glaucoma 2007;16(3):324-328. [CrossRef] [PubMed]
8 Hau S, Barton K. Corneal complications
of glaucoma surgery. Curr Opin Ophthalmol
2009;20(2):131-136. [CrossRef] [PubMed]
9 Francis BA, Singh K, Lin SC, Hodapp E,
Jampel HD, Samples JR, Smith SD. Novel glaucoma procedures: a report by the
American Academy of Ophthalmology. Ophthalmology
2011;118(7):1466-1480. [PubMed]
10 Kalinina Ayuso V, Scheerlinck LM, de
Boer JH. The effect of an Ahmed glaucoma valve implant on corneal endothelial
cell density in children with glaucoma secondary to uveitis. Am J Ophthalmol 2013; 155(3):530-535. [CrossRef] [PubMed]
11 Wagschal LD, Trope GE, Jinapriya D, Jin
YP, Buys YM. Prospective randomized study comparing Ex-PRESS to trabeculectomy:
1-year results. J Glaucoma
2015;24(8):624-629. [CrossRef]
[PubMed]
12 Dahan E, Ben Simon GJ, Lafuma A.
Comparison of trabeculectomy and Ex-PRESS implantation in fellow eyes of the
same patient: a prospective, randomised study. Eye (Lond)
2012;26(5):703-710. [CrossRef]
[PMC free
article] [PubMed]
13 Nouri-Mahdavi K, Hoffman D, Coleman AL,
Liu G, Li G, Gaasterland D, Caprioli J, Advanced Glaucoma Intervention Study.
Predictive factors for glaucomatous visual field progression in the Advanced
Glaucoma Intervention Study. Ophthalmology
2004;111(9):1627-1635. [CrossRef] [PubMed]
14 Ozgonul C, Mumcuoglu T, Gunal A. The
effect of bevacizumab on wound healing modulation in an experimental
trabeculectomy model. Curr Eye Res 2014;39(5):451-459. [CrossRef] [PubMed]
15 Dahan E, Carmichael TR. Implantation of
a miniature glaucoma device under a scleral flap. J Glaucoma 2005;14(2):98-102. [CrossRef] [PubMed]
16 Smith DL, Skuta GL, Lindenmuth KA,
Musch DC, Bergstrom TJ. The effect of glaucoma filtering surgery on corneal
endothelial cell density. Ophthalmic Surg
1991;22(5):251-255. [PubMed]
17 Saheb H, Gedde SJ, Schiffman JC, Feuer
WJ, Tube Versus Trabeculectomy Study G. Outcomes of glaucoma reoperations in
the Tube Versus Trabeculectomy (TVT) Study. Am
J Ophthalmol 2014;157(6):
1179-1189.e2. [CrossRef] [PMC free article] [PubMed]
18 Storr-Paulsen T, Norregaard JC, Ahmed
S, Storr-Paulsen A. Corneal endothelial cell loss after mitomycin C-augmented
trabeculectomy. J Glaucoma
2008;17(8):654-657. [CrossRef] [PubMed]
19 Engin KN, Erdem-Kuruca S, Akgun-Dar K,
Cetin B, Karadenizli S, Gurel E, Yemisci B, Bilgic S, Arslan M. The evaluation
of human tenon’s fibroblasts and endothelial cell responses to antifibrotics
alone and in combination with alpha-tocopherol. Curr Eye Res 2015;40(1):19-29. [CrossRef] [PubMed]
--------------------------------------------------------------------------------------------------------------------------------
All rights reserved by Press of International Journal of Ophthalmology (IJO
PRESS)