IF in JCR CiteScore
Rank About IJO Current
Issue Featured Articles Articles In Press Recent Accepted
 International Journal
of Ophthalmology
International Journal
of Ophthalmology
2017; 10(9): 1392-1395
·Clinical Research·
Long-term outcome of highly myopic foveoschisis
treated by vitrectomy with or without gas tamponade
Li-Na Yun, Yi-Qiao Xing
Department of Ophthalmology, Renmin Hospital
of Wuhan University, Wuhan 430060, Hubei Province, China
Correspondence to: Yi-Qiao
Xing. Department of Ophthalmology, Renmin Hospital of Wuhan University, Wuhan
430060, Hubei Province, China. xing-yiqiao@aliyun.com
Received: 2017-06-06
Accepted: 2017-08-12
Abstract
AIM: To
evaluate the long-term safety and efficacy of vitrectomy and internal limiting
membrane (ILM) peeling with or without gas tamponade for highly myopic
foveoschisis.
METHODS: We
performed an open-label, observer-blinded clinical trial of 85 patients with myopic
foveoschisis between 2000 and 2012. Patients were randomly allocated to one of
two groups, those who received vitrectomy and ILM peeling without gas tamponade
(no-gas group) or those who with gas tamponade (gas group) and follow up at
least 5y.
RESULTS: Visual
acuity of gas group improved from 0.82±0.33 to 0.79±0.73 in 6mo, improved to
0.71±0.67 in 1y and within this range in the following 4y. Visual acuity of
no-gas group improved from 0.81±0.46 to 0.78±0.66 in 6mo, improved to 0.70±0.65
in 1y. The finial visual acuity of two groups were significantly increased
compared with the baseline (P<0.05). The visual acuity was improved
in 35 of 40 eyes (87.5%) in gas group and 29 of 33 eyes (87.9%) in no-gas
group, while there were no significant differences between gas group and no-gas
group in the visual acuity. The foveoschisis on optical coherence tomography
(OCT) completely resolved in 5 of 40 eyes in 1mo, 14 eyes in 6mo and 40 eyes in
1y in the gas group. While the foveoschisis completely resolved in 4 of 33 eyes
in 1mo, 10 eyes in 6mo and 33 eyes in 1y in the no-gas group.
CONCLUSION: Vitrectomy
and ILM peeling without gas tamponade appears to be as effective in the
treatment of myopic foveoschisis as vitrectomy and ILM with gas tamponade.
However, eyes treated with no-gas tamponade showed more rapid resolution of
myopic foveoschisis.
KEYWORDS: myopic foveoschisis; vitrectomy; internal
limiting membrane peeling; gas tamponade
Citation: Yun LN, Xing YQ. Long-term outcome of highly myopic foveoschisis treated
by vitrectomy with or without gas tamponade. Int J Ophthalmol 2017;10(9):1392-1395
INTRODUCTION
Myopic foveoschisis is one of the major
causes of poor vision in highly myopic eyes. Its prevalence has been reported
to range from 8% to 34%[1-2].
Its pathogenesis remains uncertain. Several factors, including vitreous
traction of residual premacular vitreous cortex, rigidity of the internal
limiting membrane (ILM), stiffness of retinal vessels, and posterior
staphyloma, have been suggested to have a role in the development of myopic
foveoschisis[3-6]. In patients
of myopic foveoschisis with foveal detachment, the chances of visual
improvement are 70%-80%, compared with 40% in patients without foveal
detachment[2,7-8].
Reports have mentioned there was possibility of myopic foveoschisis progressed
to a macular hole with the functional improvement further dropped to 30% after
vitrectomy and ILM peeling with gas tamponade[9-10]. Previous study has revealed that vitrectomy and ILM
peeling without gas tamponade is an effective treatment for myopic foveoschisis[3,11]. However, it remains unclear
whether vitrectomy and ILM peeling without gas tamponade was safety and
efficacy with longer follow-up[12]. Thus, the
present study was conducted to evaluate the long-term safety and functional
efficacy of vitrectomy and ILM peeling without gas tamponade in the treatment
of myopic foveoschisis.
SUBJECTS AND METHODS
Study Design This was a
randomized open-labeled, observer-blinded clinical trial of patients with
myopic foveoschisis. The clinical trial protocol and consent form were approved
by the Ethics Committee of the Hospital. We obtained written informed consent
from all patients and/or their first-degree relatives.
Patient Enrollment and Randomization Consecutive
patients were selected from November 2000 to December 2012. Patients between 31
and 75y of age were included in this study only when they met the following
conditions: 1) the diopter was more than -6.00 D or axial length was more than
26.00 mm; 2) best corrected visual acuity (BCVA) less than 0.4 or BCVA was or more
than 0.4 with significant metamorphopsia; 3) foveal detachment with macular
retinoschisis confirmed by optical coherence tomography (OCT).
Patients were excluded when they met the
following conditions: 1) patients with macular hole, choroidal neovascularization,
ablation retinae or peripheral retina hole were detected by OCT; 2) patients
who used to undergo laser photocoagulation surgery on macular region; 3)
incorporated with other retinal disease.
Patients were divided into 2 groups: the gas
group, which underwent vitrectomy and ILM with gas tamponade; the no-gas group,
which underwent vitrectomy and ILM without gas tamponade.
Surgery
All patients signed operation agreement and underwent pars plana
vitrectomy and ILM peeling, with and without gas tamponade[13].
One experienced surgeon performed all operations. Posterior detachment of
vitreous was performed and posterior cortex was completely removed during
surgery. The gas group was performed fluid-air exchange with gas tamponade. The
no-gas group was performed without fluid-air exchange or gas tamponade.
According to the study period and the surgeon’s discretion, the patients was
treated for gas tamponade
Follow-up All patients
were followed for at least 5y and carried out a thorough ocular examination at
baseline, 1, 6mo and each year after surgery. Snellen BCVA test, ocular
tension, slit-lamp biomicroscopy was used for dilated fundus examination,
indirect ophthalmoscope, A-scan ultrasonography or B-scan ultrasonography, eye-ground
photography and OCT were included at each follow-up visit. Main outcome
measures included postoperative BCVA, central foveal thickness (CFT) and the
reattachment of retina in macular region. In this study, we also examined
whether there was any complication, such as subhyaloid hemorrhage or
intraocular hypotension and recorded all the data.
Criterion of Therapeutical Effect 1) The
logarithm of the minimal angle of resolution (logMAR units) converted to
Snellen visual acuity; 2) The change of 0.2 or more logMAR unit was regarded as
the improvement of visual acuity; 3) The change of 0.2 or more logMAR units was
taken for deterioration of visual acuity; 4) The change of logMAR units of less
than 0.2 was considered as the stabilization of visual acuity.
Statistical Analysis The SPSS software (version 20.0 software
for Windows; SPSS, Inc., Chicago, Illinois, USA) was used for statistical
analyses. Preoperative and postoperative clinical parameters were compared
using Mann-Whitney U tests for continuous variables, and using Fisher
exact tests for categorical variables. Wilcoxon signed rank tests were used for
comparisons of visual change within a group[14]. P
values <0.05 were considered to indicate statistical significance.
RESULTS
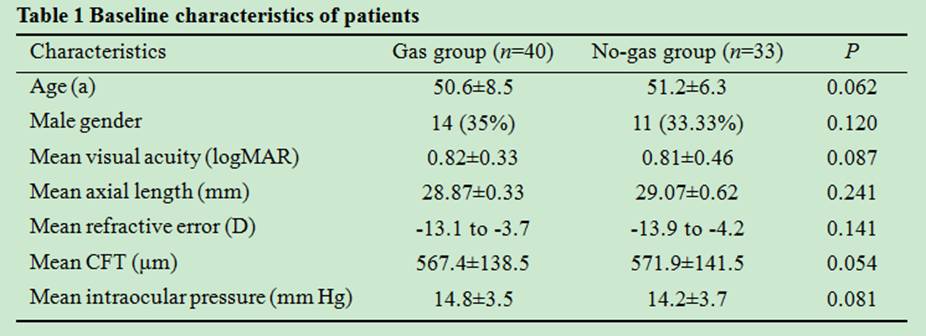
Baseline Characteristics Of 73
patients were finally included in this study at last, the gas group were 40
patients and the no-gas group were 33 patients. For the mean follow-up period
after surgery, the gas group was 5.3y (range 5-6y) and no-gas group was 5.2y
(range 5-6y). Table 1 was the baseline characteristics of two group, the age at
onset, gender, visual acuity, axial length, refractive error, CFT and
intraocular pressure did not differ significantly between two groups.
During the follow-up period, visual acuity of
gas group improved from 0.82±0.33 to 0.79±0.73 in 6mo, improved to 0.71±0.67 in
1y and within this range in the following 4y. Visual acuity of no-gas group
improved from 0.81±0.46 to 0.78±0.66 in 6mo, improved to 0.70±0.65 in 1y and
within this range in the following 4y (Table 2, Figure 1). The finial visual
acuity of two groups were significantly increased compared with the baseline (P<0.05).
The visual acuity was improved in 35 of 40 eyes (87.5%) in gas group and 29 of
33 eyes (87.9%) in no-gas group, remained unchanged in 2 eyes (5%) in gas group
and 3 eyes (9.09%) in no-gas group, and worsened in 3 eyes (7.5%) in gas group
and 1 eye (3.03%) in no-gas group. While there were no significant differences
between gas group and no-gas group in the visual acuity. Foveal reattachment
was attained within 1 to 6mo both in two group. The foveoschisis on OCT completely
resolved in 5 of 40 eyes in 1mo, 14 eyes in 6mo and 40 eyes in 1y in the gas
group. While the foveoschisis completely resolved in 4 of 33 eyes in 1mo, 10
eyes in 6mo and 33 eyes in 1y in the no-gas group.
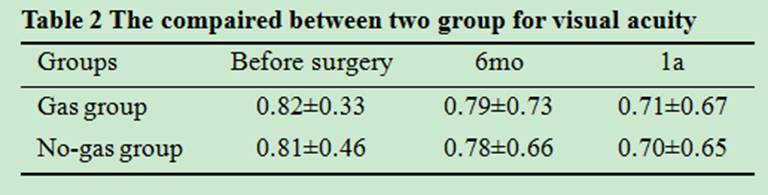

Figure 1 Before and after treatment A: Before treatment; B:
After treatment.
There were no serious complication such as
peripheral retinal break or macular hole occurred during vitrectomy. No retinal
detachment developed during follow-up period.
DISCUSSION
Gas tamponade has been used in the treatment
of myopic foveoschisis, inducing retinal repositioning by pushing the retina
back and keep the retina surface dry[14].
Although the curative effect of gas tamponade was not well knew, gas tamponade
used to be performed in most cases of pars plana vitrectomy[11,15]. Patients with gas tamponade were ordered to maintain
a prone position for at least 1wk[16-17].
The face-down position would be very uncomfortable to many patients[18]. It was assumed that complete release of vitreoretinal
traction is essential and sufficient to restore[19].
In this study, we evaluated the long-term safety and efficacy of vitrectomy and
ILM peeling without tamponade for the treatment of myopic foveoschisis. Our
data demonstrated long-term beneficial effects of vitrectomy without tamponade
in terms of functional outcome[20-21].
Previous reports have mentioned that the retina of patients with myopic
foveoschisis were thinner than normal people, especially with retinal
detachment[10,21]. On the
other side, after removing all traction on the retinal surface, the ILM within
the vascular arcade and staphyloma was peeled with ILM forceps in all eyes to
ensure complete removal of the overlying premacular vitreous cortex and
myofibroblasts on the ILM[22-23].
It could be related to more complete removal of posterior traction, and so such
a selection bias could affect the postoperative result[24-25]. Thus we conjectured that it was no effect of gas
tamponade for prevention macular hole[20,26].
Our results showed the long-term safety and
possible beneficial effects of vitrectomy and ILM peeling without gas
tamponade. ILM peeling without gas tamponade could be the treatment of choice
for myopic foveoschisis without macular hole[21,27]. However, several limitations should be mentioned.
First, owing to the experimental nature of treatment, relatively small numbers of
younger cases were included in this study. Patients know the surgery they
choose and the risk and differences of two surgeries that would influence the
prognosis.
ACKNOWLEDGEMENTS
Conflicts of Interest: Yun LN, None; Xing
YQ, None.
REFERENCES
1 Gohil R, Sivaprasad S, Han LT,
Mathew R, Kiousis G, Yang Y. Myopic foveoschisis: a clinical review.
<ii>Eye (Lond)</ii> 2015;29(5):593-601. [CrossRef]
[PMC free article] [PubMed]
2 Maalej A, Wathek C, Khallouli
A, Rannen R, Gabsi S. Foveoschisis in highly myopic eyes: clinical and
tomographic features. <ii>J Fr Ophtalmol</ii> 2014;37(1):42-46. [CrossRef]
[PubMed]
3 Mii M, Matsuoka M, Matsuyama K,
Otsu Y, Nishimura T. Favorable anatomic and visual outcomes with 25-gauge
vitrectomy for myopic foveoschisis.<ii> Clin Ophthalmol</ii>
2014;8:1837-1844. [CrossRef] [PMC free article] [PubMed]
4 Huang Y, Huang W, Ng DS, Duan
A. Risk factors for development of macular hole retinal detachment after pars
plana vitrectomy for pathologic myopic foveoschisis. <ii>Retina
</ii>2017;37(6):1049-1054. [CrossRef]
[PubMed]
6 Germano RA, Zacharias LC,
Takahashi WY. Recurrent myopic foveoschisis: resolution after internal limiting
membrane removal. <ii>Arq Bras Oftalmol </ii>2015;78(1):44-46. [CrossRef]
[PubMed]
7 Uchida A, Shinoda H, Koto T, Mochimaru
H, Nagai N, Tsubota K, Ozawa Y. Vitrectomy for myopic foveoschisis with
internal limiting membrane peeling and no gas tamponade.
<ii>Retina</ii> 2014;34(3):455-460. [CrossRef]
[PubMed]
8 Lim LS, Ng WY, Wong D, Wong E,
Yeo I, Ang CL, Kim L, Vavvas D, Lee SY. Prognostic factor analysis of
vitrectomy for myopic foveoschisis. <ii>Br J Ophthalmol</ii>
2015;99(12):1639-1643. [CrossRef]
[PubMed]
9 Lai TT, Ho TC, Yang CM.
Spontaneous resolution of foveal detachment in traction maculopathy in high
myopia unrelated to posterior vitreous detachment. <ii>BMC Ophthalmol
</ii>2016;16(1):18-19. [CrossRef]
[PMC free article] [PubMed]
10 Hoang QV, Chen CL,
Garcia-Arumi J, Sherwood PR, Chang S. Radius of curvature changes in
spontaneous improvement of foveoschisis in highly myopic eyes. <ii>Br J
Ophthalmol</ii> 2016;100(2):222-226. [CrossRef]
[PMC free article] [PubMed]
11 Mateo C, Gomez-Resa MV, Bures-Jelstrup
A, Alkabes M. Surgical outcomes of macular buckling techniques for macular
retinoschisis in highly myopic eyes. <ii>Saudi J Ophthalmol</ii>
2013;27(2):235-239. [CrossRef]
[PMC free article] [PubMed]
12 Kim KS, Lee SB, Lee WK.
Vitrectomy and internal limiting membrane peeling with and without gas tamponade
for myopic foveoschisis. <ii>Am J Ophthalmol </ii>
2012;153(1):320-326 . [CrossRef]
[PubMed]
13 Zhang Z, Wei Y, Jiang X, Zhang
S. Pars plana vitrectomy and wide internal limiting membrane peeling with
perfluoropropane tamponade for highly myopic foveoschisis-associated macular
hole. <ii>Retina </ii>2017;37(1): 274-282. [CrossRef]
[PubMed]
14 Wu TY, Yang CH, Yang CM. Gas
tamponade for myopic foveoschisis with foveal detachment. <ii>Graefes
Arch Clin Exp Ophthalmol</ii> 2013;251(6): 1319-1324. [CrossRef]
[PubMed]
15 Fang X, Weng Y, Xu S, Chen Z,
Liu J, Chen B, Wu P, Ni H, Yao K. Optical coherence tomographic characteristics
and surgical outcome of eyes with myopic foveoschisis. <ii>Eye
(Lond)</ii> 2009;23(6):1336-1342. [CrossRef]
[PubMed]
16 Zhang YP, Xue AQ, Wang YQ, Yan
WT, Song ZM. Vitrectomy without internal limiting membrane peeling associated
with gas tamponade for treatment of foveoschisis in pathologic myopia.
<ii>Zhonghua Yan Ke Za Zhi </ii> 2011;47(2):497-503. [PubMed]
17 Chuang LH, Chen YP, Wang
NK, Yeung L, Chen KJ, Hwang YS, Wu WC, Chen TL, Lai CC. Macular hole repair by
vitrectomy and internal limiting membrane peeling in highly myopic
eyes.<ii> Retina </ii> 2014;34(10):2021-2027. [CrossRef]
[PubMed]
18 Sasaki H, Shiono A, Kogo J,
Yomoda R, Munemasa Y, Syoda M, Otake H, Kurihara H, Kitaoka Y, Takagi H.
Inverted internal limiting membrane flap technique as a useful procedure for
macular hole-associated retinal detachment in highly myopic eyes. <ii>Eye
(Lond) </ii>2017;31(4):545-550. [CrossRef]
[PMC free article] [PubMed]
19 Parolini B, Frisina R,
Pinackatt S, Gasparotti R, Gatti E, Baldi A, Penzani R, Lucente A, Semeraro F. Indications
and results of a new L-shaped macular buckle to support a posterior staphyloma
in high myopia. <ii>Retina </ii> 2015;35(12):2469-2482. [CrossRef]
[PubMed]
20 Obata S, Fujikawa M, Iwasaki
K, Kakinoki M, Sawada O, Saishin Y, Kawamura H, Ohji M. Changes in retinal
thickness after vitrectomy for epiretinal membrane with and without internal
limiting membrane peeling. <ii>Ophthalmic Res</ii>
2017;57(2):135-140. [CrossRef] [PubMed]
21 Soiberman U, Shai D,
Loewenstein A, Barak A. Macular hole surgery with internal limiting membrane
peeling facilitated by Membrane-Blue<supsup>®</supsup> versus
Membrane-Blue-Dual<supsup>®</supsup>: a retrospective comparative
study. <ii>J Ophthalmol </ii> 2016;2016:1292735. [CrossRef]
[PMC free article] [PubMed]
22 Philippakis E, Couturier A,
Gaucher D, Gualino V, Massin P, Gaudric A, Tadayoni R. Posterior vitreous detachment
in highly myopic eyes undergoing vitrectomy.<ii> Retina</ii>
2016;36(6):1070-1075. [CrossRef]
[PubMed]
23 Liu B, Ma W, Li Y, Luo Y, Jin
C, Liang X, Sadda SR, Gao Q, Lu L. Macular buckling using a three-armed
silicone capsule for foveoschisis associated with high myopia.<ii>
Retina</ii> 2016;36(10):1919-1926. [CrossRef]
[PubMed]
24 Lichtwitz O, Boissonnot M,
Mercie M, Ingrand P, Leveziel N. Prevalence of macular complications associated
with high myopia by multimodal imaging. <ii>J Fr Ophtalmol</ii>
2016;39(4):355-363. [CrossRef]
[PubMed]
25 Lee CL, Wu WC, Chen KJ, Chiu
LY, Wu KY, Chang YC. Modified internal limiting membrane peeling technique
(maculorrhexis) for myopic foveoschisis surgery. <ii>Acta
Ophthalmol</ii> 2017;95(2):e128-e131. [CrossRef]
[PubMed]
26 Tranos P, Wickham L, Dervenis
N, Vakalis A, Asteriades S, Stavrakas P. The role of membrane-inner retina
adherence in predicting simultaneous internal limiting membrane peeling during
idiopathic epiretinal membrane surgery. <ii>Eye (Lond) </ii>2017;31(4):636-642.
[CrossRef] [PubMed]
27 Chen SN, Yang CM. Lens
capsular flap transplantation in the management of refractory macular hole from
multiple etiologies.<ii> Retina </ii> 2016;36(1):163-170. [CrossRef]
[PubMed]
--------------------------------------------------------------------------------------------------------------------------------
All rights reserved by Press of International Journal of Ophthalmology (IJO
PRESS)